In dentistry, commonly prescribed medications include antibiotics, to treat and prevent infection, and non-opioid and opioid analgesics, to prevent and relieve pain. Both types of medications are classified based on their structure and mechanism of action.1
Globally, antibiotics are widely used.2 A negative consequence of this widespread use is the emergence of bacterial resistance to certain antibiotics,2 which is increasing worldwide.3 Bacteria may be intrinsically resistant to antibiotics, as aerobic bacteria are resistant to metronidazole, or they may acquire resistance through a spontaneous mutation or a transfer of genetic material.2 It is acquired resistance that concerns us because the improper use of antibiotics may lead to such resistance. Moreover, if the dose of antibiotics is too weak or the duration of treatment too long, the chance of mutation increases.4 After mutation, bacteria may survive and divide in the presence of an antibiotic it has achieved resistance against.
The impact of bacterial resistance to antibiotics has been substantial. It is evident in hospitals where normally commensal bacteria are leading to serious nosocomial infections, which in turn may lead to increased clinical complications, length of stay in hospital, morbidity and mortality.5 Some infectious conditions have already become untreatable.2 In 1997, such infections resulted in over 150 000 deaths in the United States.3
Another common medication used in dentistry is opioid analgesics. Long-term use of opioids can lead to tolerance, dependence and even addiction.1 The United States and Canada place first and second in terms of per capita consumption of prescription opioids.6,7 Although many investigations in the United States have looked at the non-medical prescription of opioids,8-10 less research has been carried out in Canada. One report11 suggests that prescription opioid use in Canada in 2007–2009 was more than double that in 2001–2003. An analysis of the records of pharmacies in Canada showed that opioid prescription increased by 13% from 2005 to 2010.12 British Columbia ranked among the top 4 provinces in Canada in total opioid dispensing and among the top 3 in codeine combination dispensing.12
Possibly because of this increase in opioid use, overdoses and emergency room visits resulting from non-prescription opioid use have also increased.11,13-15 In addition, the number of people seeking treatment for prescription opioid addiction is also increasing.16 A 2004 study showed that the number of people seeking opioid detoxification at the Centre for Addiction and Mental Health in Toronto was steadily increasing,16 and the increase was a result of non-medical use of prescription opioids, not drugs such as heroin.
Research regarding the prescription of opioid analgesics and antibiotics by dental professionals is scarce. As these medications may be commonly prescribed by dentists and because of the negative consequences associated with overuse, it is important to examine how and when these medications are prescribed. The aims of this study were to examine the prescribing patterns of general dentists in Vancouver and endodontists in British Columbia regarding antibiotics and opioid analgesics and to associate such prescription with the gender, clinical experience and practice location of clinicians.
We believed that, by surveying dentists in Vancouver, we would obtain useful information that might act as a starting point for further studies in the province. We collected gender and clinical experience information simply because it was easy to do so. We had no reason to believe that male and female clinicians or those of different clinical experience would prescribe medications differently. Clinicians in the western half of Vancouver were compared with those in the eastern half as these 2 areas represent patients of substantially different socioeconomic statuses: patients residing in the western half of Vancouver are generally more affluent than those in the eastern half. We were interested in determining whether this would make a difference in dentists’ prescribing decisions.
Material and Methods
Structured Survey
An original survey was developed by the examiners and revised a number of times. It was not based on any previous surveys. Once we believed that an adequate survey had been prepared, 10 dentists were asked to complete it as a pilot study. Their feedback regarding clarity of the questions and their suggestions were considered and resulted in further revisions.
The survey consisted of 2 parts: the first was designed to collect demographic information (gender, years of clinical practice and location of practice); the second presented 7 clinical scenarios (Table 1). In each case, participants were asked whether they would prescribe an antibiotic or analgesic or both. Clinicians were also asked what specific medication they would prescribe and at what dose. (See Appendix 1 for full survey).
| Scenario A A patient calls your office and reports a severe toothache. The pain is constant and worsens when biting on the tooth or touching the tooth. According to the patient, there is no swelling. Circumstances prevent the patient from coming to your office for immediate treatment. |
| Scenario B Same situation as Scenario A except the patient reports minor localized swelling. |
| Scenario C A patient had a deep composite restoration placed 2 weeks ago, but now presents to your office with a severe toothache associated with the same tooth. The tooth is very painful to percussion. When cold is applied to the tooth, it becomes painful and this lingers for 15 s. A radiograph shows no evidence of periapical radiolucency. The diagnosis is irreversible pulpitis. You proceed with root canal treatment and complete it the same day. |
| Scenario D A new patient presents to your office. Radiography reveals an asymptomatic tooth associated with a periapical radiolucency. A deep restoration of the tooth, completed many years ago, approaches the pulp. It does not respond to thermal or electrical pulp testing, and the tooth is diagnosed as necrotic. You proceed with root canal treatment and complete it the same day. |
| Scenario E A patient presents to your office with a severe toothache associated with localized swelling. The tooth nearest the swelling does not respond to thermal or electrical pulp testing. This tooth is diagnosed as necrotic with an acute apical abscess. Radiography shows a large periapical radiolucency. You initiate root canal treatment that same day. You fully instrument all of the canals, obtaining some drainage through the canals and plan to complete root canal treatment at another appointment. |
| Scenario F You recently completed root canal treatment on a patient’s tooth. After 3 days, the patient returns in severe pain with a visible swelling in the gingival area of the tooth that was treated. Your final radiograph shows no obvious deficiencies in the root canal filling. |
| Scenario G The patient in scenario F returns again 2 days later with unbearable pain and swelling that has progressed significantly. The skin overlying the area of the treated tooth is red and warm. |
Survey Sample
We obtained a list of all dentists registered with the College of Dental Surgeons of British Columbia. This directory included 615 general dentists with offices in Vancouver and 54 endodontists practising throughout British Columbia.
No similar study was available for comparison of sample size. Given that surveying all dentists was not manageable, we decided on a conservative sample and used a random number generator to select approximately half of the general dentists practising in Vancouver (n = 284); 25 were subsequently excluded as they could not be contacted, were no longer working in the area or had retired. As the number of endodontists in British Columbia is much lower than the number of general dentists, we included all endodontists practising in the province, except for 3 full-time professors and 1 who had moved out of the country. Thus, the final sample included 259 general dentists and 50 endodontists.
Distribution of Surveys
To maximize the response rate, we sent the questionnaire 3 times. In the first round, it was sent by email to all clinicians with an email address listed in the directory. If an email address was not listed, the survey was sent by fax. In the absence of an email address and fax number, surveys were mailed to dentists’ offices. All practitioners were provided 3 options to return the completed survey: email, fax or post.
After 4–6 weeks, we telephoned the offices of all non-respondents. After briefly explaining the research to the staff member who answered the telephone, we asked how best to send the survey to ensure that the dentist received it. Based on this response, we sent the survey a second time by email, fax or post, which may or may not have been the same method used when distributing the survey the first time.
Two months after the second distribution, we mailed the survey to all non-responding offices along with a pre-stamped return envelope.
Response Rates
A total of 152 (116 general dentists and 36 endodontists) completed surveys were returned, for an overall response rate of 49.2%. The response rate was 44.8% for the sample of general dentists and 72.0% for the endodontists.
Comparison Groups and Statistical Analyses
We compared endodontists vs. general dentists, men vs. women, those with > 15 years of clinical experience vs. those with ≤ 15 years and those practising in the eastern vs. western half of Vancouver. The data were analyzed using SPSS, v. 21.0 software with the threshold for statistical significance set at p < 0.05. We used χ2 (for n values > 10) or Fisher’s exact test (n values < 10) to test for significant differences in sample sizes, respectively.
Results
Demographics
In our sample of 116 general dentists and 36 endodontists, 34% were women and 66% were men. Among the general dentists, 80% practised in the western half of Vancouver and 20% in the eastern half. Average clinical experience was 21.2 ± 11.8 years.
Prescription of Antibiotics and Analgesics
Scenario A
For the patient in scenario A, most respondents (95%) would prescribe an analgesic (Table 2). We found no significant difference between general dentists and endodontists (p = 1.000). There were also no differences based on clinical experience (p = 0.258), gender (p = 0.444) or practice location (p = 0.603).
| Decision | Scenario A | Scenario B | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | |
| Note: Percentages are based on the number of responses to each question. | ||||||||
| Prescribe antibiotics | ||||||||
| Yes | 54 (37) | 43 (39) | 11 (31) | 0.435 | 108 (73) | 85 (75) | 23 (66) | 0.282 |
| No | 92 (63) | 68 (61) | 24 (69) | 40 (27) | 28 (25) | 12 (34) | ||
| Prescribe analgesics | ||||||||
| Yes | 141 (95) | 107 (95) | 34 (94) | 1.000 | 140 (95) | 107 (95) | 33 (94) | 1.000 |
| No | 8 (5) | 6 (5) | 2 (6) | 8 (5) | 6 (5) | 2 (6) | ||
| Class of analgesic | ||||||||
| Non-opioids | 94 (69) | 71 (68) | 23 (70) | 0.980 | 85 (66) | 63(65) | 22 (69) | 0.918 |
| Opioids | 35 (26) | 27 (26) | 8 (24) | 36 (28) | 28 (29) | 8 (25) | ||
| Strong opioids | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | ||
In terms of the class of medication, 69% of respondents indicated that they would prescribe a non-opioid analgesic, and 26% said they would prescribe an opioid analgesic. We found no significant difference between general dentists and endodontists (p = 0.980) and no differences based on clinical experience (p = 0.346), gender (p = 0.658) or practice location (p = 0.798).
Overall, 37% of respondents indicated that they would prescribe an antibiotic in this scenario. We found no significant difference between general dentists and endodontists (p = 0.435) nor any differences based on gender (p = 0.235) or practice location (p = 0.402). However, clinicians with greater clinical experience would prescribe an antibiotic more often than those with less clinical experience (p = 0.002).
Scenario B
In scenario B, most respondents (95%) would prescribe an analgesic (Table 2). We found no significant difference between general dentists and endodontists (p = 1.000), nor differences based on clinical experience (p = 0.710), gender (p = 0.414) or practice location (p = 0.603).
Among the respondents, 66% reported that they would prescribe a non-opioid analgesic; 28% would prescribe an opioid analgesic. We found no significant difference between general dentists and endodontists (p = 0.918) and no differences based on clinical experience (p = 0.731), gender (p = 0.491) or practice location (p = 0.816).
Most respondents (73%) would prescribe an antibiotic in this scenario with no significant difference between general dentists and endodontists (p = 0.268) nor differences based on clinical experience (p = 0.358), gender (p = 0.294) or practice location (p = 0.090).
Scenario C
In scenario C, most respondents (86%) would prescribe an analgesic (Table 3). We found no significant difference between general dentists and endodontists (p = 0.519), nor differences based on clinical experience (p = 0.631), gender (p = 0.266) or practice location (p = 0.758).
Of all respondents, 81% would prescribe a non-opioid analgesic, and 4% would prescribe an opioid analgesic. We found no significant difference between general dentists and endodontists (p = 0.795), nor differences based on clinical experience (p = 0.592), gender (p = 0.117) or practice location (p = 0.471).
Only 5% of respondents would prescribe an antibiotic in this scenario. We found no significant difference between general dentists and endodontists (p = 0.194), nor differences based on clinical experience (p = 0.252) or gender (p = 0.096). However, 17% of clinicians in the eastern half of Vancouver indicated that they would prescribe an antibiotic, compared with only 4% of those with practices in the western half (p = 0.037).
| Decision | Scenario C | Scenario D | Scenario E | |||||||||
| Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Note: Percentages are based on the number of responses to each question. | ||||||||||||
| Prescribe antibiotics | ||||||||||||
| Yes | 7 (5) | 7 (6) | 0 (0) | 0.194 | 44 (30) | 41 (37) | 3 (9) | 0.001 | 99 (67) | 88 (78) | 11 (31) | < 0.001 |
| No | 139 (95) | 103 (94) | 36 (100) | 102 (70) | 70 (63) | 32 (91) | 49 (33) | 25 (22) | 24 (69) | |||
| Prescribe analgesics | ||||||||||||
| Yes | 125 (86) | 93 (85) | 32 (89) | 0.519 | 100 (68) | 75 (67) | 25 (69) | 0.782 | 135 (92) | 104 (95) | 31 (86) | 0.140 |
| No | 21 (14) | 17 (15) | 4 (11) | 48 (32) | 37 (33) | 11 (31) | 11 (8) | 6 (5) | 5 (14) | |||
| Class of analgesic | ||||||||||||
| Non-opioids | 107 (81) | 79 (80) | 28 (85) | 0.795 | 87 (63) | 65 (62) | 22 (67) | 0.436 | 92 (71) | 68 (69) | 24 (75) | 0.039 |
| Opioids | 4 (5) | 5 (5) | 1 (3) | 5 (4) | 5 (5) | 0 (0) | 28 (22) | 25 (26) | 3 (9) | |||
| Strong opioids | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |||
Scenario D
As in previous scenarios, most respondents (68%) would prescribe an analgesic based on scenario D (Table 3). We found no significant difference between general dentists and endodontists (p = 0.782), nor differences based on clinical experience (p = 0.154) or practice location (p = 0.277). However, 80% of female respondents would prescribe an analgesic, compared with 60% of male clinicians (p = 0.014).
Of all respondents, 63% would prescribe a non-opioid analgesic, and 4% would prescribe an opioid analgesic. We found no significant difference between general dentists and endodontists (p = 0.436) nor differences based on clinical experience (p = 0.139) or practice location (p = 0.375). Female clinicians would prescribe a non-opioid analgesic more often than their male counterparts (76% vs. 56%, p = 0.047).
Based on scenario D, 30% of all respondents would prescribe an antibiotic, with a significant difference between general dentists and endodontists (37% vs. 9%, respectively, p = 0.001). We found no significant differences based on clinical experience (p = 0.157), gender (p = 0.769) or practice location (p = 0.801).
Scenario E
Based on this scenario, 93% of all respondents would prescribe an analgesic (Table 3). We found no significant difference between general dentists and endodontists (p = 0.140), nor any differences based on clinical experience (p = 0.526), gender (p = 0.747) or practice location (p = 0.100).
Of all respondents, 71% would prescribe a non-opioid analgesic, whereas 22% would prescribe an opioid analgesic. In prescribing an opioid analgesic, we noted a significant difference between general dentists and endodontists: 26% vs. 9% (p = 0.039). No differences were based on clinical experience (p = 0.296), gender (p = 0.482) or practice location (p = 0.337).
In this scenario, 67% of all respondents would prescribe an antibiotic; a significant difference was seen between general dentists and endodontists: 78% vs. 31% (p < 0.001). We found no differences based on gender (p = 1.000) or practice location (p = 0.492), but respondents with greater clinical experience prescribed antibiotics more often than those with less clinical experience (p = 0.014).
Scenario F
Of all respondents, 99% would prescribe an analgesic in this scenario (Table 4). We found no significant difference between general dentists and endodontists (p = 1.000), nor any differences based on clinical experience (p = 1.000), gender (p = 1.000) or practice location (p = 0.213).
Of all respondents, 65% would prescribe a non-opioid analgesic, while 34% indicated that they would prescribe an opioid analgesic. We found no significant differences between general dentists and endodontists (p = 0.071), nor differences based on clinical experience (p = 0.697), gender (p = 0.688) or practice location (p = 0.153).
| Decision | Scenario F | Scenario G | ||||||
|---|---|---|---|---|---|---|---|---|
| Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | Overall, no. (%) | GD, no. (%) | Endo, no. (%) | p | |
| Note: Percentages are based on the number of responses to each question. | ||||||||
| Prescribe antibiotics | ||||||||
| Yes | 129 (88) | 102 (92) | 27 (77) | 0.031 | 109 (76) | 82 (75) | 27 (79) | 0.652 |
| No | 17 (12) | 9 (8) | 8 (23) | 35 (24) | 28 (25) | 7 (21) | ||
| Prescribe analgesics | ||||||||
| Yes | 145 (99) | 110 (99) | 35 (100) | 1.000 | 96 (66) | 75 (68) | 21 (60) | 0.421 |
| No | 1 (1) | 1 (1) | 0 (0) | 50 (34) | 36 (32) | 14 (40) | ||
| Class of analgesic | ||||||||
| Non-opioids | 82 (65) | 58 (61) | 24 (77) | 0.071 | 20 (16) | 11 (11) | 9 (31) | 0.021 |
| Opioids | 43 (34) | 37 (39) | 6 (19) | 41 (32) | 37 (37) | 4 (14) | ||
| Strong opioids | 1 (1) | 0 (0) | 1 (3) | 19 (15) | 15 (15) | 4 (14) | ||
Of all respondents, 88% would prescribe an antibiotic in this scenario: 92% of general dentists, compared with 77% of endodontists (p = 0.031). We found no significant differences based on clinical experience (p = 0.509), gender (p = 0.555) or practice location (p = 0.153).
Scenario G
Overall, 66% of respondents would change the analgesic they had originally prescribed in scenario F (Table 4), and we found no significant difference between general dentists and endodontists (p = 0.411). There were also no differences based on clinical experience (p = 0.792), gender (p = 0.980) and practice location (p = 0.903).
Of the respondents, 16% indicated that they would prescribe a non-opioid analgesic in this scenario, 32% would prescribe an opioid analgesic and 15% would prescribe a strong opioid. General dentists and endodontists differed in the types of analgesics they would now prescribe, with general dentists more likely to prescribe opioid analgesics (p = 0.021). We found no differences based on clinical experience (p = 0.452), gender (p = 0.935) or practice location (p = 0.291).
Regarding antibiotic prescription, 76% would change the antibiotic they had originally prescribed in scenario F, and the difference between general dentists and endodontists was not significant (p = 0.563). There were also no significant differences based on gender (p = 0.485) or practice location (p = 0.280), but respondents with greater clinical experience were more likely to change the type of antibiotic they had prescribed earlier (p = 0.009).
Comparisons between general dentists and endodontists in terms of prescribing antibiotics and analgesics in all scenarios are summarized in Fig. 1 and Fig. 2, respectively.
Figure 1: Prescription of antibiotics by general dentists (n = 116) and endodontists (n = 36) in various scenarios.
Figure 2: Prescription of opioid analgesics by general dentists (n = 116) and endodontists (n = 36) in various scenarios.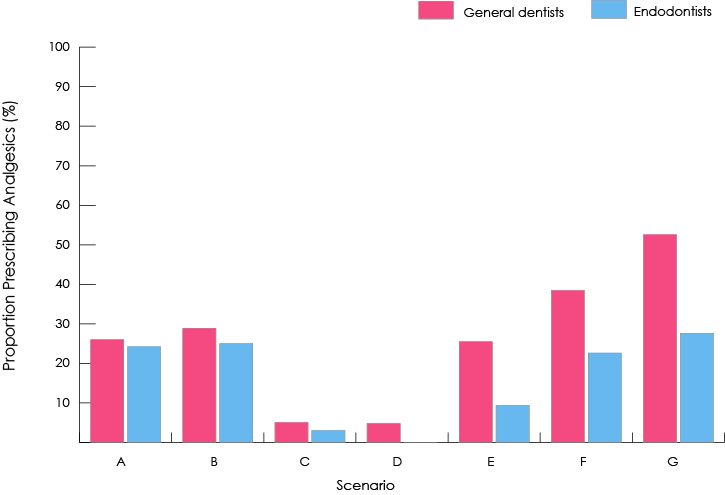
Discussion
The use of antibiotics to treat endodontic conditions is limited. Evidence has shown that root canal procedures combined with analgesic medications are sufficient for managing most symptomatic endodontic cases.17 The literature suggests that antibiotics may be used in addition to endodontic treatment in situations where there are signs of systemic involvement where swelling is increasing or where the patient is immunocompromised.17 Based on these guidelines, antibiotics would only be indicated in scenario G. Thus, our clinical scenarios revealed high rates of antibiotic prescription: at least 30% in 6 of the 7 scenarios.
Post-treatment pain may occur in 25–40% of all endodontic cases,18,19 and analgesics are often prescribed to manage such pain. Evidence shows that NSAIDs, such as ibuprofen, in large doses are effective in treating moderate to severe pain.18,20 NSAIDs are more effective than acetaminophen, medications combining acetaminophen and codeine and even medications combining acetaminophen and oxycodone.20 In our study, the overall rate of prescription of opioid analgesics was high: at least 22% in 5 of the 7 scenarios. According to recommendations, non-opioid analgesics should be used to their maximum effect before starting opioid use.21 This means that opioids should only have been prescribed where initial non-opioid treatment failed to relieve severe pain, i.e., in scenario G.
Overall, general dentists prescribed antibiotics and opioid analgesics more often than endodontists. No consistent differences were observed related to gender, clinical experience or practice location.
A difficulty in assessing these results is the lack of guidelines for comparison. However, based on recommendations made by experts in the field, our results suggest that a significant proportion of general dentists in Vancouver and endodontists in British Columbia prescribe antibiotics and opioid analgesics when they are not indicated. Overall, general dentists reported prescribing both antibiotics and opioid analgesics more often than endodontists. We observed no consistent trends related to gender, clinical experience or practice location, i.e., a clinician’s gender, clinical experience or practice location did not affect their likelihood of prescribing these medications.
Because of the impact of overuse, the availability of guidelines for the prescription of antibiotics and opioid analgesics would be valuable to society as a whole. We suggest that organizations, such as the Canadian Dental Association and the American Dental Association, work together to develop guidelines for the appropriate use of antibiotic and opioid analgesics in endondontic treatments.
A limitation of the present study is that the results are based on self-reported data. Thus, we cannot state with certainty that the responses accurately represent how clinicians act in their daily practice.
Conclusions
According to our survey of general dentists in Vancouver and endodontists in British Columbia, a substantial proportion of dental professionals prescribe opioid analgesics and antibiotics unnecessarily during endodontic procedures. General dentists tend to prescribe these medications more often than endodontists. We found no apparent differences based on gender, clinical experience or practice location.
THE AUTHORS
References
- Brunton LL, Chabner BA, Knollman BC, editors. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill; 2011.
- Standing Medical Advisory Committee, Sub-group on Antimicrobial Resistance. The path of least resistance. London: Department of Health; 1998. Available from: http://webarchive.nationalarchives.gov.uk/20081106020107/http://www.dh.gov.uk/en/
Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009357 [cited 2017 Jul 24]. - American Dental Association Council on Scientific Affairs. Antibiotic use in dentistry. J Am Dent Assoc. 1997;128(5):648.
- Bidault P, Chandad F, Grenier D. Risk of bacterial resistance associated with systemic antibiotic therapy in periodontology. J Can Dent Assoc. 2007;73(8):721-5.
- Smith RD, Coast J. Antimicrobial resistance: a global response. Bull World Health Organ. 2002;80(2):126-33.
- Fischer B, Gittins J, Rehm J. Characterizing the “awakening elephant” of prescription opioid misuse in North America: epidemiology, harms, interventions. Contemporary Drug Problems. 2008; 35(2-3):397-426.
- International Narcotics Control Board. Narcotic drugs: estimated world requirements for 2011. Statistics for 2009. New York: United Nations; 2011. Available from: https://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/20… [cited 2017 Jul 24].
- Results from the 2003 National Survey on Drug Use and Health: national findings. NSDUH series H-25. Publication SMA 04-3964. Rockville, Md.: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2004.
- Johnson LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future: national results on adolescent drug use. Overview of key findings 2005. NIH publication 06-5882. Bethesda, Md.: National Institute on Drug Abuse; 2006. Available from: http://www.monitoringthefuture.org/pubs/monographs/overview2005.pdf [cited 2017 Aug 2].
- Whiteside LK, Walton MA, Bohnert AS, Blow FC, Bonar EE, Ehrlich P, et al. Nonmedical prescription opioid and sedative use among adolescents in the emergency department. Pediatrics. 2013;132(5):825-32.
- International Narcotics Control Board. Report of the International Narcotics Control Board for 2012. New York: United Nations; 2013. Available from: https://www.incb.org/documents/Publications/AnnualReports/AR2012/AR_2012_E.pdf [cited 2017 Jul 24].
- Fischer B, Jones W, Krahn M, Rehm J. Differences and over-time changes in levels of prescription opioid analgesic dispensing from retail pharmacies in Canada, 2005-2010. Pharmacoepidemiol Drug Saf. 2011;20(12):1269-77.
- Manchikanti L. National drug control policy and prescription drug abuse: facts and fallacies. Pain Physician. 2007;10(3):399-424.
- Hurwitz W. The challenge of prescription drug misuse: a review and commentary. Pain Med. 2005;6(2):152-61.
- Paulozzi LJ, Budnitz DS, Xi Y. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Saf. 2006; 15(9):618-27.
- Sproule B, Brands B, Li S, Catz-Biro L. Changing patterns in opioid addiction: characterizing users of oxycodone and other opioids. Can Fam Physician. 2009;55(1):68-9,69.e1-5.
- Fouad AF. Are antibiotics effective for endodontic pain? Endod Topics. 2002;3:52-66. doi:10.1034/j.1601-1546.2002.30106.x
- Holstein A, Hargreaves KM, Niederman R. Evaluation of NSAIDs for treating post-endodontic pain. Endod Topics. 2002;3:3-13. doi:10.1034/j.1601-1546.2002.30102.x
- Harrison JW, Baumgartner CJ, Zielke DR. Analysis of interappointment pain associated with the combined use of endodontic irrigants and medicaments. J Endod. 1981;7(6):272-6.
- The Oxford League table of analgesic efficacy. Bandolier Journal; 2007. Available from: http://www.bandolier.org.uk/booth/painpag/Acutrev/Analgesics/lftab.html
- Keiser K, Hargreaves KM. Building effective strategies for the management of endodontic pain. Endod Topics. 2002;3:93-105.





