Body
Periodontal Abscess
Localized, purulent infection within the tissues adjacent to the periodontal pocket that may lead to the destruction of periodontal ligament and alveolar bone
Presentation
More Likely to Occur
Periodontitis-related abscess:
- as an acute exacerbation of untreated chronic periodontitis
- as the consequence of the treatment of chronic periodontitis
Nonperiodontitis-related abscess:
- due to foreign body impaction
- due to alterations in the integrity of the root leading to bacteria colonization
Signs
- In the presence of a superficial abscess, there is an ovoid elevation of the gingiva along the lateral aspect of the root. A deep periodontal abscess might be less obvious.
- Suppuration, either spontaneous or provoked, through a fistula or from a periodontal pocket
- Tooth mobility and/or elevation
- Regional lymphadenopathy
Symptoms
- Mild discomfort to severe pain
- Sensitivity on palpation and/or percussion on the affected tooth
- Fever and/or malaise
Investigation
- Inquire about any history of chronic periodontitis and the nature of any recent dental/periodontal interventions.
- Determine the existence of a periodontal pocket (Fig. 1).
- Confirm the presence of purulent exudate.
- Obtain radiographic evidence of bone loss. However, the lack of evident bone loss does not necessarily eliminate the existence of a periodontal abscess.
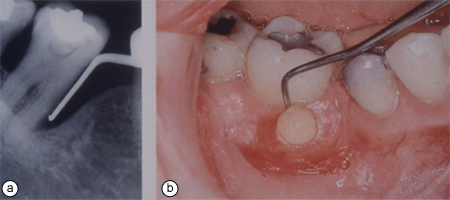 Figure 1a: Angular osseous defect on mesial aspect of tooth 47; 1b) purulent exudate on probing of deep periodontal pocket on the same tooth.
Figure 1a: Angular osseous defect on mesial aspect of tooth 47; 1b) purulent exudate on probing of deep periodontal pocket on the same tooth.
Diagnosis
Based on clinical observations/investigation, a diagnosis of periodontal abscess is determined.
Differential Diagnosis
- Periapical abscess
- Lateral periodontal cyst
- Periodontic-endodontic lesion
In case of recurrent abscesses, the following differentials should be considered:
- Osteomyelitis
- Squamous cell carcinoma
- Eosynophilic granuloma
Treatment
Two-Staged Approach
- Management of the acute lesion
Systemic antibiotics should be prescribed only when systemic involvement is evident.- Establish drainage via pocket lumen through subgingival instrumentation of the root surface. In addition, incision of the abscess may be necessary.
- If the abscessed tooth does show advanced attachment loss and its prognosis is poor, extraction should be the recommended course of action.
- Management of the original and/or residual lesion
A referral to the periodontist is usually recommended for stage-two treatment.- Therapy takes place 7 to 14 days following the management of the acute lesion, and typically includes periodontal flap surgery, particularly in the presence of deep infrabony pockets.

