ABSTRACT
Objective: Dental disease is concentrated among those with low socioeconomic status. Dental care is not publicly funded, and many Canadians must therefore make difficult financial choices when accessing dental care. Families who live in poverty have difficulty meeting even their most basic household needs, so dental treatment may not be affordable. The objective of this study was to understand how the cost of dental treatment affects the monthly budgets of families with low incomes.
Materials and Methods: A chart review was conducted for a sample of 213 new patients examined at the Dalhousie University dental clinic over a 1-year period. Costs for proposed treatment plans were averaged. The patients’ ability to pay for proposed treatment was examined in the context of various income scenarios.
Results: Two hundred and one patients were included in the final analysis. Dental treatment costs per patient averaged approximately $1600 for the year, with 42% of the planned treatment completed within the first year. The estimated monthly cost of completed treatment was $55. When the cost of a healthy diet was included in the monthly budget, it was determined that families in Nova Scotia with parents working for minimum wage and those receiving income assistance would experience a 100% shortfall for dental expenses.
Conclusions: Low-income families in Nova Scotia were unable to afford both a nutritious diet and dental care. This is disturbing, given the links between a healthy diet and both overall health and dental health. An understanding of the significance of income shortfalls for those with low incomes, especially as they affect even basic nutritional needs, will help dental professionals to appreciate the seriousness of this issue and the difficulties that many Canadians face when trying to access basic dental care.
Introduction
It is well established that dental disease is concentrated among those with low socioeconomic status.1,2 Even in Canada, which ranks among the most developed countries, those who bear the greatest burden of morbidity have the most difficulty affording dental care.3 In most jurisdictions, those who do not have access to private dental insurance and do not qualify for government assistance programs are required to pay for dental care out of their own pockets.4 This is a difficult situation for many Canadians, especially the “working poor” and those receiving government assistance.4
According to the National Council on Welfare, 11% of Canadians live in poverty.5 Families who live in poverty are known to have difficulty meeting even their most basic household needs.6 Among the most troubling reality is “food insecurity,” a situation characterized by a lack of sufficient resources to meet the requirements for a healthy diet.7 Of particular relevance to dentistry is the impact that dental disease and the costs of dental treatment may have on the household budgets of low-income families and, by extension, their food security. Research has demonstrated that dental disease is linked to food insecurity when food purchases must be compromised to pay for dental care.8 In the face of these difficult choices about how income is to be spent, it is not difficult to understand why many Canadians are unable to place a high priority on dental care.
The purpose of this study was to better understand the economic implications of the real costs of dental treatment as they relate to budgeting for low-income families. University dental clinics provide ideal sites for such research. A large proportion of patients who attend such clinics have very low incomes and seek care in this setting to take advantage of fees that are typically lower than those in private practice.9 Using various income scenarios, we set out to examine dental treatment costs in relation to other household expenses, particularly food costs.
Materials and Methods
In this study undertaken at Dalhousie University, Halifax, Nova Scotia, the average treatment costs for new patients attending the dental teaching clinic were calculated. Ethics approval was obtained from the Dalhousie University Health Sciences Human Research Ethics Board. Retrospective data were collected from the clinic’s computerized patient database (axiUm, Exan Enterprise Inc., Las Vegas, NV). From the list of patients who had received a treatment plan during the academic year 2006–2007, every fifth patient chart was selected to generate a sample of 213 patients. Edentulous patients and children under the age of 16 were excluded using specific identifier codes. The sample represented 14.8% of the 1439 new patients seen that year. Twelve patients had total fees that were greater than 2 standard deviations above the mean, and these outliers were removed, for a final sample size of 201. Income data were not available for the patients in the sample.
The costs of planned and completed treatments were determined for each patient for the 1-year period after approval of the treatment plan. Treatments analyzed included diagnostic and preventive procedures, periodontics, restorative procedures, removable prosthodontics, minor surgery, interceptive orthodontics and endodontics. Prosthodontic procedures related to fixed and implant-retained prostheses were excluded from the analysis because of the complexity of these treatments and the lengthy time frames for their completion. Fees at the dental clinic were based on approximately 50% of the fees in the 2006 fee guide of the Nova Scotia Dental Association (for general dentists). Therefore, an estimation of the costs of similar treatments in private practice can be determined by doubling the fees reported here. Projected household costs for families with various incomes were obtained from food-costing data for 2004/056 and included the cost of the National Nutritious Food Basket (NNFB) for a family of 4. To understand the financial burden of treatment needs for families living at or below the median income range, the average cost of treatment was examined in the context of 5 income scenarios for a family of 4 with 2 children: income assistance without benefits for dental services; income assistance with Nova Scotia Department of Community Services employment support and income assistance dental benefits; employment with minimum wage, with 1 parent working full-time and the other working part-time; employment with average call centre wage, with 1 parent working full-time and the other working part-time; and median income for Nova Scotia families. No adjustments were made to account for the 1-year difference between the income and food-costing data (2004/05) and the dental costs in the fee guide (2006), as the increase in dental fees from 2005 to 2006 was negligible (less than 3%).
Results
The average annual cost for planned dental treatment for the patients in this study was $1593.24 for the year ($132.77 per month). Figure 1 highlights both the estimated cost of planned treatment and the percentage of treatment completed for each patient during the study year. As might be expected, lower total treatment costs were associated with a greater percentage of treatment completed within 1 year of the treatment plan. On average, patients had completed 42% of the planned treatment within the first year following documentation of their respective treatment plans. This translates to an estimated monthly cost of $55.22. In Table 1, this cost is considered as an additional monthly expense for the various income scenarios.
Table 1 Analysis of dental costs in Nova Scotia (NS) in the context of various monthly income and expense scenarios
(for 2004/05)a
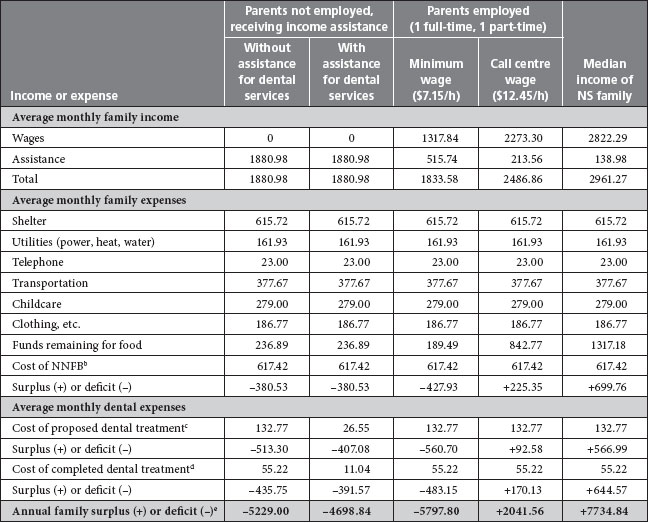
a Adapted from Nova Scotia Participatory Food Security Projects.6 All scenarios are for families of 4 (2 parents and 2 children).
b NNFB = National Nutritious Food Basket.
c Cost of dental treatment based on average cost of planned dental treatment for 1 adult, at 50% of the rates in the Nova Scotia Dental Association fee guide (data from this study, for academic year 2006-2007).
d Cost of dental treatment based on average cost of completed dental treatment for 1 adult, at 50% of the rates in the Nova Scotia Dental Association fee guide (data from this study, for academic year 2006-2007).
e Surplus or deficit estimate is based on the average cost of completed dental treatment for 1 adult.
We determined that families receiving income assistance or with 2 parents working for minimum wage (1 part-time and 1 full-time) would have had a 100% shortfall for costs associated with dental treatment both in the teaching clinic and in private practice. In Nova Scotia, families receiving income assistance who are eligible for dental services benefits through the Nova Scotia Department of Community Services are required to pay 20% of treatment costs. These families would have a 100% shortfall for this copayment ($11/month). Overall, a family of 4 with 2 parents working for minimum wage would have a calculated household deficit of $5797.80 with dental care for 1 parent. A similar situation would create a deficit of $5229.00 for families receiving income assistance. These estimates do not include costs for dental treatment for the other parent or for the children.
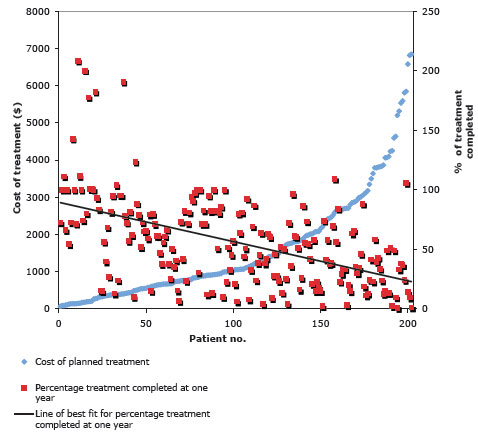
Figure 1: Cost of planned treatment and percentage of treatment completed at 1 year for 201 patients seen in the dental clinic at Dalhousie University.
Discussion
This study highlights the financial limitations experienced by people in low-income brackets when accessing dental care. In fact, families living in Nova Scotia in 2005 that were receiving income assistance or that had 2 parents working for minimum wage (1 part-time and 1 full-time) would have had difficulty affording dental treatment for any member of the family, even at 50% of the fees listed in the fee guide for general dentists. Jobs held by “working poor” individuals typically do not include dental benefits.10 For Nova Scotians receiving income assistance that includes dental benefits, even the copayment would be potentially prohibitive.
It is known that dental disease is concentrated among those with low socioeconomic status, who exhibit a disproportionately high level of dental disease.1,2 By considering the real cost of dental treatment in the context of theoretical income scenarios, this study provides insight into the financial shortfalls faced by many Canadian families. Income data are not collected as part of the clinic record at the Dalhousie dental clinic. Therefore, we do not claim that this study population represents the income scenarios described, and we acknowledge that our sample may not be representative of those who are most financially challenged, who would be expected to have even higher burdens of disease. Indeed, if the dental needs of low-income families are greater than the needs for the typical patient visiting the Dalhousie dental clinic, the income shortfall would be even greater than what we have proposed using theoretical scenarios, and these families would clearly be unable to afford recommended dental care.
The data for various income levels and household expenses in Nova Scotia suggest that families receiving income assistance and families working for minimum wage are unable to afford a nutritious diet.6 Once additional costs such as dental treatment are added to average expected expenses, decisions must be made as to how to allocate scarce resources. It has already been mentioned that people will pay for dental treatment by sacrificing food purchases.8 Muirhead and colleagues8 also suggested that low-income families may purchase lower-cost foods containing higher levels of sugar in place of nutrient-dense foods, such as fruits and vegetables. This contributes to a vicious circle that may compound existing disparities associated with both adequate nutrition and oral health. Specifically, low income contributes to the consumption of a diet that increases the risk for dental disease (i.e., a diet high in sugar). Allocating finances to treat dental disease leaves even fewer resources to support a nutritious diet.
This study had several limitations. Because income data were not available, no direct conclusions could be drawn about the affordability of dental care for the patient population of the Dalhousie dental clinic. Also, patients’ ability to complete treatment might have been limited by the amount of work that could be completed within the 1-year period, given the limited pace of work during the training of students in the dental clinic.
Conclusions
One of the objectives of this project was to raise awareness about the financial challenges for low-income families needing dental care. By estimating the costs of treatment at the Dalhousie faculty of dentistry and analyzing these costs in the context of various income scenarios, we were able to obtain a better understanding of how the cost of dental treatment affects the monthly budgets of those with low incomes. To afford dental care, these families are faced with having to forgo other essential needs, such as a nutritious diet. This represents a serious health concern and requires attention from the dental profession. A concerted effort by the profession, government and society at large to create effective health promotion and prevention strategies and to advocate for the social supports required to meet the oral health needs of disadvantaged populations would go a long way toward minimizing health disparities in Canada.
THE AUTHORS
References
- Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century--the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31 Suppl 1:3-23.
- Sabbah W, Tsakos G, Chandola T, Sheiham A, Watt RG. Social gradients in oral and general health. J Dent Res. 2007;86(10):992-6.
- Leake JL, Birch S. Public policy and the market for dental services. Community Dent Oral Epidemiol. 2008;36(4):287-95.
- Main P, Leake J, Burman D. Oral health care in Canada--a view from the trenches. J Can Dent Assoc. 2006;72(4):319. Available: www.cda-adc.ca/jcda/vol-72/issue-4/319.html.
- National Council of Welfare. Poverty by province for all persons, 2004. Poverty statistics 2004. Available: www.ncwcnbes.net/documents/researchpublications/ResearchProjects/PovertyProfile/2004/PovertyRatesProvinces-AllENG.pdf (accessed 2010 Feb 2).
- Nova Scotia Participatory Food Security Projects. Working together to build food security in Nova Scotia: participatory food costing 2004/05. March 2007. Available: www.ahprc.dal.ca/publications/Finalreport2004-05FoodCosting.pdf (accessed 2010 Feb 2).
- Davis B, Tarasuk V. Hunger in Canada. Agriculture and Human Values. 1994;11(4):50-7.
- Muirhead V, Quinonez C, Figueiredo R, Locker D. Oral health disparities and food insecurity in working poor Canadians. Community Dent Oral Epidemiol. 2009; 37(4):294-304. Epub 2009 Jun 9.
- Damiano PC, Warren JJ. A profile of patients in six dental school clinics and implications for the future. J Dent Educ. 1995;59(12):1084-90.
- Fleury D, Fortin M. When working is not enough to escape poverty: an analysis of Canada's working poor. Human Resources and Social Development Canada, Policy Research Group. August 2006. Available: www.hrsdc.gc.ca/eng/cs/sp/sdc/pkrf/publications/research/SP-630-06-06/SP-630-06-06E.pdf (accessed 2010 Feb 2).

Dalhousie program promotes student research interests: Scholarship Across the Curriculum is an academic requirement within the Dalhousie dental and dental hygiene programs that challenges students to examine relevant research and clinical care questions. The research presented in this article is based on a project developed by Patrick Snow, who recognized that many patients at the Dalhousie University dental clinic face difficult financial choices when seeking dental care.
