Abstract
Objectives: To explore reasons for the underuse of dental services covered by a government-funded program in Alberta.
Methods: In 2011, a survey questionnaire was sent to 4000 randomly selected clients of the Alberta Child Health Benefit and the Alberta Adult Health Benefit programs. Only respondents with children were included in the analysis. Reasons were explored among those who indicated that their children did not receive any dental services in the year before the survey. Difficulties faced by those who reported receiving at least 1 dental service were also noted.
Results: Among 795 respondents, 597 had at least 1 child. A total of 1303 children aged 1–19 years (mean age 11.79 years, standard deviation 4.2) were included in the analysis. Of these children, 443 (34.0%) had not received any covered dental services; the most common reason (50.7%) was no perceived need (interpreted from the replies "my child was too young" or "had no dental problems") followed by perceived insufficient coverage (38.6%). The most common challenge reported by dental care users was also insufficient coverage (44.9%). About 57% of parents were aware that annual fluoride application was covered by the program; however, only 34.3% of their children received fluoride and 14.2% had sealants.
Conclusions: Low-income families underuse available dental benefits for children. Perceived need seems to be the primary determinant of use. Parental awareness about the coverage does not seem to promote the use of preventive measures for young children.
Oral diseases are serious health threats, particularly dental caries, which remains the most prevalent unmet health care need and chronic disease in children.1 Dental caries is largely preventable through a virtuous combination of at-home and professional dental care in the form of adequate oral hygiene, control of sugar intake and regular dental visits.2 Frequent use of dental services has been associated with better oral health.3 It allows early assessment of the needs and risk factors for disease, prevention of onset of caries through evidence-based preventive measures and detection and management of dental problems at early stages. Dental visits also have the potential to enhance preventive practices at home through parent education.
Disparities in the use of dental care have been widely reported in dentistry literature. Younger children and elders, recent immigrants, poor and near-poor people and racial and ethnic minorities are less likely to receive dental care and, thus, experience dental diseases more often.4–6 Multiple factors have been associated with the use of dental care, including income, education attainment, ethnicity, perceived oral health status and dental insurance.7,8
Dental insurance is a strong predictor of receiving dental care and a factor that is modifiable through dental health policies.9 Therefore, emphasis has been placed on enhancing affordability of dental services by providing publicly funded dental insurance to people with low income. Studies measuring the impact of public insurance have consistently shown increased odds of receiving dental care.8 However, the use of dental services by publicly insured people has been lower than that of their privately insured counterparts as well as below the recommended level of dental care.10 The observed benefits of public insurance have been limited for some racial/ethnic minorities, such as Hispanic and African Americans, as well as for young children, possibly because parents do not perceive a need for pediatric dental care at early ages.5 Low rates of dental care among young children are of particular concern, as an increase in caries level has been observed in this age group.11 Overall, dental insurance seems to enhance access, but not frequency of use of dental care.9
The lower than expected impact of public dental insurance is a result of factors related to availability, enrolment, acceptance, amount of coverage and patterns of use of dental care among less affluent groups.12 Studies have shown a considerable gap between eligibility and insured status.13In Canada, the dental care system is predominantly private, with only about 5% of current expenditures on dental services coming from public programs.14 Low acceptance of public insurance among dentists has been reported repeatedly because of low reimbursement levels and inefficient reimbursement systems.15 Although little evidence exists, it is generally accepted that coverage level plays an important role in the use of dental services by low-income people with competing financial needs.16 However, even when financial barriers are addressed via comprehensive public dental insurance programs, suboptimal use of dental services persists among those insured.17 This shows the complexity and multifactorial nature of the reasons behind the use of dental care among socially disadvantaged groups.2
In Canada, public funding of dental care is intended to assist target groups, such as those with low income, and each province has the autonomy to determine the level and form of public funding as well as the eligibility criteria.18 In Alberta, health benefit programs administered by Alberta Human Services provide low-income Albertans with premium-free diabetic supplies, prescription drugs and dental, optical and emergency ambulance services to ensure their optimal health and well-being. This study complements a previous report on use of dental services by recipients of Alberta Child Health Benefit and the Alberta Adult Health Benefit programs.17 Although a low rate of use of dental services for children was previously reported by parents, barriers related to this suboptimal use remain unexamined. To bridge this gap, a follow-up survey was conducted to identify these barriers.
Methods
In 2011, Alberta Human Services mailed out introductory letters with a survey and a postage-paid return envelope to 4000 randomly selected active client households of the Alberta Child Health Benefit and the Alberta Adult Health Benefit programs (2000 each). The intent of the letter was to inform the client of the survey and its purpose and to encourage participation. Contact information was provided in the event the letter recipient had any questions or concerns about the survey. In the survey, the respondents were asked a series of questions about their demographics, source of information about the benefit programs, use of dental services, and types of dental services received by their children in the past 12 months. Data used for this study were collected by the Alberta Human Services as part of a comprehensive evaluation of its health benefit programs; therefore, the personal information of the participants was blinded to the authors. No ethics approval was required by the University of Alberta Research Ethics Board in order to analyze and report the shared data.
Of the respondents, all Alberta Child Health Benefit clients, but only Alberta Adult Health Benefit clients with children were considered for this study. The respondents were divided into 2 groups: users and non-users of the benefit programs based on whether they received any dental services for their children in the year before the survey. Barriers to access to dental services were explored using 2 questions: 1 requesting reasons why non-users did not receive dental services covered by the program and 1 asking what difficulties users of the program experienced. Clients' awareness of preventive dental services covered by the benefit programs was also explored.
Data were analyzed using SPSS version 20.0 (SPSS Inc., Chicago, Ill., USA). Descriptive statistics were used to identify barriers for both user and non-user groups. Logistic regression analysis was used to determine the probability of using dental services covered by the health benefit plan. The level of significance was defined as p < 0.05.
Results
Among the 795 participants who returned surveys, 597 had at least 1 child; 373 were enrolled with the Alberta Child Health Benefit program and 224 with the Alberta Adult Health Benefit program. Of the respondents with children, 237 (39.7%) were single parents, 415 (69.6%) were women and 301 (50.4%) were from areas other than Edmonton and Calgary (Alberta's 2 largest cities). Table 1 presents the demographic characteristics of the study participants.
Table 1 Demographic characteristics of respondents to the 2011 survey on the use of the Alberta Child Health Benefit and the Alberta Adult Health Benefit programs who had at least 1 child.
| Characteristic* | No. (%†) of respondents (n = 597) |
| Sex | |
| Male | 162 (27.1) |
| Female | 415 (69.5) |
| Location | |
| Edmonton | 141 (23.6) |
| Calgary | 155 (26.0) |
| Other | 301 (50.4) |
| Family structure | |
| Couple with children | 356 (59.6) |
| Single parent, with children | 237 (39.7) |
| No. of children in household | |
| 1 | 190 (31.8) |
| 2 | 167 (28.0) |
| 3 | 100 (16.8) |
| ≥ 4 | 96 (16.1) |
| No. of children by age group (n = 1303)‡ | |
| 0–5 years | 258 (19.8) |
| 6–12 years | 506 (38.8) |
| 13–17 years | 435 (33.4) |
| 18–19 years | 104 (8.0) |
*Based on data provided by Alberta Employment and Immigration in relation to the survey.
†In some categories, the percentages do not total 100% because of missing data.
‡Mean age of children 11.79 years (standard deviation 4.2).
Use of the program and dental services
Most participants (88.3%) considered the Alberta health benefit programs helpful in terms of providing dental services that they would not otherwise be able to use. Clients' source of information about the health benefit programs are listed in Table 2. Of the 1303 children, aged 1–19 years (mean 11.79 years, SD 4.2), who were included in the analysis, 443 (34.0%) had not received any covered dental services (non-users) and 601 (46.2%) had received 3 or more dental services in the previous year (Fig. 1). General dental examination and cleaning were the most frequently received services (57.0% and 53.8%, respectively). Dental sealant and fluoride application were provided to only 185 children (14.2%) and 448 children (34.4%), respectively (Fig. 2). Overall, 254 respondents with children (42.5%) were not aware of their children's eligibility for a yearly dental examination and fluoride application.
Table 2 Source of information about the Alberta health benefit programs of survey respondents with at least 1 child.
| Source |
No. (%) of respondents (n = 597)* |
| Alberta government website or offices | 213 (35.7) |
| Word of mouth | 147 (24.6) |
| Application kit | 64 (10.7) |
| Pamphlet/newsletter/magazine/poster | 63 (10.6) |
| Can't recall/don't know | 63 (10.6) |
| Other | 38 (6.4) |
*Percentages do not total exactly 100% because of missing data.
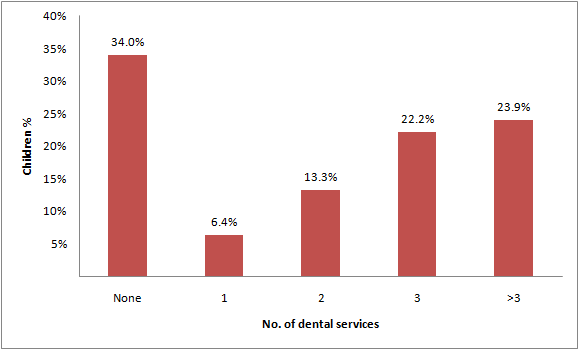 Figure 1: Level of dental service received by children (n = 1303) of respondents to the Alberta health benefit programs survey in the previous year.
Figure 1: Level of dental service received by children (n = 1303) of respondents to the Alberta health benefit programs survey in the previous year.
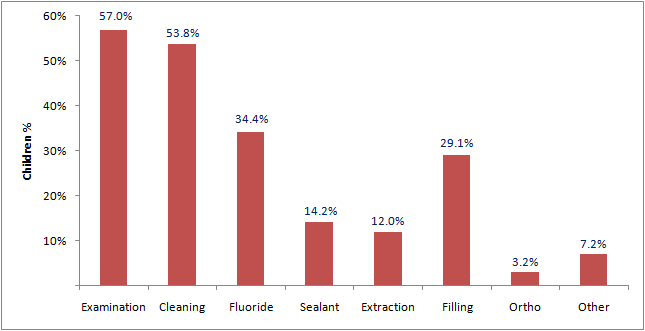 Figure 2: Types of dental services received by children(n = 1303) of respondents to the Alberta health benefit programs survey in the previous year.
Figure 2: Types of dental services received by children(n = 1303) of respondents to the Alberta health benefit programs survey in the previous year.
Barriers to use
Of the respondents with children, 174 (29.1%) did not obtain covered dental services for their children during the year before the survey (non-users). The most common reported reason (50.7%) was no perceived need, interpreted from replies such as "no dental problems," "too young for a dental check-up" (Fig. 3). Other reasons mentioned included lack of knowledge about dental coverage, insufficient coverage, fear of dental treatment, language barrier and lack of time and transportation.
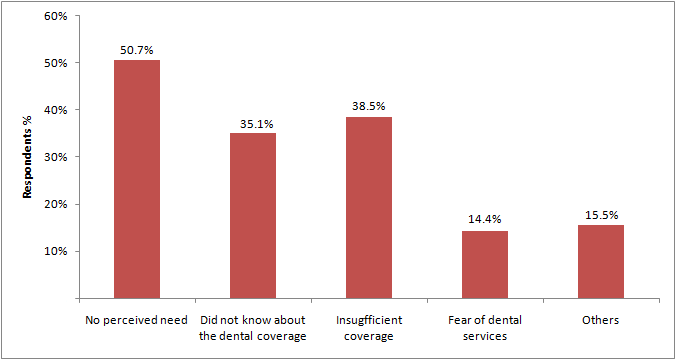 Figure 3: Reasons given by respondents with children who did not use dental services covered by Alberta health benefit programs in the year before the survey (n = 174).
Figure 3: Reasons given by respondents with children who did not use dental services covered by Alberta health benefit programs in the year before the survey (n = 174).
Difficulties
Among the 423 respondents who received at least 1 dental service for their children in the year before the survey (users), 225 (53.2%) reported some difficulties. The most frequent challenge mentioned was insufficient or lack of coverage of the dental services they needed (44.9%). Other reported challenges included inadequate knowledge of the coverage at the time their children received dental treatment (7.3%), problem finding a dentist or dentist not accepting their benefit card (7.8%) and difficulties related to lack of transportation, child care and language barrier while receiving the services (5.0%) (Table 3).
Table 3 Problems and barriers experienced by survey respondents with at least 1 child in gaining access to dental services covered by Alberta health benefit programs.*
| Obstacle/barrier |
No. (%) of respondents (n = 423) |
| None | 199 (47.0`) |
| The plan did not cover all my dental needs | 190 (44.9) |
| Could not find a dentist/Dentist would not accept my health benefit card | 33 (7.8) |
| Little knowledge of the coverage | 31 (7.3) |
| Lack of child care to get to dental appointment | 8 (1.9) |
| Language barrier | 7 (1.7) |
| Lack of transportation, distance to the dental office | 6 (1.4) |
| Other | 10 (2.4) |
*Respondents were able to choose more than 1 response.
Factors affecting use of dental services
Demographic variables had no significant impact on the use of dental services covered by the program; however, families who had more than 2 children reported significantly higher use of the program (p < 0.05).
Discussion
Disparities in use of dental services have been reported for children from low-income families, racial and ethnic minorities and those with special health care needs.19 Low-income families face several challenges accessing and using dental care for their children, including the availability of dental providers who see young or publicly insured children, cost of dental services and parents' perceived need for dental care for their child.20
Parental perceived need has been found to be a key determinant of care-seeking behaviour for children. One possible explanation is that parents believe that problems in primary teeth are not important and that dental care should be sought only if the child has a serious problem with extreme pain.21 Similarly, in our study, the most common reason for children not visiting a dentist in the year before the survey was no perceived need reported by the parents. Because perceived need has been found to be strongly associated with symptoms of oral pain,22 oral health promotion interventions should be directed toward educating parents about non-painful oral signs and symptoms as well as the connection between children's oral health and their general health.
Many children and youth do not receive the preventive dental services recommended to reduce the incidence of caries: dental check-up, cleaning, fluoride treatment and dental sealants. In our study, the use of fluoride treatment and sealant was low compared with other dental services, even though most of the participants were aware of the coverage for this service. Similarly, a recent study based on data from the 2007 National Survey of Children's Health demonstrated that a significant proportion of children in the United States do not receive the recommended level of preventive dental care.21 The survey also found a significant association between parents' report of their child's oral health needs and dental visits for preventive care. Overall, use of preventive dental care was found to be below national targets.21 A possible explanation for the underuse of preventive dental care for children is that some parents have an "illness reaction" approach23 instead of a health promotion or disease prevention approach.24 For these parents, taking remedial action after a problem is perceived will be their main motivation for seeking professional care. It is worth mentioning that sealants are still underprescribed by dental professionals, which may be a reason for low use of this preventive modality by Alberta health benefit plan clients.
Dental insurance can play an important role in promoting optimal use of dental services. However, in our study, many clients of the Alberta Child Health Benefit Plan reported that children were the only members in the family who enjoyed the benefits of dental insurance coverage because parents were not eligible. Some parents complained that the coverage was insufficient and did not include some procedures, such as root canals and orthodontic treatment. In fact, insufficient coverage was the most common difficulty reported by dental care users. Similar concerns were reported in a recent qualitative study, in which parents whose children needed services that were not covered by their health insurance expressed a great deal of concern about the impact that unattended oral health problems had on their children's overall health and quality of life.12
Many of the non-users of dental services in our study also reported insufficient coverage as a reason for not seeking dental services for their children, in many cases because of their lack of knowledge about the benefit program and the complexity of the health care system. Increasing oral health literacy among low-income families by teaching them how to navigate the health care system, including health insurance, may increase the use of dental services covered by publicly funded programs. For example, community-based programs could be provided with information about health benefit programs and dental coverage to provide to parents who have little experience with the dental health care system.
One of the limitations of this study was that we were unable to validate parents' reports of their children's use of dental services. Although self-reported dental use has been shown to be validated among adults,25 parent recall of children's dental use may be less accurate. In addition, although the survey was mailed to randomly selected clients, those who chose to reply were more likely to have used the covered dental services than non-respondents; therefore, the actual utilization rate might be lower than we report here.
Conclusions
Although dental insurance was considered to be a factor enhancing the use of dental services by our participants, children underused the available dental benefits. We found parental perceived need to be the primary determinant of use of dental care services for this group of insured children. Awareness of the coverage did not increase the use of preventive measures for young children. Therefore, oral health promotion interventions should be directed at enhancing perception of the need for preventive services to prevent the onset of dental problems or to detect them at an early stage. Dental professionals should encourage their patients to adopt preventive measures including regular dental visits. To raise awareness of the importance of preventive services, sufficient dental coverage for preventive and restorative care must be provided, particularly to children at greater risk of developing dental diseases. More in-depth investigation on the impact of public insurance on use of dental services for young children is recommended.
THE AUTHORS
References
- Oral health in America: a report of the surgeon general (executive summary). Rockville, MD: US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health, 2000 [accessed 2014 Jun 9]. Available: www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/sgr/execsum.htm.
- Patrick DL, Lee RS, Nucci M, Grembowski D, Jolles CZ, Milgrom P. Reducing oral health disparities: a focus on social and cultural determinants. BMC Oral Health. 2006;6(Suppl 1):S4.
- Donaldson AN, Everitt B, Newton T, Steele J, Sherriff M, Bower E. The effects of social class and dental attendance on oral health. J Dent Res. 2008;87(1):60-4.
- Ettinger RL, Mulligan R. The future of dental care for the elderly population. J Calif Dent Assoc. 1999;27(9):687-92.
- Muirhead VE, Quiñonez C, Figueiredo R, Locker D. Predictors of dental care utilization among working poor Canadians. Community Dent Oral Epidemiol. 2009;37(3):199-208.
- Bedos C, Brodeur JM, Benigeri M, Olivier M. [Utilization of preventive dental services by recent immigrants in Quebec]. [Article in French] Can J Public Health. 2004;95(3):219-23.
- Duncan RP, Gilbert GH, Peek CW, Heft MW. The dynamics of toothache pain and dental services utilization: 24-month incidence. J Public Health Dent. 2003;63(4):227-34.
- Edelstein BL. Disparities in oral health and access to care: findings of national surveys. Ambul Pediatr. 2002;2(2 Suppl):141-7.
- Bhatti T, Rana Z, Grootendorst P. Dental insurance, income and the use of dental care in Canada. J Can Dent Assoc. 2007;73(1):57.
- Seiber EE, Mariotti A. Differences in use of dental and medical services by noninstitutionalized children in Ohio. J Am Dent Assoc. 2011;142(3):302-8.
- Schulz AJ, Williams DR, Israel BA, Lempert LB. Racial and spatial relations as fundamental determinants of health in Detroit. Milbank Q. 2002;80(4):677-707, iv.
- Cortés DE, Réategui-Sharpe L, Spiro III A, García RI. Factors affecting children's oral health: perceptions among Latino parents. J Public Health Dent. 2012;72(1):82-9.
- Fisher MA, Mascarenhas AK. Does Medicaid improve utilization of medical and dental services and health outcomes for Medicaid-eligible children in the United States? Community Dent Oral Epidemiol. 2007;35(4):263-71.
- Quiñonez C, Locker D, Sherret L, Grootendorst P, Azarpazhooh A, Figueiredo R. An environmental scan of publicly financed dental care in Canada. Ottawa, ON: Health Canada, 2005.
- Mofidi M, Rozier RG, King RS. Problems with access to dental care for Medicaid-insured children: what caregivers think. Am J Public Health. 2002;92(1):53-8.
- Increasing access to Medicaid dental services for children through collaborative partnerships. Chicago, IL: American Dental Association, March 2004.
- Amin MS. Utilization of dental services by children in low-income families in Alberta. J Can Dent Assoc. 2011;77:b57.
- Birch S, Anderson R. Financing and delivering oral health care: what can we learn from other countries? J Can Dent Assoc. 2005;71(4):243,243a-d.
- Nelson LP, Getzin A, Graham D, Zhou J, Wagle EM, McQuiston J, et al. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent. 2011;33(1):29-36.
- Romaire MA, Bell JF, Huebner CE. Variations in children's dental service use based on four national health surveys. Pediatrics. 2012;130(5):e1182-9.
- Bell JF, Huebner CE, Reed SC. Oral health need and access to dental services: evidence from the National Survey of Children's Health, 2007. Matern Child Health J. 2012;16(Suppl 1):S27-34.
- Slaughter A, Taylor L. Perceptions of dental care need among African-American elders: implications for health promotion. Spec Care Dentist. 2005;25(3):158-63.
- Amin M, Perez A. Is the wait-for-patient-to-come approach suitable for African newcomers to Alberta, Canada? Community Dent Oral Epidemiol. 2012;40(6):523-31.
- Roden J. Capturing parents' understanding about the health behaviors they practice with their preschool-aged children. Issues Compr Pediatr Nurs. 2003;26(1):23-44.
- Gilbert GH, Rose JS, Shelton BJ. A prospective study of the validity of data on self-reported dental visits. Community Dent Oral Epidemiol. 2002;30(5):352-62.



