Abstract
Objective: To measure the light energy that dental students delivered to a simulated Class I restoration before training, immediately after training and 4 months after training.
Methods: Thirty-eight (38) dental students used a single light-emitting diode curing light (SmartLite iQ2, Dentsply) to cure, for 10 seconds, a simulated Class I restoration positioned in the Managing Accurate Resin Curing – Patient Simulator (BlueLight analytics inc.). The students then attended an instructional lecture and received individualized instruction on optimizing their light-curing technique. The students were retested immediately after instruction and again 4 months later (without further instruction). The irradiance and energy delivered during light-curing were calculated for each student at all 3 time points. Mean values were calculated and compared.
Results: Before instruction, the students delivered between 0.1 and 7.2 J/cm2 of energy (mean ± standard deviation [SD] 4.1 ± 1.7 J/cm2). After instruction, the same students delivered between 5.8 and 7.5 J/cm2 of energy (mean ± SD 6.7 ± 0.4 J/cm2). Analysis of variance and Fisher’s Protected Least Significant Difference tests showed that instruction with the patient simulator led to a significant improvement in the amount of energy delivered and that the students retained this information. When retested 4 months later, the students delivered between 4.2 and 7.9 J/cm2 of energy (mean ± SD 6.1 ±1.1 J/cm2). Although this was less energy than immediately after instruction, the decline was not significant (p = 0.44).
Conclusions: Provision of immediate feedback on light-curing technique and instruction on how to avoid mistakes led to a significant and lasting improvement in the amount of energy delivered by the students.
According to an American Dental Association survey, an estimated 146 million resin restorations and sealants were placed during 2005/2006.1Given that almost all of these restorations would have used light-cured resins, it can be concluded that the dental light-curing unit (LCU) has become an indispensable piece of equipment in dental offices. It therefore follows that students, dentists, hygienists and dental assistants should be taught how to properly use the LCU. Until recently, it has not been possible for clinicians, whether students and dentists, to determine how much light energy was being delivered during light-curing with an LCU. The light-curing process appears easy: simply press a button, expose the resin for a few seconds and, on the surface at least, the restoration appears fully cured. However, hardness of the surface of the restoration does not indicate adequate curing of the entire restoration. This situation is of concern, given reports that inadequate polymerization adversely affects the resin’s physical properties,2-7 reduces bond strength,3-5,8,9 increases wear and breakdown at the margins,6,7 decreases biocompatibility of the resin restoration10-12 and increases bacterial colonization of the resin in the restoration.12 Equally undesirable is the delivery of too much energy to the tooth, as this may cause thermal damage to the pulp and exposed oral tissues.13-17
The user faces many challenges during light-curing of resin restorations. For example, access to the tooth may be limited, and it is often difficult to position the tip of the LCU at 90° (perpendicular) to the resin surface. Incorrect positioning can lead to shadows and an inadequate amount of light reaching the resin. In addition, many LCUs used in dental offices do not deliver as much light as the manufacturer claims or the user thinks, because of deterioration of the light source, reflectors or filters or because of debris on the end of the light guide.18-22 A recent study,23 involving use of up-to-date and properly functioning LCUs, demonstrated that the operator’s ability to correctly use the LCU affects the amount of light that reaches the resin. More specifically, that study examined the ability of 20 dental professionals to deliver energy to simulated restorations in a dental mannequin. Even though the study participants used the same 3 LCUs on the same tooth for the same exposure time, there was a 4-fold variation in the amount of energy that they delivered.23 This wide range in clinicians’ ability to deliver the energy required to adequately cure a resin restoration may help to explain why the median longevity of direct posterior resin restorations placed in dental offices is only 6 years,24,25 even though Ferracane26 and Opdam and colleagues27 have shown that such restorations can theoretically last as long as amalgam restorations. Reduced longevity is of special concern, given that resin composite is now the primary choice for posterior restorations in many countries.26
The radiant energy (E) received by a restoration can be defined as the mathematical product of irradiance (I) and exposure time (t): E = I × t. Although resin manufacturers rarely specify the amount of energy (J/cm2) required to adequately cure their products, it is possible to calculate this energy as the product of recommended curing times (seconds) and recommended minimum irradiance (mW/cm2). Unfortunately, the typical clinician has no way of knowing how much irradiance, and thus energy, is being delivered to restorations because of the inaccuracy of dental radiometers.28,29 In addition, dental radiometers report only the irradiance at the tip end of the LCU, not irradiance or energy received by the resin restoration. It has been reported that distance can significantly affect irradiance received, as well as homogeneity of light beam, extent of resin curing and bond strengths.3,30-32 Thus, tip irradiance gives little indication of the energy that the surface of a resin restoration, typically 7 mm away from the light tip, will receive.32,33
Simulation using advanced technology has become prominent in health care, and simulators have been recognized as an important aspect of health care training.34In addition, simulators may help to identify students who need early instructional intervention.35 A recently introduced simulation device, Managing Accurate Resin Curing – Patient Simulator (MARC-PS, BlueLight analytics inc., Halifax, NS), uses a laboratory-grade spectroradiometer to accurately measure the irradiance, spectrum and energy received by simulated resin restorations in a dental mannequin.23,36
The purpose of this study was to determine the quantity of energy that dental students delivered in 10 seconds to a simulated Class I restoration. The first hypothesis was that the energy delivered by the students would be greater than the minimum 6 J/cm2 necessary to cure resins, as reported by Fan and colleagues.37 The second hypothesis was that the students would deliver more energy after receiving additional simulator-based instruction on optimal use of an LCU. The third hypothesis was that the students would retain the improved ability to use the LCU for 4 months.
Methods
Appropriate approval was obtained from the Dalhousie University Health Sciences Research Ethics Board. Thirty-eight dental students, all at the end of their first year of study, were recruited. All of the students had been taught how to use an LCU (although not with the MARC-PS system), and all had used LCUs in their preclinical courses. The irradiance and energy delivered by each student to the same simulated Class I restoration in the upper left maxillary second molar (tooth 27) in a MARC-PS unit was measured before and immediately after further light-curing instruction with the MARC-PS system. In their preclinical courses, all of the students had used a dental mannequin similar to the MARC-PS mannequin. The irradiance received was measured with a CC3 light detector (Ocean Optics, Dunedin, FL) attached by a fibre optic cable to a laboratory-grade spectrometer (USB 4000, Ocean Optics) placed at the bottom of the cavity preparation. The CC3 detector was fixed at 2 mm from the cavosurface margin and 4 mm from the cusp tip (Fig. 1). As such, the detector measured the irradiance that would be received by the top surface of the resin (i.e., 2 mm from the cavosurface margin and 4 mm from the end of the light guide). To simulate the optical characteristics of a human tooth, the maxillary molar tooth housing the detector was made from a flowable resin composite (Filtek Flow, Shade A2, 3M-ESPE, St. Paul, MN). Before use, the MARC-PS system was calibrated using an NIST-traceable (National Institute of Standards and Technology, Gaithersburg, MD) high-power light source (HL-2000-HP, Ocean Optics). The irradiance (mW/cm2) received by the detector from a SmartLite iQ2 LCU (Dentsply, Milford, DE) was measured in real time, and the energy delivered (J/cm2) was calculated automatically by the MARC software after the LCU had been used for 10 seconds. This 10-second curing time was in accordance with the manufacturer’s instructions for several resins.38 An experienced operator also tested the LCU with the MARC-PS system under ideal conditions at the beginning and end of each phase of the study to confirm that the light output remained constant.
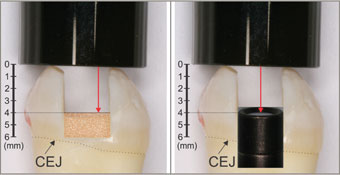 Figure 1: The detector in the maxillary second molar (tooth 27) in Managing Accurate Resin Curing – Patient Simulator simulates the position of the top surface of a resin composite in the preparation. The distance from the tip of the curing light to the top of the detector (CC3 detector, Ocean Optics) or to the top of the simulated resin surface is 4.0 mm. The proximal box is above the cementoenamel junction (CEJ).
Figure 1: The detector in the maxillary second molar (tooth 27) in Managing Accurate Resin Curing – Patient Simulator simulates the position of the top surface of a resin composite in the preparation. The distance from the tip of the curing light to the top of the detector (CC3 detector, Ocean Optics) or to the top of the simulated resin surface is 4.0 mm. The proximal box is above the cementoenamel junction (CEJ).
The students were observed as they cured the simulated restoration and any deficiencies in technique were noted for use during individualized instruction.
Following these observations, the students attended a lecture, which was followed by individual coaching and feedback using the MARC-PS system. The students were shown how easily mistakes can occur when they are using an LCU and how to optimize their light-curing technique. They were specifically instructed to wear eye protection, to look at the restoration being cured, to stabilize the light as close as possible to the restoration and to pay attention to what they were doing. The students were asked to repeat the curing process, using all of the same equipment, immediately after the instruction section and again 4 months later, just after they had completed a second-year preclinical course on placing posterior resin composite restorations. The energy delivered before and after instruction was subjected to analysis of variance followed by Fisher’s Protected Least Significant Difference (PLSD) post hoc multiple-comparison tests, with p values less than 0.01 considered significant.
To determine the theoretical maximum amount of energy that could be delivered in 10 seconds, the end of the light guide was positioned in contact with the cusp tip and perpendicular to the CC3 detector, which was 4 mm distant from the tip of the light guide. The LCU was clamped rigidly over the tooth, and the amount of light energy delivered in 10 seconds under these ideal conditions was measured. The typodont and the LCU were then repositioned and the measurements repeated 3 times. The mean of these 4 measurements was then calculated.
Results
Under ideal laboratory conditions, with the tooth and typodont fully accessible on the laboratory bench, the maximum amount of light energy that could be delivered in 10 seconds (mean ± standard deviation [SD]) was 8.0 ± 0.4 J/cm2.
Before attending the instructional lecture and demonstration on light-curing, 32 (84%) of the 38 students were unable to deliver the predefined, minimally acceptable amount of energy (6 J/cm2)37. Figure 2 illustrates the wide variation in irradiance and energy delivered by the students before instruction. It was noted that students who consistently delivered a low amount of energy did not wear the orange protective eyeglasses that were readily available, did not look at the preparation when using the LCU, did not stabilize the LCU tip with one hand and did not pay sufficient attention to what they were doing when using the LCU.
After additional instruction on optimal use of the LCU and one practice session with the MARC-PS system, the amount of energy delivered by the 38 students increased significantly, from 4.1 to 6.7 J/cm2(p < 0.01, Fisher’s PLSD) (Figure 3, Table 1), and 36 (95%) of the students delivered at least 6 J/cm2. Four months later, the students were tested again with the MARC-PS system. During the intervening 4 months, the students used an LCU (as part of their dental education), but they did not use the MARC-PS system. At that time, all but one of the students used the optional eye protection. After the 4-month interval, the energy delivered declined slightly, to 6.1 J/cm2 (Table 1), but this difference was not significant (p = 0.44, Fisher’s PLSD) and the amount of energy remained significantly greater than the baseline energy delivered (p < 0.01, Fisher’s PLSD). Furthermore, after the 4-month interval, 23 (61%) of the students delivered the minimum threshold of energy.
 Figure 2: Screen capture of the Managing Accurate Resin Curing (MARC) software showing the irradiance delivered by the students before they received additional instruction about light-curing with the MARC Patient Simulator. All students used the same SmartLite iQ2 light-curing unit for 10 seconds. The maximum amount of energy delivered to the detector under optimum laboratory conditions was 8.0 J/cm2.
Figure 2: Screen capture of the Managing Accurate Resin Curing (MARC) software showing the irradiance delivered by the students before they received additional instruction about light-curing with the MARC Patient Simulator. All students used the same SmartLite iQ2 light-curing unit for 10 seconds. The maximum amount of energy delivered to the detector under optimum laboratory conditions was 8.0 J/cm2.
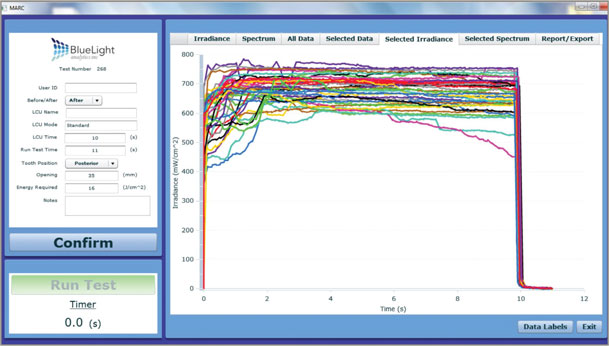 Figure 3: Screen capture of the Managing Accurate Resin Curing (MARC) software, showing the irradiance delivered by the students immediately after they received additional instruction about light-curing with the MARC Patient Simulator. All students used the same SmartLite iQ2 light-curing unit for 10 seconds. The maximum amount of energy delivered to the detector under optimum laboratory conditions was 8.0 J/cm2. After training, there was greater uniformity in irradiance delivered over the 10-second curing time.
Figure 3: Screen capture of the Managing Accurate Resin Curing (MARC) software, showing the irradiance delivered by the students immediately after they received additional instruction about light-curing with the MARC Patient Simulator. All students used the same SmartLite iQ2 light-curing unit for 10 seconds. The maximum amount of energy delivered to the detector under optimum laboratory conditions was 8.0 J/cm2. After training, there was greater uniformity in irradiance delivered over the 10-second curing time.
Table 1 Energy delivered by students before and after receiving additional light-curing instructiona 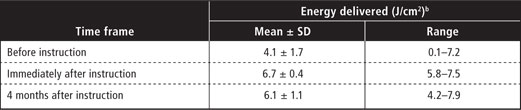
aThe same students were tested at each time point. Each student used the same light-curing unit for 10 seconds on the same tooth. The maximum amount of energy that could be delivered in 10 seconds was 8.0 J/cm2.
bAmounts of energy delivered immediately after instruction and 4 months after instruction were each significantly different from the amount of energy delivered before instruction (p < 0.01), but there was no significant difference between the amount of energy delivered immediately after instruction and the amount delivered 4 months later (p = 0.44) (Fisher’s Protected Least Significant Difference post hoc multiple-comparison tests).
Discussion
This study illustrates how easily mistakes can occur during the light-curing process and shows the importance of using proper technique to deliver the greatest amount of light from an LCU to a restoration. In this simulated clinical environment, the MARC-PS system was used to measure first-year dental students’ ability to deliver light to a simulated Class I restoration in a maxillary molar. Before the students received additional light-curing instruction, the average total energy received by the Class I preparation was 4.1 ± 1.7 J/cm2, and 84% of the students did not deliver the minimal requirement of 6 J/cm2 of energy to produce adequate curing. Therefore, the first hypothesis of this study, that students would deliver the minimum threshold of energy for curing, was rejected. However, after receiving further instruction with the MARC-PS system, 95% of the students were able to deliver the 6 J/cm2 minimum threshold set for this study.37 Therefore, the second hypothesis, that the students would deliver more energy after receiving additional instruction with the MARC-PS system, was accepted. Four months later, the students had retained the knowledge gained through this customized light-curing instruction, and improvements in energy delivery, relative to the baseline value, were both statistically significant (p < 0.01) and generally evident, with 61% of students delivering more than the minimal energy threshold. Although the students delivered less energy after 4 months (mean ± SD 6.1 ± 1.1 J/cm2) than immediately after instruction (mean ± SD 6.7 ± 0.4 J/cm2), the decline was not significant (p = 0.44). Therefore, the third hypothesis, that the students would retain their additional knowledge, was accepted.
In the first round of testing (before instruction), it was noted that the poor light-curing technique of some students adversely affected the amount of energy delivered. As a general observation, it was common for these students to point the tip of the LCU at the tooth, press the “on” button and then look away from the bright blue light. During the ensuing 10 seconds, the LCU tip would drift away from the target area of the restoration. Providing customized light-curing instruction led to improvements in the amount of energy delivered (Table 1, Figs. 2 and 3), and there was a 63% increase in the mean amount of energy delivered, from 4.1 to 6.7 J/cm2. Figure 2 illustrates the wide variation in irradiance delivered by the students before instruction. In the most extreme example, one student missed the restoration altogether during the light-curing. Figure 3 shows that the students’ technique became more consistent after instruction, with the lines becoming clustered at higher irradiance values. The mean energy that the students delivered to the simulated restoration was significantly greater immediately after and 4 months after instruction than before instruction (p < 0.01), and there was a corresponding reduction in SD values, from 1.7 J/cm2 before instruction to 0.4 J/cm2 immediately after instruction. Additionally, before receiving the instruction with the MARC-PS system, the students delivered on average only 50% of the potential maximum of 8.0 J/cm2, whereas after instruction they delivered on average 84% of the potential maximum amount of energy. This study will be repeated when the same students are in the third and fourth years of their training.
This study transfers curing light research from the laboratory environment to the clinical setting and has real-life implications. Now that the dental profession can measure how much energy is being delivered to simulated restorations, practitioners can start to manage what is likely a widespread problem of inadequate energy delivery to resin restorations. The mannequin head in the patient simulator used for this study provided a realistic simulation, and the calibrated spectroradiometric measuring device accurately quantified the effects of incorrect technique on the amount of energy delivered during light-curing. It is now possible to predict the amount of light energy that would be received, under clinical conditions, by the top surface of the resin, which is located 4 mm from the end of the light guide. It must be recognized that deeper or less accessible restorations will receive less light, whereas more accessible preparations will receive more light.
The critical minimum amount of energy required to cure a resin composite will depend on the brand and type of resin, the type of LCU and the type of light guide used.32,39-43The current study was designed to investigate if it would be possible to improve students’ ability to use an LCU; it was not designed to determine minimum exposure times. In addition, the results obtained here are specific to the brand of LCU and light guide used and may not be generalizable to other brands of equipment.32,44
Conclusions
Before receiving light-curing instruction, individual dental students exhibited a large range (between 0.1 and 7.2 J/cm2) in the amount of light energy delivered to the top surface resin positioned 4 mm from the end of an LCU light guide in a maxillary second molar. Furthermore, 84% of the students did not deliver the minimum 6 J/cm2 of energy required for adequate curing.
After the students received additional light-curing instruction with a patient simulator the mean energy delivered increased by 63%, from 4.1 ± 1.7 J/cm2 to 6.7 ± 0.4 J/cm2 (p <0.01), and 95% of the students delivered more than 6 J/cm2.
Four months later, the amount of energy that the students delivered had declined somewhat (from 6.7 ± 0.4 J/cm2 to 6.1 ±1.1 J/cm2). This reduction was not significant (p = 0.44), and the amount of energy delivered remained significantly greater than the pre-instruction value (p < 0.01). Sixty-one percent of the students delivered more than 6 J/cm2.
THE AUTHORS
References
- American Dental Association. 2005-06 Survey of Dental Services Rendered. Chicago: American Dental Association; 2007 ISBN 1-60122-027-8.
- Lohbauer U, Rahiotis C, Kramer N, Petschelt A, Eliades G. The effect of different light-curing units on fatigue behavior and degree of conversion of a resin composite. Dent Mater. 2005;21(7):608-15.
- Xu X, Sandras DA, Burgess JO. Shear bond strength with increasing light-guide distance from dentin. J Esthet Restor Dent. 2006;18(1):19-27; discussion 28.
- Kim SY, Lee IB, Cho BH, Son HH, Um CM. Curing effectiveness of a light emitting diode on dentin bonding agents. J Biomed Mater Res B Appl Biomater. 2006;77(1):164-70.
- Staudt CB, Krejci I, Mavropoulos A. Bracket bond strength dependence on light power density. J Dent. 2006;34(7):498-502. Epub 2006 Jan 18.
- Ferracane JL, Mitchem JC, Condon JR, Todd R. Wear and marginal breakdown of composites with various degrees of cure. J Dent Res. 1997;76(8):1508-16.
- Vandewalle KS, Ferracane JL, Hilton TJ, Erickson RL, Sakaguchi RL. Effect of energy density on properties and marginal integrity of posterior resin composite restorations. Dent Mater. 2004;20(1):96-106.
- Franco EB, dos Santos PA, Mondelli RF. The effect of different light-curing units on tensile strength and microhardness of a composite resin. J Appl Oral Sci. 2007;15(6):470-4.
- Segreto D, Brandt WC, Correr-Sobrinho L, Sinhoreti MA, Consani S. Influence of irradiance on the push-out bond strength of composite restorations photoactivated by LED. J Contemp Dent Pract. 2008;9(2):89-96.
- Knezevic A, Zeljezic D, Kopjar N, Tarle Z. Cytotoxicity of composite materials polymerized with LED curing units. Oper Dent. 2008;33(1):23-30.
- Uhl A, Volpel A, Sigusch BW. Influence of heat from light curing units and dental composite polymerization on cells in vitro. J Dent. 2006;34(4):298-306. Epub 2005 Sep 19.
- Brambilla E, Gagliani M, Ionescu A, Fadini L, Garcia-Godoy F. The influence of light-curing time on the bacterial colonization of resin composite surfaces. Dent Mater. 2009;25(9):1067-72. Epub 2009 Apr 17.
- Baroudi K, Silikas N, Watts DC. In vitro pulp chamber temperature rise from irradiation and exotherm of flowable composites. Int J Paediatr Dent. 2009;19(1):48-54. Epub 2008 Feb 19.
- Santini A, Watterson C, Miletic V. Temperature rise within the pulp chamber during composite resin polymerisation using three different light sources. Open Dent J. 2008;2:137-41.
- Guiraldo RD, Consani S, Lympius T, Schneider LF, Sinhoreti MA, Correr-Sobrinho L. Influence of the light curing unit and thickness of residual dentin on generation of heat during composite photoactivation. J Oral Sci. 2008;50(2):137-42.
- Durey K, Santini A, Miletic V. Pulp chamber temperature rise during curing of resin-based composites with different light-curing units. Prim Dent Care. 2008;15(1):33-8.
- Bagis B, Bagis Y, Ertas E, Ustaomer S. Comparison of the heat generation of light curing units. J Contemp Dent Pract. 2008;9(2):65-72.
- Barghi N, Berry T, Hatton C. Evaluating intensity output of curing lights in private dental offices. J Am Dent Assoc. 1994;125(7):992-6.
- Miyazaki M, Hattori T, Ichiishi Y, Kondo M, Onose H, Moore BK. Evaluation of curing units used in private dental offices. Oper Dent. 1998;23(2):50-4.
- Pilo R, Oelgiesser D, Cardash HS. A survey of output intensity and potential for depth of cure among light-curing units in clinical use. J Dent. 1999;27(3):235-41.
- Barghi N, Fischer DE, Pham T. Revisiting the intensity output of curing lights in private dental offices. Compend Contin Educ Dent. 2007;28(7):380-4; quiz 385-6.
- Hegde V, Jadhav S, Aher GB. A clinical survey of the output intensity of 200 light curing units in dental offices across Maharashtra. J Conserv Dent. 2009;12(3):105-8.
- Price RB, Felix CM, Whalen CM. Factors Affecting the Energy Delivered to Simulated Class I and Class V Preparations.J Can Dent Assoc. 2010;76:a94.
- Department of Health and Human Servcies, USA. National Institute of Dental and Craniofacial Research. National Institute of Health. Strategic Plan 2009–2013. Bethesda, MD; 2009 May. NIH Publication No. 09-7362. p. 19 Available from: http://www.nidcr.nih.gov/NR/rdonlyres/79812F51-8893-46BD-AE9D-2A125550533B/0/NIDCR_StrategicPlan_20092013.pdf
- 25.Sunnegardh-Gronberg K, van Dijken JW, Funegard U, Lindberg A, Nilsson M. Selection of dental materials and longevity of replaced restorations in Public Dental Health clinics in northern Sweden. J Dent. 2009;37(9):673-8. Epub 2009 May 4
- 26.Ferracane JL. Resin composite--state of the art. Dent Mater. 2011;27(1):29-38. Epub 2010 Nov 18.
- Opdam NJ, Bronkhorst EM, Loomans BA, Huysmans MC. 12-year survival of composite vs. amalgam restorations. J Dent Res. 2010;89(10):1063-7. Epub 2010 Jul 26.
- Leonard DL, Charlton DG, Hilton TJ. Effect of curing-tip diameter on the accuracy of dental radiometers. Oper Dent. 1999;24(1):31-7.
- Roberts HW, Vandewalle KS, Berzins DW, Charlton DG. Accuracy of LED and halogen radiometers using different light sources. J Esthet Restor Dent. 2006;18(4):214-22; discussion 223-4.
- Zhu S, Platt J. Curing efficiency of three different curing modes at different distances for four composites. Oper Dent. 2011;36(4):362-71. Epub 2011 Aug 11.
- Price RB, Labrie D, Whalen JM, Felix CM. Effect of distance on irradiance and beam homogeneity from 4 light-emitting diode curing units. J Can Dent Assoc. 2011;77:b9.
- Price RB, Dérand T, Sedarous M, Andreou P, Loney RW. Effect of distance on the power density from two light guides. J Esthet Dent. 2000;12(6):320-7.
- Yearn JA. Factors affecting cure of visible light activated composites. Int Dent J. 1985;35(3):218-25.
- Buchanan JA. Use of simulation technology in dental education. J Dent Educ. 2001;65(11):1225-31.
- Urbankova A, Engebretson SP. Computer-assisted dental simulation as a predictor of preclinical operative dentistry performance. J Dent Educ. 2011;75(9):1249-55.
- Price RB, McLeod ME, Felix CM. Quantifying light energy delivered to a class I restoration. J Can Dent Assoc. 2010;76:a23.
- Fan PL, Schumacher RM, Azzolin K, Geary R, Eichmiller FC. Curing-light intensity and depth of cure of resin-based composites tested according to international standards.J Am Dent Assoc. 2002;133(4):429-34.
- Dentsply. Smartlite IQ2 curingcard. Form #544015 ed. Milford, DE DENTSPLY International Inc.; 2005.
- Shortall AC, Harrington E. Relative merits of narrow versus standard diameter light guides. Eur J Prosthodont Restor Dent. 2001;9(1):19-23.
- Prati C, Chersoni S, Montebugnoli L, Montanari G. Effect of air, dentin and resin-based composite thickness on light intensity reduction. Am J Dent. 1999;12(5):231-4.
- Price RB, Felix CA, Andreou P. Third-generation vs a second-generation LED curing light: effect on Knoop microhardness. Compend Contin Educ Dent. 2006;27(9):490-6; quiz 497, 518.
- Price RB, Felix CA. Effect of delivering light in specific narrow bandwidths from 394 to 515nm on the micro-hardness of resin composites. Dent Mater. 2009;25(7):899-908. Epub 2009 Feb 24.
- Nomoto R. Effect of light wavelength on polymerization of light-cured resins. Dent Mater J. 1997;16(1):60-73.
- Nitta K. Effect of light guide tip diameter of LED-light curing unit on polymerization of light-cured composites. Dent Mater. 2005;21(3):217-23.



