Body
Oral Ulcers
Oral ulcers are a common clinical problem in the pediatric population. Generally, an ulcer is defined as a well-circumscribed lesion with an epithelial defect covered by a fibrin clot (a pseudomembrane), giving the ulcer a yellow-white appearance.
Presentation
Population
- Any segment of the pediatric population, from infancy through adolescence
- Children of parents with recurrent oral ulcers due to genetic predisposition (i.e., recurrent aphthous stomatitis)
- Young children in group settings (e.g., daycare, shared play areas) developing oral ulcers secondary to an infectious (i.e., bacterial and/or viral) etiology due to the increased risk of oral fluid transfer in those settings
Signs
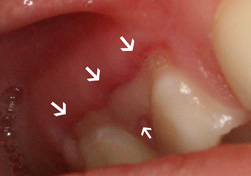
- Well-circumscribed lesions, often depressed, with an epithelial defect covered by a yellow-white pseudomembrane (Fig. 1)
- Single or multiple ulcers; may present in clusters (herpetiform)
- Intraoral/perioral location: nonkeratinized and/or keratinized oral mucosa, oropharynx, lips, perioral skin
- Variable size (most commonly measured in millimetres, but may be larger)
- General location: oral/perioral lesion(s) only or with involvement of other affected surfaces (i.e., skin, genitals, other mucous membranes)
NOTE: Click to enlarge figure.
Symptoms
- Pain severity: Can range from asymptomatic to severe discomfort
- Burning
- Irritation
- Pruritis (itching sensation)
- Systemic symptoms, such as fever, malaise, lymphadenopathy, difficulty swallowing and general irritability
Investigation
- Ask the parent or patient (if the patient is old enough), about the history of the lesions.
- Was the onset of oral lesions acute (e.g., over hours or days) or chronic (e.g., over weeks or months)?
- Are there single or multiple lesions?
- Is there a history of similar conditions (i.e., does the patient have recurring mouth ulcers)?
- Where are the lesions located: in the oral/perioral regions only, or in the oral/perioral regions with involvement of additional surfaces?
- Where are the oral/perioral lesions located (e.g., lips, cheeks, tongue, gingiva, palate, floor of mouth, oropharynx)?
- Is there a history of oral/perioral trauma?
- Are the lesions associated with systemic symptoms, such as fever, malaise, lymphadenopathy, gastrointestinal pain, nausea, vomiting, diarrhea, and/or generalized joint/muscle pain?
- Does anyone else in the family (i.e., parents, grandparents, siblings) have a recent or chronic history of oral/perioral ulcers?
- Did the child come into contact recently with anyone with visible oral/perioral ulcers? Did they share toys, utensils or cups with that individual?
- Perform a clinical examination:
- If possible, record patient’s weight and monitor weight for any significant changes during follow-up visits.
- Review vital signs and monitor any significant abnormalities due to possible metabolic disturbances secondary to inadequate hydration and/or nutrition intake.
- Complete a thorough head and neck exam for detection of lymphadenopathy and ulcers on exposed cutaneous and/or mucosal surfaces.
- Complete a thorough oral/perioral examination to detect ulcers on any oral/perioral surfaces and/or oropharynx.
- Overall, evaluate if the child looks ill.
- Further Laboratory Testing:
- Not usually done by general practitioners; if laboratory testing is indicated, patient should be referred to his/her family physician, pediatrician and/or oral medicine specialist.
Diagnosis
Given the nonspecific clinical presentation of many oral ulcerative conditions in the pediatric population, the clinician should consider the following differential diagnoses:
Single Ulcers
- Trauma
- Recurrent aphthous ulcer
- Deep fungal infection (rare)
- Cancer (rare)
Multiple Ulcers
Infectious Etiology
Bacterial
- Acute necrotizing ulcerative gingivitis
- Perioral impetigo
Viral
- Primary herpetic gingivostomatitis
- Recurrent herpes infections
- Herpangina
- Acute lymphonodular pharyngitis
- Hand-foot-and-mouth disease
- Varicella
- Measles
Chronic Ulcerative and Vesiculobullous Conditions
- Recurrent aphthous stomatitis
- Juvenile bullous pemphigoid
- Childhood linear IgA disease
- Hereditary epidermolysis bullosa
- Juvenile dermatitis herpetiform
- Riga–Fede disease
Associated with Systemic Conditions
- Congenital neutropenia
- Autoimmune disorders (e.g., lupus erythematosus, Crohn disease)
- Behçet syndrome
- PFAPA syndrome, a clinical disorder characterized by periodic fever, aphthous stomatitis, pharyngitis and cervical adenitis.
- Metabolic deficiency diseases
- HIV/AIDS
Treatment
Common Initial Treatments
- Palliative treatment:
- Monitor nutritional intake and ensure adequate hydration.
- Manage fever with over-the-counter antipyretics (i.e., acetaminophen).
- Consider use of antimicrobial mouthwash to prevent secondary infection of ulcers (if the patient can swish and spit).
- If you can confirm a specific diagnosis for the oral ulcers, consider treatment with appropriate medications, such as antibiotics, antiviral agents and topical corticosteroids, within your scope of expertise.
- If the patient appears to be significantly dehydrated, lethargic or demonstrates signs of failure-to-thrive, refer the patient to an acute care facility for urgent evaluation.
- The patient should be clinically re-evaluated 2 weeks after initial presentation.
Alternate Treatments
- If a systemic condition is suspected as the cause of oral ulcers, the patient should be referred to his/her primary care physician and/or pediatrician for further evaluation and management.
- Consider referring patients with organ-specific ulcers to medical subspecialists (i.e., dermatologist, gastroenterologist, otorhinolaryngologist) for evaluation and management, if necessary.
Advice
- Provide supportive advice to the patient and family.
- Encourage frequent hydration and nutritional intake.
- Monitor for resolution of oral lesions and/or systemic symptoms.
- If the patient appears to be significantly dehydrated, weak and/or demonstrates signs of failure-to-thrive, the patient should be taken to the family physician or an acute care facility for urgent evaluation.
- If the ulcers have not resolved in more than 2 weeks, refer the patient to his/her family physician, pediatrician and/or oral medicine specialist for further evaluation and management.
THE AUTHORS
Suggested Resources
- Greenberg MS, Glick M, Ship JA, editors. Burket’s oral medicine. 11th ed. Hamilton: BC Decker; 2008.
- Pinto A. Pediatric soft tissue lesions. Dent Clin North Am. 2005;49(1):241-58.
- Patel NJ, Sciubba J. Oral lesions in young children. Pediatr Clin North Am. 2003;50(2):469-86.
- Flaitz CM, Baker KA. Treatment approaches to common symptomatic oral lesions in children. Dent Clin North Am. 2000;44(3):671-96.