ABSTRACT
Objective: Some pregnant women may be at increased risk of poor oral health. A publicly funded prenatal dental program in Vancouver, British Columbia, called Healthiest Babies Possible (HBP), has been providing oral health education and limited clinical services for over 20 years to low-income women assessed to be at high risk of preterm or low-weight births. This report is an assessment of the initial outcomes.
Methods: A prospective before–after evaluation of a non-probability convenience sample of women was undertaken over 1 year (2005–2006). Participants were seen at the customary 2 clinic visits, and were asked to return for a postnatal visit. Data collected by an inside evaluator, the program’s dental hygienist, included questionnaires, semi-structured interviews, observations, clinical indices, appointment statistics and self-reports. Univariate and bivariate analyses (Student’s t test and ANOVA) were performed.
Results: Of the 67 women in the sample, 61 agreed to participate; 36 (59%) attended all 3 appointments at the clinic, and 40 (66%) completed all 3 interviews and questionnaires either at the clinic or by telephone. Clinical indices of gingival health improved significantly over the time of the evaluation. Improvements in tooth cleaning were demonstrated by a significant decrease in plaque (p < 0.001). The proportion of the women’s other children receiving professional dental care increased significantly (p < 0.001). Oral health knowledge improved and, overall, women expressed satisfaction with the program.
Conclusion: Participants in this evaluation demonstrated improved gingival health, enhanced knowledge of oral health and positive tooth-cleaning behaviour. These women pursued infant oral care and sought professional dental visits for their children.
Introduction
Some pregnant women may be at increased risk of poor oral health for a variety of reasons.1,2 If this concern is not addressed, the risks of maternal transmission of “cavity causing” bacteria to the infant, progression of periodontal disease and, possibly, adverse pregnancy outcomes are increased.1,2 However, prenatal dental programs have been reported to be effective in improving oral health outcomes during pregnancy, most likely because women are particularly receptive to health education interventions at that time.3–6
In Canada, most dental public health programs with a prenatal component focus on oral health counselling. Unfortunately, only pregnant women who can afford dental services receive needed professional dental care. Low-income pregnant women face great difficulty in obtaining dental services, as dental public health programs for adults are limited in availability and accessibility.
In British Columbia, only 1 publicly funded prenatal dental program provides clinical, in addition to educational, services. This program has operated in Vancouver for over 20 years at a dental public health clinic whose main priority is the provision of services to low-income children. Referrals of pregnant women to the prenatal dental program are from Healthiest Babies Possible (HBP), a city-wide program for low-income women at high risk of preterm or low-birth-weight pregnancies or both. In addition to low income, factors that enable a pregnant woman’s participation in the HBP program include history of substance abuse, young age, refugee or new immigrant status and Aboriginal heritage.7
Women in the HBP program are referred to the dental program if they self-report a dental concern or have not had a dental visit for over 2 years. Twelve to 15 clinic appointments a month are allocated to these women. Each woman customarily receives 2 free 1-hour clinic appointments that include an oral examination, limited clinical hygiene services and oral health counselling. If additional dental services are required, a client is given a list of dental offices offering treatment at reduced cost. According to a 2004 HBP internal report, since 1986, over 1600 women had been served by the HBP dental program.
Other than appointment monitoring, no formal assessment or evaluation of the HBP dental program has been carried out. As a first step in that direction, an evaluability assessment was conducted to establish a feasible evaluation framework.8 This is a systematic process that consists of describing the program structure (i.e., objectives, logic, activities and performance indicators) and determining its plausibility and feasibility in terms of achieving the program objectives, its suitability for intensive evaluation and its acceptability to program managers, program operators and policymakers.9 An evaluability assessment clarifies program intent, identifies areas for improvement, determines if and where evaluation is warranted and identifies a feasible evaluation design.10,11 Identification of stakeholder interest, awareness and objectives for the program and a description of the program theory are the 2 primary outcomes of such an assessment.12
A logic model was developed to depict the theory of the HBP dental program.8 A logic model is a visual schematic that illustrates the relations between contextual factors and program inputs and outcomes.13,14 It is similar to hypothesis testing in basic science research and describes the “nuts and bolts of the program.” The logic model provides a general framework for describing the rationale and logic process behind decision making that organizations, individuals or groups may follow.15
As a result of the evaluability assessment, descriptive and process evaluations of the HBP dental program were conducted.8 The Precede–Proceed Health Promotion Planning and Program Evaluation Model guided the evaluation framework.14,16 Application of these models to the HBP dental program drew attention to the multiple factors (predisposing, enabling, reinforcing) influencing the clients’ oral health outcome. This report is limited to an assessment of the most immediate outcomes of the HBP dental program regarding gingival health, oral health knowledge and client satisfaction.
Methods
A prospective outcomes evaluation with a follow-up period of 1 year was undertaken as part of the overall evaluation of the HBP dental program. A before–after method was chosen, as comparison with a control group was not feasible given the uniqueness of the program and the clientele. The study was approved by the University of British Columbia’s Behavioural Research Ethics Board and Vancouver Coastal Health Research Institute. The evaluator was the program’s dental hygienist (DL), who had 15 years of clinical experience.
From February to September 2005, a pilot study was carried out to determine the feasibility of recruiting participants who would return for a follow-up postnatal visit; recruitment for the evaluation began in October 2005. Almost 78% (15) of the 19 women in the pilot study agreed to participate, but only 33% (5 of the 15) returned for a postnatal visit. It was apparent that ongoing communication with clients would be challenging because their contact information was inadequate; therefore, better quality and more detailed contact information was obtained before beginning the formal evaluation. Additional measures adopted to increase attendance at the postnatal visit included mailing birth congratulation cards and telephoning each woman after delivery. A thank-you gift package was given to each returning participant at their postnatal visit.
Questionnaires were tested in the pilot study, revised and reviewed for clarity and comprehension by clients and staff. Various clinical indices were pretested on clients for ease of use, time efficiency and “client-friendliness.”
A reasonable sample size was determined to be 40, which was the usual number of new clients seen in a year. The sampling frame was a non-probability convenience sample comprising women referred from the umbrella HBP program to the HBP dental program. Further inclusion criteria were stage of pregnancy (< 35 weeks gestation) and commitment to the evaluation encounters (interviews, questionnaires and clinical assessment).
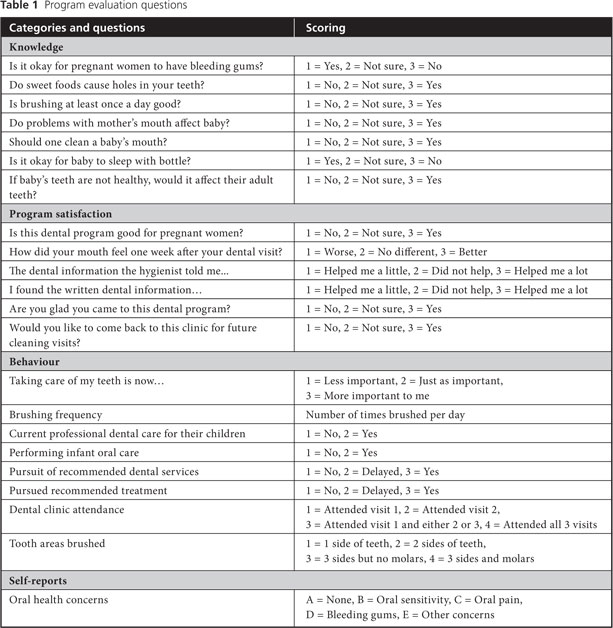
Figure 1 outlines the activities undertaken at the 3 clinic visits. In Table 1, items from the outcomes questionnaire and interview are grouped into categories, such as oral health knowledge, home care behaviours and satisfaction with the program. All handouts were at a 4th grade readability level. Table 2 shows participant demographics, including their oral health concerns and needs.
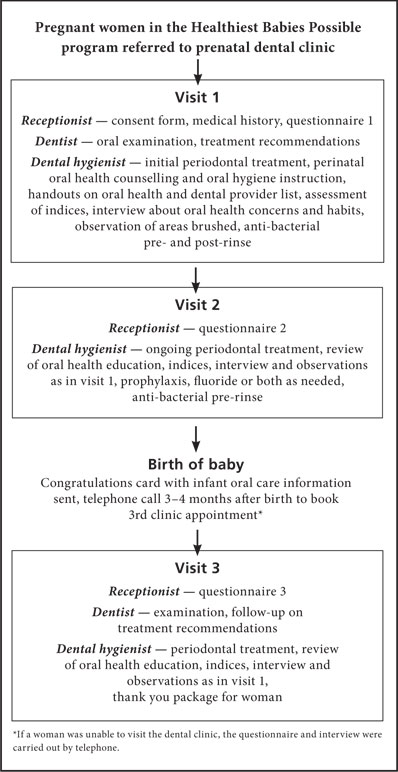 Figure 1: Outcomes evaluation flowchart
Figure 1: Outcomes evaluation flowchart

Clinical measurements were selected for ease of use, patient comfort and simplicity. A modified version of Ramfjord’s periodontal disease index for calculus, plaque and gingival status was applied to 6 teeth. Periodontal pocket depth was defined as the deepest measurement using a standard pressure-sensitive probe (KerrHawe Click-Probe, Kerrhawe SA, Bioggio, Switzerland), the ideal measurement being 0. Absence of or decrease in bleeding on probing was an indicator that gingival health had improved.18 Participants were examined by the attending dentist for visible decay, treatment needs and ideal timing for this treatment (before or after birth of child). Shorter-term outcomes were evaluated by comparing prenatal visits 1 and 2. Medium-term outcomes were assessed by comparing prenatal visit 1 with postnatal visit 3.
Univariate descriptive statistical analysis, bivariate analysis (χ2 test or Fischer exact test), Student’s t test and ANOVA with post hoc Bonferroni adjustment were carried out. Reliability testing (Cohen kappa, intra-class correlation) was performed for self-reports and clinical indices. For all tests, the threshold for statistical significance was set at p < 0.05.
Results
Of the 67 women who attended the program over the 1-year period, 61 (91%) consented to participate in the evaluation. The main reasons for non-participation were uncertainty about future residency or difficult personal circumstances.
The participants originated from 18 countries and spoke 15 different languages; 87% of the women had no dental insurance (Table 2). Their mean age (SD) was 27.7 (± 5.0) years. The median number of pregnancies was 2 and mean gestational stage at visit 1 was 22.8 (± 5.2) weeks. Average time between screening and visit 1 and between visits 1 and 2 was 4 weeks. The average time between visit 2 and postnatal visit 3 was 41 weeks (range 31–70 weeks). Of the 61 women, 50 (82%) attended the 2 prenatal clinic visits, 36 (59%) attended all 3 clinic visits and 40 (66%) completed all 3 interviews and questionnaires.
Postnatal data available from the HBP prenatal coordinator revealed that mean gestational week at delivery was 39.3 (± 1.2) and mean birth weight was 3328 (± 458.1) grams. Only 1 participant delivered a preterm, low-birth-weight baby; 2 women had babies who weighed less than 2500 grams, but were not preterm.
The reliability (Cohen kappa) of repeated questions and self-reports varied from 0.62 to 1.00; for clinical indices, it ranged from 0.66 to 1.00. Thus, all measurements were considered of “substantial to almost perfect” reliability.19 The reliability of the gingival and bleeding-on-probing indices were high to very high reliability (0.538–0.710 intra-class correlation).20
Of the 40 women for whom complete questionnaire data were obtained, 30 (75%) needed further dental treatment but only 7 (23% of the 30) received it. Figure 2 shows self-reported oral health concerns during the 3 encounters.
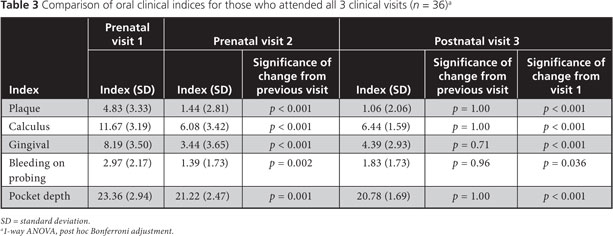
In Table 3, participants’ gingival health and plaque indices are compared over time. Gingival indices improved significantly between visits 1 and 2 and between visits 1 and 3. Substantial improvement in tooth cleaning ability by visit 2 was demonstrated by improved plaque indices, which were maintained at the postnatal visit 3 (p < 0.001).
 Figure 2: Oral concerns reported by clients who completed all 3 interviews and questionnaires (n = 40).
Figure 2: Oral concerns reported by clients who completed all 3 interviews and questionnaires (n = 40).
+ Significantly different (p 0.05) compared with visit 1 (χ2 test).
Oral health knowledge improved significantly. For example, more women understood that bleeding is not normal during pregnancy (p < 0.001) and that baby should not sleep with a bottle (p = 0.019). The proportion of participants’ other children receiving professional dental care increased significantly (p < 0.001) and 93% (40/43) of the participants interviewed postnatally reported performing infant oral care.
Of the 51 women who completed the first 2 interviews and questionnaires, 45 (88%) indicated that they found oral health information to be “very helpful” especially when it was provided verbally by the dental hygienist. Forty-eight (94%) reported that their mouth felt better after visit 1 and 41 (80%) indicated that taking care of their teeth had become more important to them since they had been participating in the HBP dental program. Overall satisfaction with the program was reported by all the women, and all those who attended follow-up visits indicated that they would like to return to the clinic for future visits. Suggestions for improving the program included more flexible hours, more frequent follow-up and provision of a dental check-up for baby when teeth erupt.
Discussion
Evaluation of the HBP dental program revealed improvements in behaviours, skills, knowledge and gingival health. The evaluator’s observation of improved tooth cleaning was supported by improved plaque indices. The participants’ enhanced skills, together with the program’s modest clinical intervention (superficial periodontal debridement), likely led to the women’s improved gingival health. Their improved tooth cleaning technique may have been a result of a combination of the recommendation of a smaller, easier-to-use toothbrush, one-to-one oral hygiene instruction and decreased gingival sensitivity to brushing after debridement.
The increase in the number of clients seeking professional dental care for their other children was a positive outcome that may have occurred for a variety of reasons: encouragement from the hygienist, women’s new awareness of the accessibility of pediatric care at the clinic, their greater comfort in bringing other children for care after their own positive experience and their newly acquired knowledge about the importance of baby teeth.
An encouraging finding was that, despite the challenges of life with a newborn, most mothers reported attending to infant oral care practices. There was general improvement in knowledge; for example, mothers learned about the influence of their oral health on that of their babies and that bleeding gums are not a normal part of pregnancy. The improved behaviour and knowledge outcomes of this program generally reflect the receptivity of pregnant women to new health knowledge.3–6
Both oral pain and bleeding had decreased by visit 2; however, reports of oral pain increased at visit 3. Although this was troubling, it likely occurred because few women received the recommended “needed” dental treatment because of financial barriers and other issues of access to care. Mothers’ responsibilities for their new babies probably afforded them less time to address personal care needs, including oral self-care.21
Individual patient counselling combined with translated handouts appeared to be reasonably effective in relaying information that led to positive behaviours across diverse cultural backgrounds, despite some language barriers. The positive provider–client relationship that developed over time promoted behaviour change.22,23 Not surprisingly, information delivered verbally was felt to be more helpful than written information in pamphlets. This finding is well documented in health education literature.23
It is important to mention the limitations of this program evaluation and consider some of the usual cautions related to observational data.24 Ways to minimize observer bias and maximize consistency include using trained observers, systematic data collection methods and unobtrusive observers.25 In this study, consistency was enhanced because one experienced, trained examiner made all the assessments. However, the positive outcomes of this program may have been heightened by a bias in self-selection by more motivated clients who attended all 3 visits or completed all 3 interviews and questionnaires.26
Inside evaluators conduct an estimated 50%–75% of program evaluations in North America.12 Disadvantages of insider evaluation include lack of objectivity and ambiguity surrounding the dual role. However, there is growing support for and acknowledged benefits of insider evaluation.27–29 Some advantages include familiarity with and access to the organization and program, the ability to observe implementation of evaluation recommendations, rapport with staff, the ability to communicate evaluation findings frequently and the ability to provide staff with a better understanding of activities and findings.12 Concerns with insider evaluation27,28,30 can be minimized by adhering to appropriate methods, ensuring validity of measurement instruments and paying attention to evaluation frameworks as well as to the American Evaluation Association guiding principles of systematic inquiry, competence, integrity/honesty, respect for people and responsibility for general and public welfare.12,31,32 Although an external evaluator would enhance the validity of the insider evaluation process,12,31 the cost of hiring an external evaluator can be prohibitive for chronically underfunded public health programs that prefer to spend dollars on services.
Results of the outcomes assessment cannot be easily generalized to the entire group of HBP clients, as the cohort of participants was a voluntary convenience sample. Retention of a “transient” clientele for the duration of the study was indeed challenging. However, the fact that 66% (40/61) of the women followed for 1 year participated in some sort of longer-term follow-up adds credibility to the findings.
Ideally, the 2-visit program should be extended into the postnatal period. An enhanced program might include postnatal telephone follow-up (after 3 months) to reinforce infant oral care messages and the need for an early dental visit. Oral health programs focusing on this early postnatal period have an important role in controlling early childhood caries, as behaviours that promote child dental health are established in infancy and early childhood.33 An economic analysis of the program should also be considered.
Conclusion
Women who participated in this evaluation of the HBP dental program demonstrated improved gingival health, enhanced knowledge of oral health and positive tooth cleaning behaviours. They pursued infant oral care and sought professional dental visits for their other children.
THE AUTHORS
References
- Jeffcoat MK, Geurs NC, Reddy MS, Cliver SP, Goldenberg RL, Hauth JC. Periodontal infection and preterm birth: results of a prospective study. J Am Dent Assoc. 2001;132(7):875-80.
- Zanata RL, Navarro MF, Pereira JC, Franco EB, Lauris JR, Barbosa SH. Effect of caries preventive measures directed to expectant mothers on caries experience in their children. Braz Dent J. 2003;14(2):75-81. Epub 2003 Oct 3.
- Günay H, Dmoch-Bockhorn K, Günay Y, Geurtsen W. Effect on caries experience of a long-term preventive program for mothers and children starting during pregnancy. Clin Oral Investig. 1998;2(3):137-42.
- Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R. Oral health during pregnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc. 2001;132(7):1009-16.
- Gomez SS, Weber AA. Effectiveness of a caries preventive program in pregnant women and new mothers on their offspring. Int J Paedtri Dent. 2001;11(2):117-22.
- Gomez SS, Weber AA, Emilson CG. A prospective study of a caries prevention program in pregnant women and their children five and six years of age. ASDC J Dent Child. 2001;68(3):191-5, 152.
- Healthiest Babies Possible Program. Annual report 2004. Vancouver, BC: Vancouver Coastal Health; 2004.
- Lin DL, Harrison R. Evaluability assessment of a dental prenatal program. Can J Dent Hygiene. 2010;44(5):201-6.
- Smith MF. Evaluability assessment: a practical approach. Norwell, Mass.: Kluwer Academic; 1989.
- Juvenile Justice Evaluation Center. Evaluability assessment: examining the readiness of a program for evaluation (Program evaluation briefing series). Washington, DC: Justice Research and Statistics Association; 2003. Available: www.jrsa.org/pubs/juv-justice/evaluability-assessment.pdf (accessed 2011 March 15).
- Ovretveit J. Action evaluation of health programmes and changes: a handbook for a user-focused approach. Abingdon, U.K.: Radcliffe Medical Press; 2002.
- Mathison S, editor. Encyclopedia of evaluation. Thousand Oaks, Calif.: Sage Publications; 2005.
- Logic model development guide. Battle Creek, Mich.: W.K. Kellogg Foundation; 2004. Available: www.wkkf.org/knowledge-center/resources/2010/Logic-Model-Development-Guide.aspx (accessed 2011 March 15).
- Centers for Disease Control and Prevention. Framework for program evaluation in public health. MMWR 1999;48(RR-11):1-40. Available: www.cdc.gov/mmwr/preview/mmwrhtml/rr4811a1.htm (accessed 2011 March 15).
- Chiappelli F, Cajulis OS. The logic model for evidence-based clinical decision making in dental practice. J Evid Based Dent Pract. 2009;9(4):206-10.
- Green LW, Kreuter MW, editors. Health promotion planning: an educational and ecological approach. 3rd ed. Mountain View, Calif.: Mayfield Publishing; 1999.
- Standard country and area codes classification. New York: United Nations Statistics Division. Available: unstats.un.org/unsd/methods/m49/m49regin.htm (accessed 2011 March 15).
- Darby ML, Walsh MM. Dental hygiene theory and practice. 2nd ed. Philadelphia: WB Saunders; 2003.
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-74.
- Hopkins WG. Effect statistics. In: A new view of statistics. Web site of WG Hopkins; 2009. Available: sportsci.org/resource/stats/index.html (accessed 2011 March 15).
- Redford M. Beyond pregnancy gingivitis: bringing a new focus to women's oral health. J Dent Educ. 1993;57(10):742-8.
- Weinstein P, Harrison R, Benton T. Motivating parents to prevent caries in their young children: one-year findings. J Am Dent Assoc. 2004;135(6):731-8.
- Weinstein P, Harrison R, Benton T. Motivating mothers to prevent caries: confirming the beneficial effect of counseling. J Am Dent Assoc. 2006;137(6):789-93.
- Kerlinger FN. Foundations of behavioral research. 3rd ed. Fort Worth, Tex.: Holt, Rinehart and Winston; 1986.
- Hodges BC, Videto DM. Assessment and planning in health programs. Sudbury, Mass.: Jones and Bartlett; 2005.
- Harrison RL, Wong T. An oral health promotion program for an urban minority population of preschool children. Community Dent Oral Epidemiol. 2003;31(5):392-9.
- Klein N, Johnston M. Insider-out: the health worker as researcher. Nurs Res. 1979;28(5):312-4.
- Bonner A, Tohurst G. Insider-outsider perspectives of participant observation. Nurs Res. 2002;9(4):7-19.
- Shaw I, Faulkner A. Practitioner evaluation at work. Am J Eval. 2006;27(1):44-63.
- Minkler M. Ethical challenges for the “outside” researcher in community-based participatory research. Health Educ Behav. 2004;31(6):684-97.
- King JA, Morris LL, Fitz-Gibbon CT. How to assess program implementation. 2nd ed. Thousand Oaks, Calif.: Sage Publications; 1987.
- American Evaluation Association. Guiding principles for evaluators. Fairhaven, Mass.; 2004. Available: www.eval.org/publications/guidingprinciples.asp (accessed 2011 March 15).
- Ismail AI. Prevention of early childhood caries. Community Dent Oral Epidemiol. 1998;26(1 Suppl):49-61.
