ABSTRACT
Over the last 40 years, the proportion of women in dentistry has been rising steadily, raising questions about the effects of this feminization on the profession. A review of the literature, although limited, highlights potentially important areas related to gender, including impact on work hours, practice models, professional incomes, the dentist–patient relationship, clinical philosophies, specialty practice, academia and leadership. Although cohorts of predominantly female dentists are only beginning to enter the workforce and, thus, it is difficult to predict the long-term effects, some trends are evident: women are less likely than men to own their practice; women may work 4–6 fewer hours a week and see fewer patients; there is a pay differential; female general practitioners and specialists appear more likely to work in urban centres; and women are less prominent in the specialties, academia and leadership roles. Thus, the profession may shift toward less entrepreneurship, more urbanization and, possibly, fewer clinical hours available to the population as a result of feminization. With the ultimate goal of excellence in patient care, this may entail increases in student enrolment, formal incentives for practice relocation to rural communities, more business education and policies to modify advanced education and training for women with children. This knowledge, although still not robust, is relevant for policy, educational institutions and professional governing bodies.
Introduction
Dentistry is a profession dominated by men. Women have been making significant inroads only since the 1970s,1 as a result of professional initiatives and women’s movements, raising questions about the effects of feminization on dentistry, defined as an increase in female presence and a corresponding shift in the occupation.1,2 Although most practising dentists in North America are men, this will soon change. In Ontario, 16% of dentists were women in 1991, 28% in 2005 and, in 2010, the majority of dental students in North America were female.2
Will this shift be paralleled by changes to the profession? Some speculate that feminization will have significant implications in terms of labour supply, practice characteristics and professional ideals.1-5 With different societal and familial pressures, will female dentists have different goals and expectations? How will this affect patient care? Despite minimal data in Canada, a literature review highlights important areas, including impacts on work hours, practice models, professional incomes, the dentist–patient relationship, clinical philosophies, specialty practice, academia and leadership.
Demographics
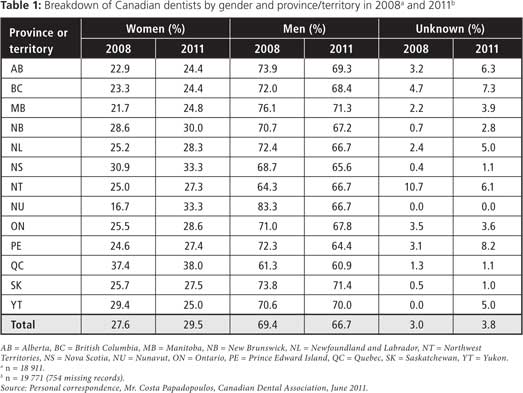
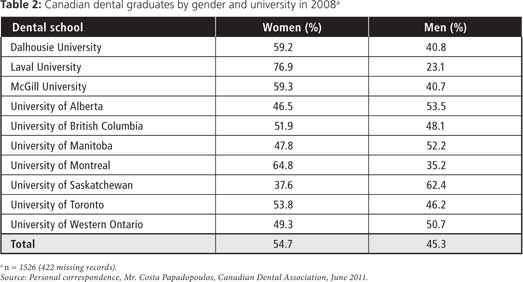
In 2008, the proportion of female dentists in Canada ranged from 16.7% to 37.4%, with a mean of 27.6%; in 2011, the range was 24.4% to 38.0%, with a mean of 29.5% (Table 1). In 2008, 6 of 10 Canadian dental faculties had more female graduates than male (Table 2). Annual data for multiyear comparisons were not available, nor were provincial data on the gender of foreign-trained dentists graduating from Canadian institutions. Although in 2008 Ontario had the most graduates from any advanced standing degree program in Canada (32–41 graduates/year),6 in 2001, 34% of female dentists in Ontario were foreign-trained versus 15% of men.2
Work Hours
Among the most cited differences between male and female dentists has been the claim that women work less. The average length of the career of a female dentist in Canada is 20 years v. 35 years for men, potentially creating future shortages as more women enter the profession.3 In New Zealand, for example, two-thirds of male dentists plan to retire after age 60, whereas two-thirds of female dentists plan to retire before that age.7 United States labour statistics reveal that, among dentists younger than 55 years of age, 96% of men v. 90% of women are still working.4
The 2006 Canadian census indicated that male dentists in Ontario average 39.5 hours/week and 47.2 weeks/year, whereas female dentists work 35.6 hours/week and 44.7 weeks/year.8 In contrast, when work hours per year were analyzed in a 2002 survey of Ontario dentists, no overall differences were found.2 Gender differences were only evident for the youngest cohort: 39.2 hours/week for men v. 35.5 hours/week for women (or 5 fewer weeks of work per year). A study in Washington State5 found that female dentists, particularly those aged 25–40, work 10% fewer days, treat 10% fewer patients and perform 10% fewer procedures; based on these figures, for every 5% increase in female dentists, 1.2% (15 000) fewer patients would be treated annually. Other research also shows that female dentists see fewer patients annually.9 The US labour statistics4 indicate that, from 1986 to 1999, 30% of women v. 14% of men worked part-time (i.e., < 32 hours/week), and 16% of women v. 30% of men worked more than 42 hours/week. A 2011 US study10 found significantly more male dentists (89%) working full-time than women (75%).
Adams2 reported that marital status and children may influence the observed difference in work hours between the sexes. Her Ontario study of dentists found that women aged 25–37 work 3.5–6 hours/week less than men. Unmarried female dentists work the same hours as men, and those in the 32–37 and 48+ age brackets work more.2 A US study4 reported that marital status of women, controlling for children, has no impact on work hours; for male dentists, marriage adds 1 hour/week of work. However, having children reduces women’s work time by 7 hours/week, while it has no impact on men. A physician study reported that women perform 67% of childcare and household duties, compared with 19% of childcare and 26% of household duties for men,11demonstrating that household organization affects work hours. A survey in the United Kingdom found that 50% of female dentists work 2 or fewer days/week, mainly because of childcare responsibilities (65%).12,13
Practice Model
Some speculate that men and women practise differently. In a US survey,10 74% of men were the owner or partner in a practice v. 54% of women. In Ontario, the 2006 Canadian census indicated that 83% of male dentists are self-employed (57% unincorporated, 26% incorporated) v. 63% of women (48% unincorporated, 15% incorporated), whereas 17% of male dentists work as employees v. 37% of women.8 Another Ontario study reported that 55% of men work in solo practice v. 35% of women.2 It also found that male dentists in solo and group practice employ more staff than female dentists.2 Women are also more likely to work as associates (27.2% v. 9.2% of men), especially those in the youngest cohort (46% v. 22.9%).2 Similarly, a New Zealand survey found that 47.7% of women work as associates compared with 22.3% of men.7 Women are almost twice as likely as men to work in a hospital setting (13.1% v. 7.6%). This situation is also observed in pharmacy, which has also seen an influx of women, with more women working for hospitals and corporate pharmacies than independent practice.1 Female dentists are also more likely to work in urban centres than men.4,14
Income
In 2000, female Ontario dentists made an average of $84 655 a year compared with $145 304 for men.2 This 58% difference may be attributed to the greater proportion of women working as associates. A study of Washington State dentists5 found that women’s total annual income is 10% less ($17 761) than men’s; however, they treat 10% fewer patients, perform 10% fewer procedures, treat a higher proportion of pediatric patients and are 7.9 years younger. No differences were found in terms of income or number of procedures per patient. Another study found that after controlling for factors affecting income (practice ownership, age, work hours), US female dentists have a mean net income 22% below that of men ($95 410 v. $121 640).15
Dentist–Patient Relationship
Some argue that female dentists have different traits, including more empathy and better communication skills.16-18 Female dentists are perceived as less rushed, more likely to discuss ailments with patients and more humane and caring.18 A comparison of full-time male and female dentists revealed no differences in the number of patients they see per week or the number of days patients wait for appointments.10 In terms of decision-making, female dentists have been reported to make decisions more based on “feeling” (personal values, maintenance of harmony, sympathy and tact) than men, who base decisions more on “thinking” (logic, consistency, objectivity).17 Female dental students have been found to have better social skills, to be more emotionally expressive and sensitive, more verbally expressive and more responsive to patient needs, whereas men have better emotional control.16 In addition, male dentists (46%) have been perceived as more likely to expect the patient to endure pain compared with female dentists (8%).18
There is also evidence that male and female dentists are more alike than dissimilar.17,19 A survey of Canadian dentists19 revealed that the sexes do not differ in their attitude toward pro bono care, nor in a variety of opinions regarding publicly financed dental care. A US study10 reported no differences between male and female dentists in the number of treated patients with insurance.
Clinical Philosophies
Evidence suggests that male and female dentists vary in their approach to clinical practice. A number of studies show that compliance with infection control is different: men are less likely to use gloves, masks and protective eyewear, and suffer more sharps injuries.20 Another study found that female dentists favour a more preventive philosophy, take a more conservative approach to restoration and encourage more preventive strategies in the early stages of caries.10 Male dentists have been reported to intervene more often in the case of enamel lesions in low-risk patients.21 Female dentists have been found to be more attuned to secondary prevention of eating disorders than male dentists.22 One study9 also reported that female dentists are more likely to refer patients to specialists for large multi-unit fixed cases, single- and multi-root endodontics, surgical extractions, periodontal surgery, maxillofacial pathology and implants. Female dentists have been found to refer patients more frequently: 70.3% of simple and complex surgical cases involving medically compromised patients v. 49.5% for male dentists.23
Specialists
In 2001, female dentists made up 23% of generalists and 14% of specialists.2 This is not reflected in medicine, where women represented 43.4% of postgraduate trainees in specialty programs in Ontario in 2009.24 With the influx of women into medicine in Ontario occurring much earlier (1911) than into dentistry (1950–60s),1 gender parity in that latter profession may be reached in time.
The distribution of women in specialties is also unequal, with few women choosing oral and maxillofacial surgery (OMFS) or endodontics.25 In one US study,25 61% of female OMFS respondents reported gender bias; 48% reported bias within their practice and 38% reported sexual harassment during their residency. The same survey found that marriage rates among female OMFS practitioners had decreased and divorce rates increased. A report on medical specialists in Switzerland26 indicated that gender was the strongest factor influencing specialty choice, with women underrepresented in surgical specialties.
When selecting a specialty, female dental students are more highly influenced by location and proximity to family.27 This is reflected in the uneven distribution of specialists in Ontario, with female specialists more likely to work in urban (61% women v. 48% men) than rural centres (0% women v. 7% men).2 Female specialists also appear to have more conservative attitudes toward professional issues (e.g., independent hygiene practices and role of insurance companies in determining dental treatment).2
The duration of specialty education conflicts with child-bearing years and is a potential reason for the specialist gender gap. Most women undertake postgraduate dental education before having children (60.7%) compared with 34.3% of men.7 More male specialists (65%) have their children before or during postgraduate training than women (21.4%). Strikingly, 17.9% of female specialists have no children v. 0.7% of men. Reduced flexibility in marital partnerships may contribute to fewer female specialists. One survey reported that half of male dentists v. a quarter of women feel their partner has made career adjustments to accommodate their career.7
Academia and Leadership
One study28 investigated the advancement of female dentists based on academic appointment, publication status and leadership within professional organizations. Among 9 dental journals, only 13% of first authors and 9% of last (senior) authors were women; 12% of publishing male dentists held both a DDS and a PhD v. 1% of women. Although the rate of publication by women has been increasing since 1986, it does not reflect the number of women entering academia or the workforce. Since the mid-1990s, there have been small increases in the number of tenured and tenure-track women in dentistry, and, from 1985 to 2006, the number of female deans increased from 2% to 18%. Among specialty organizations, the American Academy of Public Health Dentistry has had the highest proportion of female presidents (10%); 3 have never had a female president (American Association of Oral and Maxillofacial Surgery, American Association of Orthodontists and American Association of Pediatric Dentistry). A review of websites of Canadian dental organizations also reveals that few leadership positions—on boards of directors, association councils or executive committees—are held by women.
In the US, male and female dental faculty do not differ in terms of hours worked per week, time spent on research or available grant support.29 Yet, men are more likely to have office space, secretarial support, protected research time and laboratory space. Women perceive the work environment to be less welcoming and report more sexual harassment (32.7% women v. 3.4% men). Female faculty are less likely to be married or have a partner (69.3% women v. 90% men) or to have children (57% v. 87.9%) and are more likely to have fewer children (1.14 v. 2.1 children). A study of medical faculty30 reported similar findings.
Several organizations and initiatives (e.g., American Dental Education Association, Executive Leadership in Academic Medicine Program for Women) have the intention of improving the academic culture for women.31 This is important as there are still incidents of perceived and actual gender bias and harassment of women in academia.28,29,31 According to Dannels and colleagues,31 97% of deans across 29 American and 4 Canadian dental schools feel that the work environment is more positive for women today. A quarter to a third report that there is room for improvement and that policies are in place in support of female faculty: 68.8% of institutions provide benefits for part-time faculty; 46.9% have an optional delayed tenure clock and 30% have an automatic delayed tenure clock to accommodate childbirth or adoption; 40.6% have childcare facilities onsite or nearby; and 12.5% have a tenure option for part-time faculty. Of the 10 Canadian dental schools, only 1 (Laval University) has had a female dean (1995–2000).32
Discussion
Male and female dentists differ in a number of ways. Whether this has major implications for dentistry is unknown. The effects of feminization are unclear, as current data are not robust enough to draw conclusions. With many variables at play, studies controlling for such issues as age, marital status, children, ethnicity, owner v. associate practice, student v. practitioner must be performed. Nonetheless, this literature review has uncovered similar findings across a number of studies: less practice ownership by women; women work 4–6 fewer hours/week and see fewer patients; there is a pay differential; female generalists and specialists appear more likely to work in urban centres; and women are less prominent in the specialties, academia and leadership roles.
Thus, the profession may potentially shift in a direction that involves less entrepreneurship, more urbanization and, possibly, less patient inflow. In turn, this could mean future increases in student enrolment, formal incentives to engage in rural practice, more business education and policies to modify advanced education and training for women with children, to redress pay inequity and to assess institutional practices and policies.33-37
To advance our knowledge of the effects of feminization on Canadian dentistry, local data are required. Future research should include surveys of Canadian dentists to identify differences in work patterns; surveys of Canadian dental students to determine career goals and barriers; and focus groups, as elsewhere,13 to identify barriers faced by female dentists in clinical practice, academia and leadership and to identify solutions. These studies will be of importance for deans, senior administration and governing or regulatory bodies as they manage the potential changes associated with the gender shift.
THE AUTHORS
References
- Adams TL. A dentist and a gentleman: gender and the rise of dentistry in Ontario. Toronto: University of Toronto Press; 2000.
- Adams TL. Feminization of professions: the case of women in dentistry. Can J Sociology. 2005;30(1):71-94.
- Brown TA, Raborn W. Is there an adequate supply of new dentists in Canada? J Can Dent Assoc. 2001;67(7):373-4.
- Walton SM, Byck GR, Cooksey JA, Kaste LM. Assessing differences in hours worked between male and female dentists: an analysis of cross-sectional national survey data from 1979 through 1999. J Am Dent Assoc. 2004;135(5):637-45.
- del Aguila MA, Leggott PJ, Robertson PB, Porterfield DL, Felber GD. Practice patterns among male and female general dentists in a Washington State population. J Am Dent Assoc. 2005;136(6):790-6.
- Boorberg NB, Schönwetter DJ, Swain VL. Advanced placement, qualifying, and degree completion programs for internationally trained dentists in Canada and the United States: an overview. J Dent Educ. 2009;73(3):399-415.
- Ayers KM, Thomson WM, Rich AM, Newton JT. Gender differences in dentists’ working practices and job satisfaction. J Dent. 2008;36(5):343-50. Epub 1008 Mar 3.
- Abate R. A demographic update for Ontario: population and dental professionals. Ontario Dentist. 2011;June:38-43.
- Atchison KA, Bibb CA, Lefever KH, Mito RS, Lin S, Engelhardt R. Gender differences in career and practice patterns of PGD-trained dentists. J Dent Educ. 2002;66(12):1358-67.
- Riley JL 3rd, Gordan VV, Rouisse KM, McClelland J, Gilbert GH; Dental Practice-Based Research Network Collaborative Group. Differences in male and female dentists’ practice patterns regarding diagnosis and treatment of dental caries: findings from The Dental Practice-Based Research Network. J Am Dent Assoc. 2011;142(4):429-40.
- Colletti LM, Mulholland MW, Sonnad SS. Perceived obstacles to career success for women in academic surgery. Arch Surg. 2000;135(8):972-7.
- Murray JJ. Better opportunities for women dentists: a review of the contribution of women dentists to the workforce. Br Dent J. 2002;192(4):191-6.
- Seward M. Better opportunities for women dentists — a review of the contribution of women dentists to the workforce. Department of Health, London. 2001. Available: www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4005429 (accessed 2012 Jan 4).
- McCarthy GM, MacDonald JK. Gender differences in characteristics, infection control practices, knowledge and attitudes related to HIV among Ontario dentists. Community Dent Oral Epidemiol. 1996;24(6):412-5.
- Brown LJ, Lazar V. Differences in net incomes of male and female owner general practitioners. J Am Dent Assoc. 1998;129(3):373-8.
- Hannah A, Lim BT, Ayers KM. Emotional intelligence and clinical interview performance of dental students. J Dent Educ. 2009;73(9):1107-17.
- Morris DO. Personality types of dental school applicants. Eur J Dent Educ. 2000;4(3):100-7.
- Smith MK, Dundes L. The implications of gender stereotypes for the dentist–patient relationship. J Dent Educ. 2008;72(5):562-70.
- Quinonez CR, Figueiredo R, Locker D. Canadian dentists’ opinions on publicly financed dental care. J Public Health Dent. 2009;69(2):64-73.
- Ward D. Gender differences in compliance with infection control precautions. Br J Infect Control. 2004;5(1):17-9.
- Gordan VV, Bader JD, Garvan CW, Richman JS, Qvist V, Fellows JL, et al. Restorative treatment thresholds for occlusal primary caries among dentists in the dental practice-based research network. J Am Dent Assoc. 2010;141(2):171-84.
- Debate RD, Vogel E, Tedesco LA, Neff JA. Sex differences among dentists regarding eating disorders and secondary prevention practices. J Am Dent Assoc. 2006;137(6):773-81.
- Cottrell DA, Reebye UN, Blyer SM, Hunter MJ, Mehta N. Referral patterns of general dental practitioners for oral surgical procedures. J Oral Maxillofac Surg. 2007;65(4):686-90.
- Postgraduate medical trainees in Ontario 2009. The Ontario Physician Human Resources Data Centre. McMaster University, Neil Johnson. 2010. Available: www.ophrdc.org/public/download.aspx?fileType=pdf&fileName=PMTIO_2009_Final_Rev.pdf (accessed 2012 Jan 4).
- Rostami F, Ahmed AE, Best AM, Laskin DM. The changing personal and professional characteristics of women in oral and maxillofacial surgery. J Oral Maxillofac Surg. 2010;68(2):381-5.
- Buddeberg-Fischer B, Klaghofer R, Abel T, Buddeberg C. Swiss residents’ speciality choices — impact of gender, personality traits, career motivation and life goals. BMC Health Serv Res. 2006;6:137.
- Saeed S, Jimenez M, Howell H, Karimbux N, Sukotjo C. Which factors influence students’ selection of advanced graduate programs? One institution’s experience. J Dent Educ. 2008;72(6):688-97.
- Yuan JC, Lee DJ, Kongkiatkamon S, Ross S, Prasad S, Koerber A, et al. Gender trends in dental leadership and academics: a twenty-two-year observation. J Dent Educ. 2010;74(4):372-80.
- Nesbitt PE, Inglehart MR, Sinkford JC. Work environment perceptions of full-time dental educators: does gender matter? J Dent Educ. 2003;67(8):916-24.
- Foster SW, McMurray JE, Linzer M, Leavitt JW, Rosenberg M, Carnes M. Results of a gender-climate and work-environment survey at a midwestern academic health center. Acad Med. 2000;75(6):653-60.
- Dannels SA, McLaughlin JM, Gleason KA, Dolan TA, McDade SA, Richman RC, et al. Dental school deans’ perceptions of the organizational culture and impact of the ELAM program on the culture and advancement of women faculty. J Dent Educ. 2009;73(6):676-88.
- Sinkford JC, Valachovic RW, Harrison S. Advancement of women in dental education: trends and strategies. J Dent Educ. 2003;67(1):79-83.
- Bickel J, Wara D, Atkinson BF, Cohen LS, Dunn M, Hostler S, et al. Increasing women’s leadership in academic medicine: report of the AAMC Project Implementation Committee. Acad Med. 2002;77(10):1043-61.
- Carnes M, Morrissey C, Geller SE. Women’s health and women’s leadership in academic medicine: hitting the same glass ceiling? J Womens Health (Larchmt). 2008;17(9):1453-62.
- Lachapelle D, Williams JN, Emond V. Curriculum and education: a working group report. J Dent Educ. 2004;68(7 Suppl):36-40.
- Morahan PS, Voytko ML, Abbuhl S, Means LJ, Wara DW, Thorson J, et al. Ensuring the success of women faculty at AMCs: lessons learned from the National Centers of Excellence in Women’s Health. Acad Med. 2001;76(1):19-31.
- Palepu A, Herbert CP. Medical women in academia: the silences we keep. CMAJ. 2002;167(8):877-9.
