Red or Red-White Oral Lesions
- Common causes of mucosal redness (erythema) include:
- Vasodilation: increased blood vessel diameter commonly occurring with inflammation, but also possible with neoplasia
- Vascular proliferation: increased number of blood vessels due to release of growth factors, such as vascular endothelial growth factor (VEGF), during inflammation and as part of neoplasia
- Leaky blood vessels (bleeding into tissue): due to trauma, occasionally due to an immune response
- Epithelial thinning (atrophy and/or reduced epithelial keratinization): due to abnormal cell turnover during normal healing, in response to trauma, or as part of dysplasia
- A mixture of red and white lesions suggests an irregular epithelial surface that may be caused by a variety of processes, including chronic trauma, inflammation and neoplasia.
Presentation
Population
Any age, but more common in adults
Signs
- Signs of potential precancerous or malignant processes include:
- Colour: homogeneous red (erythroplakia) or mixed red and white (erythroleukoplakia); may appear lacy
- Surface anatomy: flat, elevated, mass, ulceration
- Surface texture: smooth, velvety, verrucous or ulcerated
- Consistency: indurated or non-indurated
- Tissue fragility
- Paresthesia, numbness, discomfort, sensitivity to spicy/acidic foods
- Nonhealing ulcer present for more than 2 weeks
- Highest intraoral risk sites for neoplasia are lateral and ventral surfaces of the tongue, floor of mouth and retromolar area. Waldeyer tonsillar ring (tonsils, base of tongue) at increased risk.
- Location: single site, multiple sites, bilateral or unilateral presentation. Malignancies are less commonly bilateral.
- See Figures 1–9 for different manifestations of red or red-white oral lesions.
 Figure 1: Asymptomatic fissured homogenous leukoplakia without erythema, representing classical lesion associated with smokeless tobacco use. Histopathology: benign, hyperkeratosis and acanthosis.
Figure 1: Asymptomatic fissured homogenous leukoplakia without erythema, representing classical lesion associated with smokeless tobacco use. Histopathology: benign, hyperkeratosis and acanthosis.
 Figure 2: Asymptomatic homogenous leukoplakia without induration and erythema, etiology unknown. Histopathology: benign, severe hyperakatosis and acanthosis.
Figure 2: Asymptomatic homogenous leukoplakia without induration and erythema, etiology unknown. Histopathology: benign, severe hyperakatosis and acanthosis.
 Figure 3: Mild local sensitivity associated with leukoplakia in area of diffuse erythema, and adjacent involvement of the gingiva by erythema and lacy changes. Histopathology: benign, epithelial hyperkeratosis and alternating atrophy, with linear lymphocytic infiltration consistent with lichen planus.
Figure 3: Mild local sensitivity associated with leukoplakia in area of diffuse erythema, and adjacent involvement of the gingiva by erythema and lacy changes. Histopathology: benign, epithelial hyperkeratosis and alternating atrophy, with linear lymphocytic infiltration consistent with lichen planus.
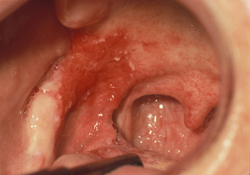 Figure 4: Asymptomatic, intense unilateral area of erythroplakia, “velvety” surface and minor leukoplakia. Histopathology: Severe dysplasia, vascular dilation, intact basement membrane.
Figure 4: Asymptomatic, intense unilateral area of erythroplakia, “velvety” surface and minor leukoplakia. Histopathology: Severe dysplasia, vascular dilation, intact basement membrane.
 Figure 5: Asymptomatic, mixed unilateral red and white lesion with elevation and verrucous changes in the anterior portion of the lesion and more posterior erythroplakia. Histopathology: white lesion: verrucous change with moderate dysplasia; red portion: squamous cell carcinoma.
Figure 5: Asymptomatic, mixed unilateral red and white lesion with elevation and verrucous changes in the anterior portion of the lesion and more posterior erythroplakia. Histopathology: white lesion: verrucous change with moderate dysplasia; red portion: squamous cell carcinoma.
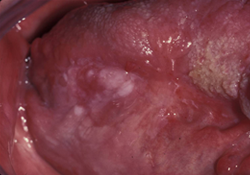 Figure 6: Patient with prior cancer in the tongue, presenting with mild discomfort of recent onset in the area of prior cancer, where leukoplakia is seen in an area of erythema. Histopathology: white area: squamous cell carcinoma; red area: epithelial atrophy, benign epithelium.
Figure 6: Patient with prior cancer in the tongue, presenting with mild discomfort of recent onset in the area of prior cancer, where leukoplakia is seen in an area of erythema. Histopathology: white area: squamous cell carcinoma; red area: epithelial atrophy, benign epithelium.
 Figure 7: Asymptomatic red/white lesion, mass with palpable firmness. Histopathology: squamous cell carcinoma.
Figure 7: Asymptomatic red/white lesion, mass with palpable firmness. Histopathology: squamous cell carcinoma.
 Figure 8: Discomfort and numbness/tingling in the tongue with thickening and mass effect and irregular surface with ulceration. Histopathology: squamous cell carcinoma.
Figure 8: Discomfort and numbness/tingling in the tongue with thickening and mass effect and irregular surface with ulceration. Histopathology: squamous cell carcinoma.
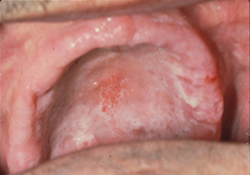 Figure 9: Mild discomfort under upper denture. Some of the white changes will wipe off with gauze, subjacent erythema. Histopathology: mucosal atrophy with areas of hyperplasia, and positive stain for Candida species.
Figure 9: Mild discomfort under upper denture. Some of the white changes will wipe off with gauze, subjacent erythema. Histopathology: mucosal atrophy with areas of hyperplasia, and positive stain for Candida species.
Symptoms
- Pain severity is variable in potential precancerous or malignant lesions: there may be no pain, some discomfort, aching or spontaneous stabbing pain.
- Throbbing pain or sensitivity to touch suggests possible underlying inflammation.
- Burning, stabbing sensation: suggests possible neural involvement and in combination with red or red-white lesions, malignancy must be considered.
Investigation
Rule Out Local Pathology
- Obtain a thorough medical and dental history.
- Inquire about any prescription drugs taken by patient (type, dosage, frequency, duration), tobacco use, alcohol abuse, illicit or street drug use, unsafe sexual activity, HPV vaccination status.
- Inquire about the history of the lesions: onset, duration and progression over time.
- Short-term duration: suggests a variety of etiologies, such as trauma, infection, environmental factors, allergy or autoimmune response.
- Medium-term duration: suggests neoplasm (benign or malignant), immune response or metabolic abnormality.
- Long-term duration: suggests developmental condition or benign neoplasm. However, if longstanding lesion suddenly changes, malignant progression should be considered.
- Perform thorough clinical head and neck, oral and dental examination. Evaluate for cranial nerve function, palpable lymph nodes, masses and tenderness.
- Look for characteristics of neoplastic lesions: unilateral, red and/or mixed red-white lesions, with or without induration and/or ulceration. Record size and location.
- Assess patient for signs of infection, including pain, swelling, lymphadenopathy, fever, etc.
- Inquire about recent and/or chronic trauma to area in question.
- Rule out other causes of local or systemic pathology, including allergy, immune inflammation and immunodeficiency state, anemia.
Diagnosis
- Based on the patient’s medical history, clinical findings and results from diagnostic procedures, a diagnosis of red or red-white oral lesions is determined.
- Diagnosis may require adjunctive clinical tests, biopsies with routine and sometimes immunofluorescent analysis, and management by a dental or medical specialist.
Differential Diagnosis
- Developmental: vascular malformation, geographic tongue
- Immune mediated: lichenoid mucositis, lupus, drug reaction, hypersensitivity reactions
- Metabolic: anemia
- Infection: candidiasis, syphilis, gonorrhea
- Trauma: mechanical, chemical, thermal irritation
- Neoplasia: dysplasia, squamous cell carcinoma, soft tissue neoplasms, lymphoma, leukemia
Treatment
Common Initial Treatments
Treatment depends on diagnosis and often requires expert care and continuing follow-up:
- Dysplastic lesions: repeated biopsies may be needed. Current treatments include elimination of risk behaviours, such as smoking; treatment of inflammation; medical therapies and/or excision. Close follow-up is mandatory. Targeted therapies and chemoprevention are under investigation.
- Squamous cell carcinoma: surgery, chemotherapy, radiotherapy and targeted therapy depending on stage of disease and site.
Advice
- If lesions are suspicious for malignancy: refer to a specialist with experience in mucosal disease and oncology, such as specialists in oral medicine, pathology, surgery, otorhinolaryngology or oncology.
- May require biopsy with appropriate biopsy site selection, careful technique, special tissue stains and submission to pathologist experienced in oral mucosal disease. If the pathology report is not consistent with history and clinical presentation of the lesion, consider repeating pathologic review, repeat biopsy or refer.
- Preneoplastic lesions may evolve over time, so repeated biopsies may be needed during follow-up.
- Treatment is variable and largely dependent on diagnosis.
THE AUTHORS
Suggested Resources
- Kerr AR, Lederman DA, Ephros, editors. Clinician’s guide to diagnosis of oral cancer and potentially malignant oral lesions. Edmonds (WA): American Academy of Oral Medicine; 2010.
- Rethman MP, Carpenter W, Cohen EE, Epstein J, Evans CA, Flaitz CM, et al. Evidence-based clinical recommendations regarding screening for oral squamous cell carcinomas. J Am Dent Assoc. 2010;141(5):509-20.
- Scully C, Felix DH. Oral Medicine–update for the dental practitioner: red and pigmented lesions. Br Dent J. 2005;199(10):639-45.
- Seigel MA, Silverman S Jr, Sollecito TP, editors. Clinician’s guide to treatment of common oral conditions. 7th ed. Edmonds (WA): American Academy of Oral Medicine; 2009.


