Abstract
Root fracture injuries affect 0.5%–7% of permanent teeth. Although cervical root fractures are less frequent in children, their serious consequences and poor prognosis may lead to tooth loss. In this case presentation, we discuss a treatment approach chosen to preserve alveolar bone growth following a cervical root fracture in an 8-year-old boy.
Root fracture is rare in permanent dentition; its prevalence ranges from 0.5% to 7%.1 This type of injury damages not only the dentin, cementum and tooth pulp, but also the periodontal ligament.2 As in most traumatic dental injuries, the maxillary central incisor region is most often affected. Root fractures are uncommon in teeth with incomplete root development and those at various stages of eruption.3 Most are caused by fighting or foreign bodies striking the teeth.1 Root fractures may be horizontal, oblique or vertical; however, horizontal and oblique fractures are the most common.4
Horizontal root fractures, which constitute fewer than 3% of all dental injuries, occur most frequently in the middle third of the root, followed by apical and cervical regions.5 They are most likely to take place in fully erupted permanent maxillary central incisors with completely formed roots.6 Depending on the severity of the impact, multiple or single fractures can be observed. Single fractures distant from the cervical level are believed to be associated with a better prognosis.4
Cervical root fractures constitute 6–19% of all intra-alveolar root fractures.6 However, they have the worst prognosis due to decreased stability of the coronal fragment and loss of vitality.7 Therefore, the location of fracture becomes a very important parameter and an indicator for tooth survival following this type of injury.2 Thus, a root fracture close to the gingival margin in a child may lead to tooth loss.7 In addition to psychosocial problems, tooth loss in a growing child has unfavourable developmental and esthetic outcomes resulting from compromised bucco-palatal width of the alveolus following tooth extraction or loss. Therefore, the situation calls for an individualized treatment plan that addresses the developmental, esthetic and emotional demands of the child patient.
In this case report, we describe the treatment approach followed to preserve alveolar bone growth following a cervical root fracture in a young boy.
Case Report
An 8-year-old boy was referred to the pediatric dentistry clinic with a fractured maxillary right central incisor (tooth 11). The trauma had occurred, a week earlier, when he had collided with a friend at school. He had been seen by 2 general practitioners who advised his parents to visit a university dental clinic for treatment.
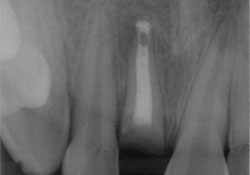
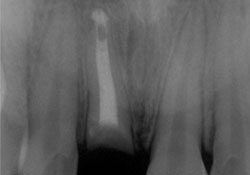
His medical history was non-contributory. Clinical examination revealed excessive mobility of the tooth, which was also tender to palpation. The neighbouring teeth were free of any symptom of trauma (Fig. 1). Following radiographic examination (Fig. 2), the injury was diagnosed as cervical root fracture.
The treatment plan comprised extraction of the coronal part of tooth 11, endodontic treatment (apexification) of the apical part followed by orthodontic extrusion and final restoration with crown reattachment.8 This plan was discussed with the patient and his parents and their approval was obtained.
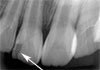
Following local anesthesia, the coronal fragment was extracted and transferred to sterile saline to be stored at 4°C for future use in a partial prosthesis.9 Inspection of the alveolar socket revealed that the fracture line was located deeply (about 4 mm) under the gingival margin (Fig. 3). It was estimated that the length of the apical part of the tooth was insufficient to satisfy the ideal crown–root ratio of 1:1 needed for crown reattachment. Thus, the treatment plan was abandoned leaving 2 available options: root submergence to facilitate alveolar bone growth or extraction of the root and fabrication of a partial prosthesis until definitive treatment could be carried out when the patient was older. These options were discussed with the parents, who decided to continue without extraction.
NOTE: Click to enlarge images.
 Figure 3: Following extraction of the coronal fragment, clinical examination revealed a deep fracture line, about 4 mm below the gingival margin.
Figure 3: Following extraction of the coronal fragment, clinical examination revealed a deep fracture line, about 4 mm below the gingival margin.
After establishing hemostasis at the extraction site, the pulp was extirpated under copious saline irrigation. The working length of the root canal was determined, and calcium hydroxide paste was placed into the root. The access cavity was covered with glass ionomer cement. The patient was prescribed antibiotics and recalled 2 weeks later.
During the second visit, under local anesthesia, a full-thickness mucoperiostal flap was reflected. The coronal part of the root surface was then further reduced to 2 mm below the marginal bone using a round bur. Utmost care was taken not to remove any bone. The root canal was thoroughly rinsed with saline to remove the calcium hydroxide paste. Subsequent irrigation with 2% chlorhexidine solution was followed by saline again. The root canal was then dried and packed with mineral trioxide aggregate (ProRoot MTA, Dentsply Maillefer, Ballaigues, Switzerland) to the predetermined working length using lentulo spirals in 3 consecutive steps. The remainder of the root canal and access cavity were obturated with high-strength glass ionomer cement. Excess cement was removed and primary wound closure was achieved by positioning the mucoperiosteal flap coronally and drawing it over the alveolus.
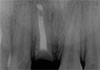
At 2 weeks after the surgery, we intended to install a temporary prosthetic appliance to prevent migration of adjacent teeth into the site. However, this plan could not be carried out as the patient had to move out of the town temporarily. On his return to the clinic, 5 months later, space closure had occurred because of migration of neighbouring teeth toward the surgery site (Fig. 4). Hence, a fan-type appliance was required to open up the space.
Following this treatment, which lasted for 6 months, it was possible to take alginate impressions of both jaws. A removable partial prosthesis was fabricated incorporating the extracted crown, which was reduced to fit on a hard plaster model. The coronal dentin was removed to approximately 1 mm from the dentino-enamel junction using a high-speed air turbine with water cooling. To copolymerize it with the pink denture resin (Dentaurum, Pforzheim, Germany), the crown was prepared with a microfilled hybrid resin composite material (Spectrum TPH, Shade B2, Dentsply, Konstanz, Germany) using an etch-and-rinse adhesive (Prime&Bond NT, Dentsply, Konstanz, Germany). Following pressurized polymerization, the prosthesis was removed from the cast. It was roughly polished and tested in the mouth, at which time occlusal adjustments were made. After fine polishing of the prosthesis, the patient was instructed on its use and maintenance.
A week later, at the first recall visit, the patient reported no complaint. He seemed comfortable and happy with his prosthesis (Fig. 5). Thereafter, the patient was followed up every 3 months. At the 33-month post-operative visit, the bucco-palatal width of alveolar bone seemed to be well preserved without significant collapse (Fig. 6). Radiographically, the submerged root showed uneventful healing (Fig. 7). However, a need for refabrication of the prosthesis was observed and scheduled for his next visit, 3 months later.
Discussion
In cervical root fractures, stabilization of the fragments with a flexible splint for up to 4 months is recommended.10 However, in the case described above, the location of the fracture line and the estimated difficulty of obtaining proper and effective stabilization of the coronal fragment led to the decision to extract the coronal segment at the outset. Although we intended to continue with orthodontic extrusion, the relatively small diameter of the extruded apical fragment was deemed to be insufficient for restoration.11 Therefore, root submergence was chosen as the treatment option.
Root submergence or “intentional root retention” is a recommended clinical procedure.10,12 Depending on clinical presentation, vital or nonvital root submergence can be attempted. Vital submergence is desirable, as it is associated with favourable outcomes, especially in terms of completion of root development and root end closure through maturogenesis.13 After more than 2 years of follow up, Rodd et al.12 reported a 91% clinical success rate among 29 nonvital and 24 vital permanent incisor roots that were intentionally retained following a crown–root fracture in children (mean age 12.1 years). In that retrospective study, of the 24 vital roots, 15 received endodontic treatment and the pulp was extirpated, 3 received pulpotomy and 5 were left untreated. The 3 teeth that were treated with pulpotomy subsequently developed pulp necrosis necessitating endodontic therapy with calcium hydroxide placement.
In a recent review, Mejàre et al.14 concluded that the current literature provides limited information about what distinguishes treatable from nontreatable pulpal inflammation in teeth with deep caries or those subjected to trauma or other injury. Johnson and Jensen13 reported a case in which a mandibular central incisor was treated with vital root submergence following a cervical root fracture in an 8-year-old patient, who had been referred to the clinic within 24 hours of the injury. In our case, because the referral time was a week after the initial traumatic injury, nonvital root submergence was chosen. The longer elapsed time increased the risk of infection in the root canal, which would have necessitated subsequent endodontic treatment if vital root submergence failed.
Our treatment approach resembles a decoronation procedure,15 the main difference being the absence of an infra-positioned (ankylosed) tooth. However, the goal of preserving the alveolar bone and allowing its continuing growth in both vertical and horizontal dimensions15 led us to choose this approach. Likewise, in the case of an ankylosed tooth, extraction has a negative effect on alveolar bone growth. Following an extraction, the surrounding alveolar process loses height and width16 resulting in narrowing and shortening of the residual ridge.17
No attempt was made to fill the canal lumen with blood18 to initiate the process that leads to gradual resorption of the remaining root and replacement of bone. Investigations of both vital and endodontically treated teeth have shown few and insignificant inflammatory changes around submerged roots.12 Furthermore, it has been reported that placement of implants in the alveolus once the patient is fully grown is relatively easy and without complications, even in cases where some remnants of the root are still visible on radiographs.15
Autotransplantation might have been an option for our patient. However, this was not considered as he had a class I occlusal relationship with slight crowding in the left maxillary anterior area (Fig. 1).
In our case, a removable partial prosthesis using the patient’s natural crown was fabricated to meet the developmental, esthetic and emotional requirements of the patient. Dependance on patient compliance, compromised esthics because of the presence of canine clasps and risk of fracture are the general disadvantages associated with the use of partial dentures. There is also the need for refabrication of the denture in parallel with growth of the jaw, as observed in this case at 2.5 years.
The long-term goal of the described treatment was to prevent the alveolar bone from ceasing to grow. Once the patient reaches maturity, the submerged root may be extracted and an implant placed to maximize the esthetic and functional outcome and provide a more predictable treatment.18 Although the treatment approach presented in this case can be regarded as temporary replacement of the missing tooth, it is an easy, functional, esthetic and relatively economical solution to the clinical problem.
THE AUTHORS
References
- Andreasen JO, Andreasen FM, Tsukiboshi M. Crown-root fractures. In: Andreasen JO, Andreasen FM, Andersson L, editors. Textbook and color atlas of traumatic ınjuries to the teeth. 4th ed. Oxford: Blackwell Munksgaard; 2007. p. 314-36.
- Welbury R, Kinirons MJ, Day P, Humphreys K, Gregg TA. Outcomes for root-fractured permanent incisors: a retrospective study.Pediatr Dent. 2002;24(2):98-102.
- Andreasen JO, Hjorting-Hansen E. Intraalveolar root fractures: radiographic and histologic study of 50 cases.J Oral Surg. 1967;25(5):414-26.
- Fayle SA. Root fractures. In: Curzon MEJ, ed. Handbook of dental trauma: A practical guide to the treatment of trauma to the teeth. 1st ed. Boston: Wright; 1999. p. 99-105.
- Calişkan MK, Pehlivan Y. Prognosis of root-fractured permanent incisors.Endod Dent Traumatol. 1996;12(3):129-36.
- Andreasen FM, Andreasen JO, Bayer T. Prognosis of root-fractured permanent incisors — prediction of healing modalities.Endod Dent Traumatol. 1989;5(1):11-22.
- Cvek M, Tsilingaridis G, Andreasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7-17 years.Dent Traumatol. 2008;24(4):379-87.
- Canoglu H, Gungor HC, Cehreli ZC. Management of cervical root fracture using orthodontic extrusion and crown reattachment: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(3):e46-9.
- Ulusoy AT, Cehreli ZC. Provisional use of a natural tooth crown following failure of replantation: a case report.Dent Traumatol. 2008;24(1):96-9.
- Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth.Dent Traumatol. 2012;28(1):2-12.
- Saito CT, Guskuma MH, Gulinelli JL, Sonoda CK, Garcia-Junior IR, Filho OM, et al. Management of a complicated crown-root fracture using adhesive fragment reattachment and orthodontic extrusion.Dent Traumatol. 2009;25(5):541-4.
- Rodd HD, Davidson LE, Livesey S, Cooke ME. Survival of intentionally retained permanent incisor roots following crown root fractures in children.Dent Traumatol. 2002;18(2):92-7.
- Johnson BR, Jensen MR. Treatment of a horizontal root fracture by vital root submergence.Endod Dent Traumatol. 1997;13(5):248-50.
- Mejàre IA, Axelsson S, Davidson T, Frisk F, Hakeberg M, Kvist T, et al. Diagnosis of the condition of the dental pulp: a systematic review.Int Endod J. 2012;45(7):597-613.
- Malmgren B. Decoronation: how, why, and when?J Calif Dent Assoc. 2000;28(11):846-54.
- Ten Heggeler JM, Slot DE, Van der Weijden GA. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: a systematic review.Clin Oral Implants Res. 2011;22(8):779-88.
- Pinho MN, Roriz VL, Novaes AB Jr., Taba M Jr., Grisi MF, de Souza SL, et al. Titanium membranes in prevention of alveolar collapse after tooth extraction.Implant Dent. 2006;15(1):53-61.
- Sigurdsson A. Decoronation as an approach to treat ankylosis in growing children.Pediatr Dent. 2009;31(2):123-8.
|
Gallery of all Figures in article |
|||
 |
 |
 |
 |
 |
 |
 |
|