ABSTRACT
Objective: To evaluate the clinical relevance of access targets for elective dental procedures performed under general anesthesia at The Hospital for Sick Children in Toronto, Ontario, by assessing incremental changes in the burden of dental disease over wait times for such procedures.
Methods: Children scheduled for elective dental procedures under general anesthesia were assigned a priority according to the dental diagnosis and the medical risk status. Each priority level was defined by a specific diagnostic code and access target (maximum acceptable wait time). The dental records of children who underwent dental procedures with general anesthesia between June 2005 and December 2008 were assessed retrospectively. A novel assessment scale was used to measure the cumulative burden of dental disease during the waiting period.
Results: A total of 378 children (age range 10 months to 17 years) met the inclusion criteria. Statistically significant correlations were identified between disease burden and wait times for priority group IV (access target 90 days) (p = 0.004), for the entire sample (p < 0.001), for children with advanced dental caries and low medical risk (p = 0.005), for patients with comorbidities (p = 0.036), for healthy patients (p < 0.001), for females (p = 0.014) and for males (p = 0.008). The mean cumulative burden of disease over time did not differ between matched groups with and without comorbidity (p = 0.38).
Conclusions: A trend suggestive of increasing burden of dental disease for children with longer wait times for elective dental procedures involving general anesthesia was found, but it was not clinically significant. Refinements in the assessment scale and a better understanding of the natural history of dental disease will likely be useful in developing clinically relevant access targets.
Introduction
Dental treatment under general anesthesia is often indicated for children with complex medical conditions, those who are uncooperative during dental care and those with extensive dental needs.1 Hospitals providing dental care under general anesthesia, including the authors’ institution, have reported wait times of 40 to 60 weeks2 from consultation to treatment. These waits are longer than the wait times for either ophthalmic services (10.6 weeks) or otolaryngologic services (11.7 weeks) performed under general anesthesia.3
The wait-time literature for pediatric dentistry has focused on the consequences of delays in dental treatment.4,5 To the authors’ knowledge, only one paper has described the use of a prioritized scheduling system for elective dental treatment of children under general anesthesia.6
Prioritization System at The Hospital for Sick Children
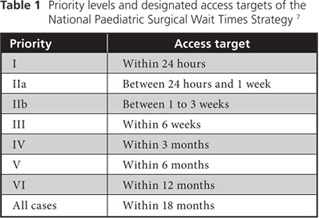
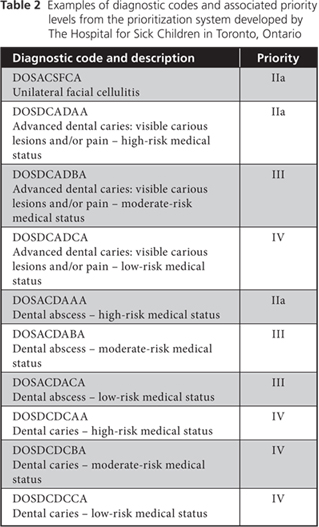
The Canadian Child and Youth Health Coalition developed a 7-level system in 2005 to prioritize children for elective surgery in Canada7 (Table 1). The Dental Department of The Hospital for Sick Children (SickKids) in Toronto, Ontario, created a complementary system that used 9-letter diagnostic codes to describe a child’s medical and dental status (e.g., DOSACDACA = dental abscess, low medical risk) (Table 2). A diagnostic code was assigned to each child at the time of the decision to treat, when the child or the parent or guardian consented to dental treatment under general anesthesia. Each diagnostic code was linked to a priority level and associated access target (maximum acceptable wait time). Each access target was based on the anticipated effect of the dental diagnosis on any existing medical comorbidity. Pediatric surgical access targets in Canada, including the National Paediatric Surgical Wait Times Strategy7 and the scheme used at SickKids, have been based on consensus and have been implemented at pediatric hospitals to aid in the prioritization of children for surgery.
The objective of the study reported here was to determine the clinical relevance of prescribed access targets for elective dental treatment performed under general anesthesia at SickKids by assessing incremental changes in the burden of dental disease over the waiting time for dental treatment. The clinical relevance of the current wait-time model was evaluated according to whether the disease burden increased significantly during the time elapsed from consultation to treatment.
Methods
Selection of Patient Records
A password-protected database (FileMaker Pro, version 8.5.1; FileMaker, Inc., Santa Clara, CA) was designed to hold wait-time data for patients (aged 0 to 17 years) scheduled for elective dental treatment from June 2005 onward. One investigator (SSC) conducted a retrospective analysis of patient records from the database and hand-searched dental charts to assess eligibility for inclusion.
The inclusion criteria were as follows:
- planned elective dental treatment under general anesthesia
- date of decision to treat between June 2005 and December 2008
- preoperative dental assessment completed and verified for accuracy by a staff pediatric dentist
- report of dental treatment completed on the day of the general anesthesia
The Research Ethics Board at SickKids granted approval (REB approval no. 1000012706) for this investigation.
Data Collection
A spreadsheet was used to organize the data from the records of eligible patients. To anonymize the patients’ data, identification numbers were used in place of patient identifiers. The wait time for each child was the number of days elapsed from the decision to treat until the date of general anesthesia. The number of days waiting beyond the access target was the difference between the actual wait time and the prescribed access target for the child’s assigned diagnostic code. The change in the burden of disease over the wait time for each child was scored with a novel assessment scale, described below.
Assessment Scale
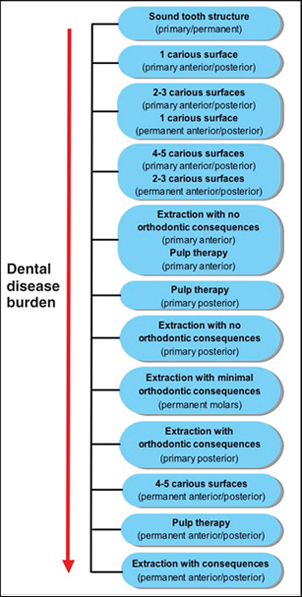 Figure 1: Scale used to score changes in the burden of dental disease. The red arrow indicates increasing severity of the burden of disease. The change in burden of disease for individual teeth is described as a positive, negative or zero integer.
Figure 1: Scale used to score changes in the burden of dental disease. The red arrow indicates increasing severity of the burden of disease. The change in burden of disease for individual teeth is described as a positive, negative or zero integer.
Five staff pediatric dentists from SickKids held 2 expert panel meetings, in November and December 2008, to develop a consensus-based assessment scale. The ordinal scale identified the increasing burden of disease associated with various conditions of the primary and permanent dentition (Fig. 1).
The expert panel ranked the burden of disease according to the treatment required and the anticipated treatment outcomes. The end points of the scale were sound tooth structure (least severe burden of disease) and extractions of one or more permanent teeth producing functional and/or esthetic and/or orthodontic consequences (most severe burden of disease). With this scale, the change in burden of disease for individual teeth is described as a positive, negative or zero integer. A positive score represents an increase in the disease burden over time (e.g., progression of a 2-surface carious lesion on a primary anterior tooth at the time of decision to treat to pulp therapy at the time of treatment would yield a score of +2). A negative score represents a decrease in the disease burden between the decision to treat and treatment (e.g., if a primary posterior tooth was deemed to need pulp therapy at the time of decision to treat, but a 2-surface restoration was performed at the time of dental general anesthesia, the score would be –3). A zero score represents comparable levels of disease burden at the time of decision to treat and the treatment date and was assessed as no change in the child’s overall disease burden.
With this assessment scale, scores for burden of disease ranged from –12 to +12 for each tooth, representing the number of levels of disease burden over which a tooth could advance over time, but not the magnitude of change between levels. For example, if restoration of a primary maxillary incisor was planned at the time of decision to treat, but additional treatment was actually performed (e.g., the planned restoration plus pulp therapy), the disease burden was deemed to have increased during the wait time, but the magnitude of the increase was unknown. The total score for each child was the sum of the scores for all existing teeth. Orthodontic extractions and teeth that exfoliated during the wait for treatment were excluded from the calculation. In addition, the primary mandibular incisors were excluded from the calculation because the treatment philosophy for incipient decay of these teeth was variable at the study hospital, some dentists favouring enameloplasty and others favouring extraction. The decision to exclude the primary mandibular incisors reflected the potential for divergent scoring because of limited treatment options and limited levels of disease burden for these teeth.
Statistical Analysis
For the purpose of analysis, the sample was divided into subgroups by priority level, diagnostic code, medical status (with or without comorbid conditions) and sex. Observations were represented graphically on scatter plots, and best-fit trend lines were calculated by linear regression. These regression analyses were completed on the larger subsets of the sample (i.e., priority groups III and IV; diagnostic codes DOSDCADCA and DOSDCADBA), which were deemed representative of children treated at SickKids. The correlation between the number of days waiting beyond the access target (the independent variable) and the total score or change in disease burden (the dependent variable) was evaluated with Pearson’s correlation coefficient (r). To assess for differences between the groups with and without comorbid conditions, pairs of patients matched by age (in months), sex and priority code were selected from the 2 groups, and a paired-samples t test was performed.
SAS software (version 9.1; SAS Institute Inc., Cary, NC) was used for statistical analysis. A p value of 0.05 or less was considered statistically significant. A descriptive summary was completed for study patients seen on an emergency basis at SickKids during the observed wait time.
Results
The dental records of 378 children (179 female, 199 male, ranging in age from 10 months to 17 years) seen for consultation between June 2005 and December 2008 were included in the analysis. The mean age (± standard deviation) at the time of the decision to treat was 4.95 ± 3.68 years. Two hundred and eighty-eight (76.2%) of the children had comorbid conditions. The 2 largest subsets by priority status, priority III (access target 42 days) and priority IV (access target 90 days), accounted for 100 (26.5%) and 266 (70.4%) of the bookings, respectively (Table 3). The mean number of days waiting beyond the access targets was 122 ± 125 days. Thirty-seven (9.8%) of the children were seen on an emergency basis for dental pain (28/37), swelling (6/37), trauma (2/37) or exfoliating teeth (1/37) during their wait for dental treatment under general anesthesia. Three hundred (79.4%) of the patients were not treated within their assigned access targets.
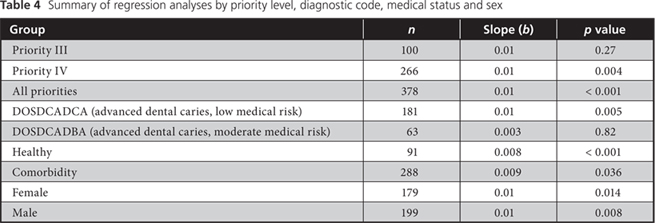
In the regression analysis by priority group, there was a small positive correlation between change in burden of disease and waiting time for the priority III group, but it was not statistically significant (Fig. 2). In contrast, the correlations for the priority IV group and the entire sample were statistically significant (Fig. 2).
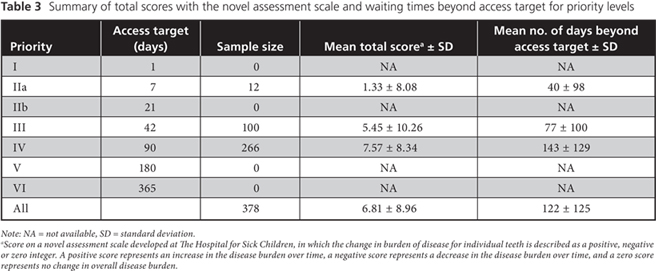
 Figure 2: Correlation between burden of disease and excess waiting time for (a) priority III group (target access time 6 weeks), priority IV group (target access time 6 months) and (b) the entire group. For the priority III group, r = 0.112 (p = 0.27). For the priority IV group, r = 0.176 (p = 0.004). For the entire group, Pearson’s r = 0.184 (p < 0.001).
Figure 2: Correlation between burden of disease and excess waiting time for (a) priority III group (target access time 6 weeks), priority IV group (target access time 6 months) and (b) the entire group. For the priority III group, r = 0.112 (p = 0.27). For the priority IV group, r = 0.176 (p = 0.004). For the entire group, Pearson’s r = 0.184 (p < 0.001).
The data set was also organized by diagnostic code, medical status and sex. In terms of diagnostic codes, the 2 largest groups consisted of cases of advanced visible carious lesions with low medical risk, the DOSDCADCA group, and moderate medical risk, the DOSDCADBA group. For both of these groups, the correlation was small and positive, but it was statistically significant only for the DOSDCADCA group (Fig. 3). For patients with and without comorbid conditions, the correlations were small and statistically significant (Fig. 4). The correlations by sex were similar in magnitude and statistically significant (Fig. 5). However, the difference in mean total score between sexes was not statistically significant (t = –1.11, df = 376, p = 0.27).
Regression analyses by subgroup produced slopes that approximated a zero value (b ≤ 0.01). This indicated that large increases in the number of days waiting beyond the access target were associated with small increments in the burden of disease (Table 4).
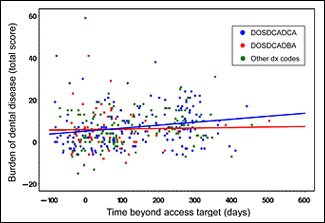 Figure 3: Correlation between burden of disease and excess waiting time for the groups with diagnostic codes DOSDCADCA and DOSDCADBA. For the DOSDCADCA group (advanced dental caries, low medical risk), Pearson’s r = 0.210 (p = 0.005). For the DOSDCADBA group (advanced dental caries, moderate medical risk), Pearson’s r = 0.030 (p = 0.82).
Figure 3: Correlation between burden of disease and excess waiting time for the groups with diagnostic codes DOSDCADCA and DOSDCADBA. For the DOSDCADCA group (advanced dental caries, low medical risk), Pearson’s r = 0.210 (p = 0.005). For the DOSDCADBA group (advanced dental caries, moderate medical risk), Pearson’s r = 0.030 (p = 0.82).
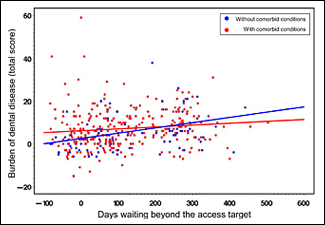 Figure 4: Correlation between burden of disease and excess waiting time by medical status. For patients without comorbid conditions, Pearson’s r = 0.387 (p < 0.001). For patients with comorbid conditions, Pearson’s r = 0.124 (p = 0.036).
Figure 4: Correlation between burden of disease and excess waiting time by medical status. For patients without comorbid conditions, Pearson’s r = 0.387 (p < 0.001). For patients with comorbid conditions, Pearson’s r = 0.124 (p = 0.036).
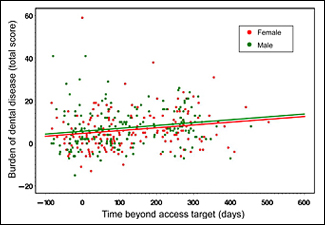 Figure 5: Correlation between burden of disease and excess waiting time by sex. For females, Pearson’s r = 0.183 (p = 0.014). For males, Pearson’s r = 0.188 (p = 0.008).
Figure 5: Correlation between burden of disease and excess waiting time by sex. For females, Pearson’s r = 0.183 (p = 0.014). For males, Pearson’s r = 0.188 (p = 0.008).
Forty-three pairs of patients matched by age, sex and priority code were identified from the groups with and without comorbid conditions. The mean total change in disease burden was similar for the groups with comorbid conditions (4.72 ± 8.35) and without comorbid conditions (6.30 ± 8.17); this difference was not statistically significant (t = 0.89, df = 42, p = 0.38).
Discussion
To the authors’ knowledge, this investigation was the first to study access targets for elective procedures requiring general anesthesia in pediatric dentistry. Notably, most of the patients (79.4%) did not undergo the necessary procedure within the defined access target. Long wait times resulted in emergency visits for 37 (9.8%) of the children, with dental pain being the most common complaint (28/37). These results are similar to those obtained by Lush and Roebuck4 and North and colleagues.5
The access targets employed in this study were based on consensus and were used by all surgical services with operating room time. Because the access targets were not specific to particular dental diseases, it was important to determine whether their use would result in children receiving dental treatment before their condition worsened appreciably. Given this model, the prescribed access targets would be considered clinically relevant if children’s dental burden of disease did not increase over wait times that approximated the access targets. The major assumption of this study was that severity of dental disease would increase between the date of the decision to treat and the treatment date. However, this assumption was not supported by the data. Regression analyses showed small increases in the severity of dental disease over time for this sample, but these changes were not clinically significant, as the slopes approximated zero (b ≤ 0.01). The most likely explanation for this finding is that by the time of a decision to treat at SickKids, patients’ dental disease burden approximated maximal severity for their respective conditions.
Although the SickKids prioritization system showed good face validity,6 the clinical relevance of the access targets could not be demonstrated because of the very small increase in dental disease burden between the dates of consultation and treatment. It is possible that the correlation between change in dental disease burden and wait times was obscured by factors such as the dental priority criteria, the assessment scale, the accuracy of treatment planning on the date of decision to treat and/or the dental disease state.
In this study, patients were prioritized according to only 2 criteria: dental diagnosis and medical risk. Given that these 2 criteria were already being assessed for children who needed to undergo a dental procedure requiring general anesthesia, this system was clinically efficient. However, the simplicity of the prioritization system might have prevented consideration of important clinical and nonclinical factors, such as dental age and oral health-related quality of life. Dental age may be inversely related to the urgency of the need for treatment of dentin caries, as the pulp to crown ratio is greater and the risk of abscess before treatment potentially greater in younger than in older children. Similarly, a child’s quality of life may be adversely affected by pulpal pain from untreated caries that impairs the activities of daily living. A decrease in a child’s oral health-related quality of life may indicate a higher priority for dental treatment.
Existing measures of dental disease burden, such as the decayed, missing and filled (DMF) index of Klein and Palmer,8 were deemed inadequate to describe gradations in the severity of progressive dental disease. The lack of available alternatives led to the development of a novel assessment scale based on expert consensus. This assessment scale was used to measure the change in disease burden for each tooth during the wait time, but it did not allow quantification of the magnitude of change between levels of disease burden. Future studies could use a visual analogue or Likert-type scale, with ratings by caregivers, patients or pediatric dentists, to discern differences between successive levels of dental disease, similar to prioritization studies in medicine.9-13
Clinical examination and radiography may have been limited by patient cooperation on the date of decision to treat, with cooperation being affected by age or comorbid conditions. These factors might have affected diagnosis of the quantity and severity of caries at the time of decision to treat, which might in turn have affected the accuracy of scoring. Despite this limitation, it was felt that the disease burden scores were not adversely affected, given the large sample size and the extensive clinical experience of staff pediatric dentists. Scoring might also have been affected by previous treatment planning practices. In the past, staff pediatric dentists at SickKids planned treatment in anticipation of caries progression during longer waits for dental procedures requiring general anesthesia; this approach ensured that families were aware of potential costs and aided in the allocation of operating room time. For this study, however, the staff pediatric dentists were instructed to plan treatment as if the child were to be treated on the day that the decision to treat was made. The previous system of treatment planning, with allowance for disease progression, may have biased the data.
It is possible that the change in disease burden was minimal during the wait for treatment, because SickKids is a tertiary care centre and often the final point of care for children with dental needs. Consequently, in many instances, the dental disease was so advanced at the time of decision to treat that only minimal progression was possible. Most of the disease progression likely occurred during the wait for consultation with the patient’s primary community-based dental provider, which would often be followed by referral to a pediatric dentist and finally referral to the hospital. Therefore, disease progression would more likely be documented if prioritization occurred much earlier in the caries process. The results from this study may be comparable only with those obtained in other pediatric tertiary care hospitals.
Conclusions
To the authors’ knowledge, this investigation was the first to evaluate the clinical relevance of access targets in pediatric dentistry, and this institution was also the first to devise a novel assessment scale of dental disease accounting for both severity and progression. The increase in the burden of dental disease beyond the access targets was minimal, as patients presented with advanced dental disease on the date of decision to treat. Because most of the disease progression occurred before consultation, the current model for access targets for general anesthesia in pediatric dentistry may be more relevant in community-based settings than at tertiary care centres. Despite the limitations of this study, a trend of increasing burden of dental disease in children was associated with prolonged wait times for elective dental treatment under general anesthesia. Further assessment of the access targets in use at SickKids may benefit from refinements of the disease burden scale and a better understanding of the natural history of dental disease.
THE AUTHORS
References
- American Academy of Pediatric Dentistry. Guideline on behavior guidance for the pediatric dental patient. Pediatr Dent. 2006–2007. 28(7 Suppl):97-105.
- Park MS, Sigal MJ. The role of hospital-based dentistry in providing treatment for persons with developmental delay. J Can Dent Assoc. 2008;74(4):353-7.
- Esmail N, Walker MA. Waiting your turn: hospital waiting lists in Canada. 16th ed. Vancouver: The Fraser Institute; 2006.
- Lush N, Roebuck EM. Adverse experiences while waiting for treatment under paediatric general anaesthetic. Int J Paediatr Dent. 2006;16(Suppl 1):11 [Abstract P24].
- North S, Davidson LE, Blinkhorn AS, Mackie IC. The effects of a long wait for children’s dental general anaesthesia. Int J Paediatr Dent. 2007;17(2):105-9.
- Casas MJ, Kenny DJ, Barrett EJ, Brown L. Prioritization for elective dental treatment under general anesthesia. J Can Dent Assoc. 2007;73(4):321. Available: www.cda-adc.ca/jcda/vol-73/issue-4/321.html.
- Canadian Child and Youth Health Coalition. “Children Wait Too”: National Paediatric Surgical Wait Times Strategy. Final Report. Ottawa: CCYHC; April 2006. Available: www.ccyhc.org/docs_indicators/surgical_wait_times/strategy_final_report_042006.pdf (accessed 2010 Oct 6).
- Klein H, Palmer C. Studies on dental caries. V. Familial resemblance in the caries experience of siblings. Public Health Rep. 1938;53:1353-64.
- Allepuz A, Espallargues M, Moharra M, Comas M, Pons JM; Research Group on Support Instruments – IRYSS Network. Prioritisation of patients on waiting lists for hip and knee arthroplasties and cataract surgery: instruments validation. BMC Health Serv Res. 2008;8:76.
- Conner-Spady BL, Arnett G, McGurran JJ, Noseworthy TW; Steering Committee of the Western Canada Waiting List Project. Prioritization of patients on scheduled waiting lists: validation of a scoring system for hip and knee arthroplasty. Can J Surg. 2004;47(1):39-46.
- Conner-Spady B, Estey A, Arnett G, Ness K, McGurran J, Bear R, Noseworthy T; Steering Committee of the Western Canada Waiting List Project. Prioritization of patients on waiting lists for hip and knee replacement: validation of a priority criteria tool. Int J Technol Assess Health Care. 2004;20(4):509-15.
- Conner-Spady BL, Sanmugasunderam S, Courtright P, Mildon D, McGurran JJ, Noseworthy TW; Steering Committee of the Western Canada Waiting List Project. The prioritization of patients on waiting lists for cataract surgery: validation of the Western Canada waiting list project cataract priority criteria tool. Ophthalmic Epidemiol. 2005;12(2):81-90.
- Escobar A, González M, Quintana JM, Bilbao A, Ibañez B. Validation of a prioritization tool for patients on the waiting list for total hip and knee replacements. J Eval Clin Pract. 2009;15(1):97-102.
