Case Presentation
A 26-year-old woman was referred to our department with a history of occasional pain in the left cheek region and a persistent preauricular and laterocervical swelling on the left side of her face over the last 6 months (Fig. 1). At the first visit, the patient was afebril, and her vital signs were stable: heart rate, 70 beats per minute; respiratory rate, 16 per minute; arterial blood pressure, 110/70 mm Hg). Laboratory tests revealed a slightly elevated white blood cell count.
The patient had consulted various medical practitioners before considering a possible dental pathology, but her symptoms had not regressed despite repeated cycles of antibiotic therapy. Subsequently, echographic examination showed the presence of a small sialolith in the left parotid gland suggesting a diagnosis of sialolithiasis. The patient underwent 3 cycles of extracorporeal shock wave lithotripsy in the left parotid region over 1 month, with no improvement in symptoms. On the contrary, after a few weeks, the laterocervical swelling became associated with a suppurative inflammatory process of the lymph nodes located in the same area. At this point, the patient was referred to us.
A panoramic radiograph revealed dysodontiasis of the left lower third molar (tooth 38) associated with a follicular cyst (Fig. 2). An approximately 10 mm radiolucency appeared distal to tooth 38, confirming an increase from the normal size of the dental follicle. Magnetic resonance imaging (MRI) revealed a subcutaneous preauricular abscess over the left masseteric space and lymphadenopathy evidenced by enlargement of the left laterocervical lymph nodes (Fig. 3).
A decision was made to remove the left lower third molar along with the cystic lesion. Histologically, the excised specimen showed a dense infiltrate of chronic inf lammatory cells comprising predominantly lymphocytes and plasma cells (Fig. 4). The patient was given 2 g meropenem intravenously 30 minutes before the surgical procedure, and she was discharged with amoxicillin/ clavulanic acid 875 mg/125 mg to be taken orally every 12 h for 7 days. After the surgery, the patient's symptoms remitted completely. At her last visit, 6 months after the procedure, no scarring of the skin could be seen.
 Figure 1: Clinical view of the persistent preauricular abscess. A suppurativeinflammatory process of the laterocervical lymph nodes appeared after cycles of extracorporeal shock wave lithotripsy performed to resolve probable sialolithiasis.
Figure 1: Clinical view of the persistent preauricular abscess. A suppurativeinflammatory process of the laterocervical lymph nodes appeared after cycles of extracorporeal shock wave lithotripsy performed to resolve probable sialolithiasis.
 Figure 2: Panoramic radiography showed dysodontiasis of tooth 38 and the presence of a follicular cyst.
Figure 2: Panoramic radiography showed dysodontiasis of tooth 38 and the presence of a follicular cyst.
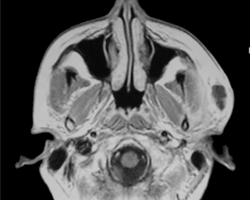 Figure 3: Magnetic resonance imaging revealed the formation of a subcutaneous abscess over the left masseteric space.
Figure 3: Magnetic resonance imaging revealed the formation of a subcutaneous abscess over the left masseteric space.
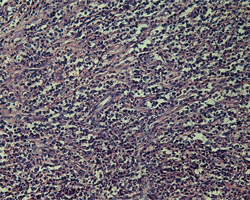 Figure 4: Histologically, the cystic lesion appeared to be a dense infiltrate of chronic inflammatory cells comprising mainly lymphocytes and plasma cells (hematoxylin and eosin staining).
Figure 4: Histologically, the cystic lesion appeared to be a dense infiltrate of chronic inflammatory cells comprising mainly lymphocytes and plasma cells (hematoxylin and eosin staining).
What is your diagnosis?
Differential Diagnosis
The clinical conditions associated with the unilateral enlargement of the preauricular region include sialolithiasis, tuberculosis, actinomycosis of the parotid gland, lymphadenitis, preauricular cyst, sebaceous cyst and neoplasm.
Sialolithiasis
Salivary gland lithiasis (sialolithiasis) is the most common disease of the major salivary glands, after mumps, and accounts for approximately 30% of all salivary disorders, with a high incidence in men aged 30 to 60.1 Sialolithiasis most commonly involves the submandibular glands (83% to 94%) and less frequently the parotid (4% to 10%) and sublingual glands (1% to 7%).2
Several hypotheses have been proposed to explain the etiology of these calculi, such as morphoanatomic factors (salivary duct stenosis, salivary duct diverticuli, etc.), saliva composition factors (high supersaturation, crystallization inhibitor deficit, etc.) and inflammatory, chemical or neurogenic factors.1 Calculi consist of a mixture of various calcium phosphates, which, once crystallized, attract and support the deposit of an organic matrix.
Surgery is highly efficacious in terms of the elimination of stones, but results in significant postoperative complications in some cases. Innovative conservative therapeutic methods include extracorporeal lithotripsy, intracannularlithotripsy and interventional sialendoscopy.3
Parotid Tuberculosis
Tuberculosis is a necrotizing granulomatous disease with varied clinical presentation and a wide distribution. Although the disease usually affects the lungs, extrapulmonary forms are not uncommon and account for approximately 20% of overall active tuberculosis.4 The salivary glands appear to be infected rarely, and involvement of the parotid gland and lymph nodes may start with a focus of mycobacterial infection in the oral cavity or a distant primary lung focus.5
This condition most commonly presents as acute sialadenitis with diffuse glandular enlargement, but it may also present as a periauricular fistula or an abscess.6
Actinomycosis of the Parotid
Primary actinomycosis is a granulomatous lesion characterized by chronic suppuration usually caused by Actinomyces israelii, gram-positive, anaerobic, commensal bacteria within the oral cavity. Actinomycosis usually occurs in healthy people, when local conditions favour its growth. It commonly affects the facial soft tissue, salivary glands, bone and skin of the face and neck. Primary actinomycosis of the parotid gland is very rare and can mimic a neoplasm.7
Clinically, cervicofacial actinomycosis is characterized by the presence of a suppurative mass with a typical discharge of pus containing tiny yellow sulphur granules, which are diagnostic. Initial symptoms including pain, fever, erythema and edema; suppuration may be absent.8
Other Conditions Causing Unilateral Enlargement of the Parotid Region
Unilateral enlargement of the parotid region can also be associated with a palpable mass or a diffuse swelling. A superficial mass in the salivary gland may suggest lymphadenitis, preauricular cyst, sebaceous cyst or extraparotid tumour. A mass inside the salivary gland may be a benign or malignant neoplasia or an intraparotid adenopathy.
The clinical symptoms of malignant tumours include rapid growth, facial nerve palsy, petrous texture and pain. The incidence of such tumours is higher among elderly patients.9
Diffuse facial swelling of the parotid region that is unrelated to the glands may be a sign of masseter muscle hypertrophy, lesions in the temporomandibular articulation or osteomyelitis affecting the ascending maxillary branch.
Rationale for Diagnosis
In the case of unilateral enlargement of the parotid region, the differential diagnosis is based on previous history of pain, paying particular attention to the location of a palpable mass or diffuse swelling. A superficial mass may be appreciated in cases of benign lymphoid hyperplasia, lymphadenitis, preauricular cyst, sebaceous cyst or extraparotid tumour, whereas a mass inside the salivary gland may suggest a neoplasm or an intraparotid adenopathy. Sialadenitis may be considered in the absence of this mass and when diffuse swelling is accompanied by episodes of salivary colic, which is characterized by an acute painful event that disappears after 15 to 20 minutes. Painful enlargements may also result from radiotherapy or may be secondary to viral sialadenitis, such as mumps.
In these cases, a simple panoramic radiograph can be used to evaluate bidimensionally any pathology in the entire dentition and surrounding bony structures, the condyles and parts of the maxillary sinus and nasal complexes. Computed tomography and MRI are frequently used when the spread of infection involves the masticatory muscles or fasciae, and they can be useful in identifying the extent of inflammation and purulent collection.
Our patient was affected by an uncommon inflammatory follicular cyst, with the potential of developing a diffuse infection. Failure of the eruptive process usually represents a risk of alteration of the dental follicle and the potential formation of a follicular cyst.
We hypothesized upward spread of the infection starting from the follicular cyst and ascending between the internal surface of the left ramus of the mandible and the internal pterygoid muscle. The infection continued this path, first climbing over the sigmoid notch, and then forming a subcutaneous abscess in the left preauricular area. The virulence of the microorganisms and masticatory forces may explain the extension of the abscess against gravity. Moreover, earlier treatment with extracorporeal shock wave lithotripsy probably promoted the spread of infection and exacerbated the suppurative process.
Third molar removal is a common surgical procedure, and the oral and maxillofacial surgeon must be familiar with all possible complications. Odontogenic infections can spread through the various spaces formed by muscles and fasciae in the maxillofacial region, causing serious complications, such as brain abscess, cavernous sinus thrombosis, temporal space infections, mediastinitis and severe deep neck space infections.10 Fortunately, in our patient, the inflammation had not spread to the parapharyngeal space, which could have created an airway obstruction and resulted in a life-threatening condition.
This paper describes a rare case of cellulitis and suppurative cervical lymphadenopathy developed from a mandibular dentigerous cyst, accompanied by an unusual subcutaneous preauricular abscess over the masseteric space. The potential for severe complications, such as sepsis or pharyngeal space involvement, along with rapid spread of infection, indicates the urgency required for correct diagnosis and immediate treatment.
THE AUTHORS
References
- Grases F, Santiago C, Simonet BM, Costa-Bauzá A. Sialolithiasis: mechanism of calculi formation and etiologic factors. Clin Chim Acta. 2003;334(1-2):131-6.
- Lustmann J, Regev E, Melamed Y. Sialolithiasis. A survey on 245 patients and a review of the literature. Int J Oral Maxillofac Surg. 1990;19(3):135-8.
- Capaccio P, Torretta S, Ottavian F, Sambataro G, Pignataro L. Modern management of obstructive salivary diseases. Acta Otorhinolaryngol Ital. 2007;27(4):161-72.
- Lee IK, Liu JW. Tuberculous parotitis: case report and literature review. Ann Otol Rhinol Laryngol. 2005;114(7):547-51.
- Hamdan AL, Hadi U, Shabb N. Tuberculous parotitis: a forgotten entity. Otolaryngol Head Neck Surg. 2002;126(5):581-2.
- Sethi A, Sareen D, Sabherwal A, Malhotra V. Primary parotid tuberculosis: varied clinical presentations. Oral Dis. 2006;12(2):213-5.
- Ermis I, Topalan M, Aydin A, Erer M. Actinomycosis of the frontal and parotid regions. Ann Plast Surg. 2001;46(1):55-8.
- Mullins JE Jr, Ogle O, Cottrell DA. Painless mass in the parotid region. J Oral Maxillofac Surg. 2000;58(3):316-9.
- Musani MA, Sohail Z, Zafar S, Malik S. Morphological pattern of parotid gland tumours. J Coll Physicians Surg Pak. 2008;18(5):274-7.
- Kinzer S, Pfeiffer J, Becker S, Ridder GJ. Severe deep neck space infections and mediastinitis of odontogenic origin: clinical relevance and implications for diagnosis and treatment. Acta Otolaryngol. 2009;129(1):62-70.



