Abstract
Introduction: Caries is the most common chronic disease of childhood, and severe forms may necessitate rehabilitative dental surgery. In this study, administrative data related to pediatric dental surgery performed under general anesthesia to treat severe early childhood caries in Manitoba, Canada, were reviewed to determine trends in pediatric dental surgery, as well as geographic, regional and socio-economic variations in surgical rates.
Methods: The total number of dental surgery cases performed under general anesthesia was obtained from provincial administrative databases for fiscal years from 1997–98 to 2006–07. Codes from the International Classification of Diseases and Related Health Problems (9th or 10th revision, as appropriate) were used to identify children who underwent extractions under general anesthesia for a slightly earlier fiscal year period (1996–97 to 2005–06). Each 10-year period was divided into two 5-year periods for comparisons over time. Analyses included descriptive and bivariate statistics, with the data being disaggregated by regional health authority (RHA) or by community area (for Winnipeg). Comparisons for which p ≤ 0.05 were defined as statistically significant.
Results: A total of 18,544 children had dental surgery under general anesthesia between 1997–98 and 2006–07 (mean age ± standard deviation 3.28 ± 1.02 years). Many of the children requiring surgery resided in one northern RHA (26.8%) or the Winnipeg RHA (23.8%). More than half of the RHAs (7/11) displayed significant increases in the rate of surgery, with northern RHAs having the highest rates. Within Winnipeg, 3 of the 12 community areas had significant increases in the rate of surgery. Two inner-city neighborhoods accounted for nearly 50% of surgical cases. The rate of extractions under general anesthesia increased significantly in 6 of the 11 RHAs, with northern RHAs having the highest rates. Four Winnipeg communities experienced significant increases in the extraction rate over time.
Conclusion: Pediatric dental surgery under general anesthesia for treatment of severe early childhood caries is common in Manitoba, and the demand increased in several communities over the study period. These results are being shared with decision-makers and communities to identify regions where oral health promotion is needed.
Early childhood caries (ECC) continues to be the most common chronic disease of childhood,1 with recent prevalence estimates in Canada ranging from 28% to 98%.2-5 Children with rampant forms of ECC, called severe ECC, frequently undergo rehabilitative dental surgery under general anesthesia because of the amount of treatment required and the patient's age.6,7 The American Academy of Pediatric Dentistry has established guidelines for the use of general anesthesia in pediatric dental treatment.8 Severe ECC can negatively affect childhood health and well-being, including growth, development and quality of life.9 Unfortunately, dental surgery does not always resolve the condition, as such treatment does not address underlying causative factors. Studies have suggested that more than half of children who undergo comprehensive treatment develop additional caries within 2 years.10,11
Reviewing data for pediatric dental surgery is important, as it can provide needed information on the volume and location of surgeries, the locations where affected patients reside, socio-economic distribution and regional trends. So far, few Canadian data exist to support the enhancement and redirection of existing resources to address the burden of severe ECC. Providing health care decision-makers with such information could inform resource planning and oral health promotion activities.
The purpose of this study was to review administrative data for the province of Manitoba, Canada, for all cases of pediatric dental surgery under general anesthesia and for cases involving extraction of primary teeth. The objectives were to determine trends in pediatric dental surgery, geographic and regional variations, and socio-economic differences.
Methods
This investigation used administrative data for all cases of in-hospital pediatric dental surgery under general anesthesia from fiscal year 1997–98 to fiscal year 2006–07 and cases involving the extraction of primary teeth from fiscal year 1996–97 to fiscal year 2005–06 (Note: the one year difference is because there were two separate processes for the acquisition of data and is based on availability of data). Approvals were obtained from the Health Information Privacy Committee of Manitoba Health (approval numbers 2007/2008-59 and 2006/2007-21, respectively) and the University of Manitoba's Health Research Ethics Board.
All Pediatric Dental Surgery Involving General Anesthesia
Manitoba Health covers general anesthesia fees for in-hospital dental surgery but does not cover fees for the dental surgery itself. Therefore, children eligible for inclusion in this study were identified on the basis of anesthesia tariffs for dental general anesthesia performed in hospital. Severe ECC occurs only in young children, so data were limited to preschool children less than 72 months (6 years) of age.1
Data were extracted by Manitoba Health (on the authors' behalf) from 2 separate databases: the Medical Claims/Physician Billings database and the Hospital Separation Abstracts database. Specifically, anesthesia tariffs were extracted from the Medical Claims/Physician Billings database.
The finalized database provided to the researchers from Manitoba Health included information on age, sex, postal code of patient's residence, regional health authority (RHA) of patient's residence, RHA of the health care facility where surgery was performed and the date of surgery. These data were obtained from the Hospital Separation Abstract database. It also included an indication of repeat surgery and whether the surgeon was a pediatric or general dentist. Rates of dental surgery by RHA were compared between two 5-year periods within the 10-year study period (i.e., 1997–98 to 2001–02 and 2002–03 to 2006–07). The same comparison was completed for Winnipeg community areas.
Pediatric Extractions Involving General Anesthesia
Extraction of primary teeth was chosen as a proxy for the most serious cases of severe ECC. Data were obtained from the Manitoba Centre for Health Policy repository and comprised de-identified claims data, where codes from the International Classification of Diseases and Related Health Problems (9th or 10th revision, as appropriate) were used to identify cases involving extractions. Eligibility was restricted to children less than 60 months of age, to avoid including extractions of soon-to-be-exfoliated teeth. At the time of this analysis, Manitoba had 11 RHAs, and children from all 11 RHAs (Fig. 1) were included. (In April 2012, after the analysis was completed, the 11 RHAs were reorganized and merged to create 5 HRAs.) Data were also assessed for Winnipeg's 12 community areas (Fig. 1). Rates of extraction were compared between two 5-year periods (1996–97 to 2000–01 and 2001–02 to 2005–06).
NOTE: Click to enlarge images
 Figure 1: Regional health authorities within the province of Manitoba before reorganization in 2012 and Winnipeg community areas.
Figure 1: Regional health authorities within the province of Manitoba before reorganization in 2012 and Winnipeg community areas.
Figures presenting data by RHA and community area are ordered according to socio-economic status in descending order (from highest to lowest). Income quintiles were developed for urban (Winnipeg and Brandon) and rural (all other) areas by assigning average household income from the 2001 Census to dissemination areas, then dividing the population into approximately 20% groupings by income (for more information, see the Manitoba Centre for Health Policy's Concept Dictionary definition: http://mchp-appserv.cpe.umanitoba.ca/viewDefinition.php?definitionID=102882).
Data Analysis
Rates of surgery and extraction for RHAs and Winnipeg community areas were calculated and plotted. Rates of extraction by income quintiles were also calculated. Statistical analyses included descriptive statistics (frequencies, means and standard deviations [SDs]) and bivariate analysis (t tests). Any p value ≤ 0.05 was considered significant. To maintain confidentiality, data were suppressed for rates based on values between 1 and 5.
Results
All Pediatric Dental Surgery Involving General Anesthesia
A total of 18,544 preschool children (51.8% boys) underwent pediatric dental surgery in 17 hospital facilities between 1997–98 and 2006–07. The mean age was 3.28 ± 1.02 years, and over 60% of the children were less than 4 years of age (Table 1), with 3-year-old children representing the largest group (38.1%). The numbers and rates of children undergoing dental surgery appeared to increase over time (Fig. 2).
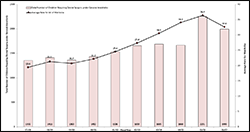 Figure 2: Provincial volume and rates of dental surgery for the province of Manitoba, Canada (1997–98 to 2006–07).
Figure 2: Provincial volume and rates of dental surgery for the province of Manitoba, Canada (1997–98 to 2006–07).
In terms of geographic distribution by patients' RHA of residence, the largest proportion of children who underwent surgery (26.8%) resided in Burntwood, an RHA located in the northern part of the province, although only 12.3% of the total surgeries were performed there. The second highest proportion of children who underwent surgery (23.8%) resided in Winnipeg, and the majority of all surgeries were performed at facilities in Winnipeg (58.8%) (Table 1).
Table 1 Age and geographic distribution of children undergoing dental surgery with general anesthetic in Manitoba (1997–98 to 2006–07)
| Variable | ||
| Age, years (months) | No. of patients | (%) of patients |
| 0–1 (< 24)* | 436 | 2.3 |
| 2 (24–35) | 3,753 | 20.2 |
| 3 (36–47) | 7,063 | 38.1 |
| 4 (48–59) | 4,685 | 25.3 |
| 5 (60–71) | 2,607 | 14.1 |
| Total | 18,544 | 100 |
| Mean ± SD | 3.28 ± 1.02 | |
| RHA of patient's residence | ||
| Assiniboine | 679 | 3.7 |
| Brandon | 406 | 2.2 |
| Burntwood | 4,967 | 26.8 |
| Central | 1,537 | 8.3 |
| Churchill | 34 | .2 |
| Interlake | 1,001 | 5.4 |
| NorMan | 1,447 | 7.8 |
| North Eastman | 998 | 5.4 |
| Parkland | 618 | 3.3 |
| South Eastman | 255 | 1.4 |
| Winnipeg | 4,411 | 23.8 |
| Out of province | 2,191 | 11.8 |
| Total | 18,544 | 100 |
| RHA of facility | ||
| Assiniboine | 86 | .5 |
| Brandon | 730 | 3.9 |
| Burntwood | 2,284 | 12.3 |
| Central | 1,174 | 6.3 |
| Churchill | 1,459 | 7.9 |
| Interlake | 0 | 0 |
| NorMan | 1,464 | 7.9 |
| North Eastman | 83 | .4 |
| Parkland | 361 | 1.9 |
| South Eastman | 0 | 0 |
| Winnipeg | 10,903 | 58.8 |
| Out of province | 0 | 0 |
| Total | 18,544 | 100 |
RHA = regional health authority, SD = standard deviation.
*Number of children < 12 months of age suppressed because of small cell size.
Rates of dental surgery by RHA of residence are shown in Figure 3a. There was a significant increase in the overall rate of dental surgery in Manitoba between the first 5-year period (1997–98 to 2001–02) and the second 5-year period (2002–03 to 2006–07) (21.6 per 1000 vs. 32.2 per 1000, p < 0.001). Statistically significant increases were observed in 7 RHAs, including Winnipeg.
Rates of dental surgery for the Winnipeg community areas are shown in Figure 3b. Two central community areas (Downtown and Point Douglas) accounted for nearly half of Winnipeg children who underwent surgery. Significant increases in the rate of surgery occurred in 3 communities (Downtown, River East and St. Vital) and for the city as a whole. Notably, the core area of Winnipeg (Downtown and Point Douglas) and Inkster experienced the highest surgery rates, and a rate reduction occurred in only one suburban community.
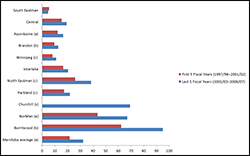 Figure 3a: Dental surgery under general anesthesia (1997–98 to 2006–07): extraction rate by Manitoba regional health authority. Dashed lines represent provincial averages (black for the earlier period, grey for the later period).
Figure 3a: Dental surgery under general anesthesia (1997–98 to 2006–07): extraction rate by Manitoba regional health authority. Dashed lines represent provincial averages (black for the earlier period, grey for the later period).
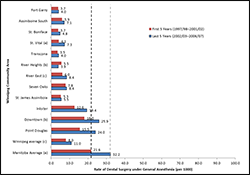 Figure 3b: Dental surgery under general anesthesia (1997–98 to 2006–07): extraction rate by Winnipeg community area. Dashed lines represent provincial averages (black for the earlier period, grey for the later period). Note: Core area of Winnipeg includes the Downtown and Point Douglas community areas. Other Winnipeg community areas are suburban.
Figure 3b: Dental surgery under general anesthesia (1997–98 to 2006–07): extraction rate by Winnipeg community area. Dashed lines represent provincial averages (black for the earlier period, grey for the later period). Note: Core area of Winnipeg includes the Downtown and Point Douglas community areas. Other Winnipeg community areas are suburban.
Of the 18,544 children included in the study sample, 231 (1.2%) were undergoing repeat surgery. The average time between procedures was 1.6 ± 0.8 years (range 0–4 years). Comparison of the number of repeat surgeries in the first and second 5-year periods showed that the number of repeat surgeries increased over time (78 for 1997–98 to 2001–02 vs. 153 for 2002–03 to 2006–07, p = 0.002). Two rural facilities (Neepawa and Boundary Trails) and the Misericordia Health Centre (Winnipeg) had the highest percentages of repeat surgeries (5.3% [1/19], 2.3% [8/343] and 2.3% [34/1495], respectively).
Pediatric Extractions Involving General Anesthesia
The provincial rate of extractions performed in hospital increased significantly across the two 5-year periods (10.2 per 1000 vs. 14.2 per 1000, p = 0.005) (Fig. 4a). Of note, all 3 northern RHAs (Churchill, NorMan and Burntwood) had significantly higher extraction rates than the provincial average for both time periods. Additionally, 6 of the 11 RHAs displayed significant increases in extraction rates across the two 5-year periods. During the second 5-year period, RHAs in Manitoba's north had the highest extraction rates. Of interest, the 2 urban RHAs (Brandon and Winnipeg) had extraction rates well below the Manitoba average. Relative to the northern region of the province, RHAs in the southern part of the province had far lower extraction rates.
Four of the 12 Winnipeg community areas had significant increases in extraction rates over time (Figure 4b). Two of these community areas (Downtown and Point Douglas) were located in central Winnipeg and displayed extraction rates well above those in the rest of the city. Only two suburban community areas (Inkster and St. Vital) experienced a significant increase in extraction rate.
In both time periods, area-level income was strongly associated with the rate of in-hospital extractions (Fig. 4c). Children living in low-income areas had significantly higher rates than those from higher-income areas. This relationship held true regardless of whether the child lived in an urban or a rural environment, with children living in rural areas having higher rates of dental extractions (p < 0.001 for both urban and rural comparisons, for both 5-year periods assessed).
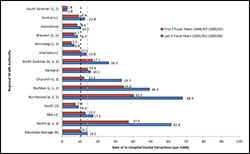 Figure 4a: In-hospital dental extractions involving general anesthesia (1996–97 to 2005–06): extraction rate by Manitoba regional health authority (RHA). The designations South, Mid and North represent geographic groupings of the RHAs. Dashed lines represent provincial averages (black for the earlier period, grey for the later period).
Figure 4a: In-hospital dental extractions involving general anesthesia (1996–97 to 2005–06): extraction rate by Manitoba regional health authority (RHA). The designations South, Mid and North represent geographic groupings of the RHAs. Dashed lines represent provincial averages (black for the earlier period, grey for the later period).
 Figure 4b: In-hospital dental extractions involving general anesthesia (1996–97 to 2005–06): extraction rate by Winnipeg community area. Dashed lines represent provincial averages (black for the earlier period, grey for the later period). Note: Core area of Winnipeg includes the Downtown and Point Douglas community areas. Other Winnipeg community areas are suburban.
Figure 4b: In-hospital dental extractions involving general anesthesia (1996–97 to 2005–06): extraction rate by Winnipeg community area. Dashed lines represent provincial averages (black for the earlier period, grey for the later period). Note: Core area of Winnipeg includes the Downtown and Point Douglas community areas. Other Winnipeg community areas are suburban.
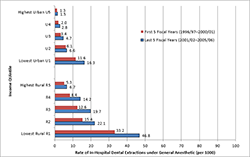 Figure 4c: In-hospital dental extractions involving general anesthesia (1996–97 to 2005–06): extraction rate by income quintile for Manitoba
Figure 4c: In-hospital dental extractions involving general anesthesia (1996–97 to 2005–06): extraction rate by income quintile for Manitoba
Discussion
The objectives of this study were to determine trends in pediatric dental surgery, geographic and regional variations, and socio-economic differences, using administrative data for surgery with general anesthesia for severe ECC in Manitoba, Canada. The intent was to provide health policy decision-makers with evidence to inform their decisions on allocation of funding and staff resources, so that oral health promotion activities can be undertaken where the needs are greatest.
In general, for the period of the study, there were significant increases in both rates of surgery and rates of extractions across Manitoba. Interestingly, 3 northern RHAs (Burntwood, NorMan and North Eastman) had significant increases in both of these rates. These results may be partially explained by the relatively high number of remote First Nations communities in northern Manitoba, where access to early dental care is scarce and prevalence of ECC is high.12,13 A recent Manitoba Health report has suggested that the rate of in-hospital dental extractions has remained high, particularly in the northern regions of the province.14.
Winnipeg also experienced an increase in the rate of surgery over the study period. One central community (Downtown) and one suburban community (St. Vital) experienced significant increases in the rates of both surgery and extractions. The increase in rate for the suburban community area was somewhat surprising but may reflect the neighbourhood's changing composition. The River East suburb experienced a significant increase only in the rate of surgery, whereas one central area (Point Douglas) and one suburban area (Inkster) experienced significant increases only in the rate of extractions. However, the trends in these latter 2 communities would also suggest increases in total surgery rates involving general anesthesia, as p values for both neighbourhoods approached the threshold for significance (p = 0.057 and 0.061, respectively).
Many children living in central Winnipeg required surgical intervention, and they represented nearly half of the total number of patients treated in Winnipeg. Other studies have shown that these 2 Winnipeg neighbourhoods have elevated caries rates.15,16 In fact, the prevalence of ECC in these areas is comparable to that on reserve and in northern communities.16 These comparative data suggest that area of residence (urban versus rural) may not always be a determinant of oral health.16 Rather, oral health may be more strongly related to socio-economic factors.
This study revealed a noticeable increase over time in the rate of children undergoing dental surgery in Manitoba, which suggests that more children are experiencing severe ECC. In addition, greater awareness of ECC through health promotion activities may have encouraged parents who would otherwise not have pursued care for their young children's tooth decay to seek out dental care. The increase in the number of children undergoing dental surgery may also reflect the increasing number of children experiencing ECC in North America as a whole.17 However, an increase in dedicated operating room time for dental surgery in Winnipeg and Thompson (to address surgical wait times) may have been a factor,6,18 even though the number of pediatric dentists remained relatively constant over this time period. Furthermore, the increase may reflect growing parental acceptance of general anesthesia in North American society. The drop in the number of children undergoing dental surgery with general anesthesia from 2005–06 to 2006–07 (as depicted in Fig. 2) is likely attributable to an increase in operating room time in 2005–06 made possible by a one-time funding arrangement with Manitoba Health to address a growing wait list.
Early childhood oral health sets the foundation for lifelong oral health, and the experience of caries at an early age is a strong predictor of future risk.19,20 About 40% of children in the current study were 3 years of age. The rates of dental surgery and extraction observed in this study indicate that early dental visits are crucial to reduce the incidence and severity of this disease. The Manitoba Dental Association implemented a Free First Visit program in 2010, which offers early screening for children under 3 years of age. This program should theoretically minimize the number of children experiencing severe ECC. However, many dentists remain unwilling to see infants and toddlers in their practices.21,22
The tendency to rely on dental surgery under general anesthesia is understandable, as this is an efficient and convenient method to minimize discomfort and diminish physical and mental stress.23 However, rehabilitative treatment does not offer a permanent solution to severe ECC, as it fails to address the underlying causative factors. In this study, 231 patients (1.2%) were undergoing repeat surgery (most within 1–2 years of the first surgery) to deal with new caries, recurrent caries or treatment failure. Numerous studies have reported much higher rates of relapse (ranging from 23% to 57%),11,24,25 and the volume of repeat surgeries in the current study is likely an underestimation. The highest percentages of repeat surgeries occurred in rural facilities (Neepawa and Boundary Trails), both of which relied on general dentists. This finding raises some concern about dental surgery under general anesthesia as performed by general dentists in rural facilities. However, it is recognized that general practitioners are doing their best in rural regions, where there are few specialists. Manitoba Health could work alongside the Manitoba Dental Association to establish acceptable standards for general practitioners in rural facilities.7
Establishing a "dental home" at a young age and visiting the dentist by 12 months of age (as recommended by the Canadian Dental Association, the Canadian Academy of Pediatric Dentistry and the American Academy of Pediatric Dentistry) may help to reduce the incidence of severe ECC.1,26 Data from a Winnipeg study revealed that children visiting a community dental clinic before 24 months of age had a significantly lower risk of ECC.15 However, despite the benefits of early identification, ECC is a complex problem that is heavily influenced by the social determinants of health. Specifically, underprivileged and lower-income communities experience higher-than-average rates of severe ECC.27 The data from this study suggest that the rate of in-hospital extractions for both urban and rural children increases as income declines. This effect was amplified for rural Manitoba, where the rate of extractions for each socio-economic quintile was much higher than the rate for its corresponding urban quintile (see Fig. 4c). It is imperative that available funding focus on delivering targeted oral health promotion and ECC prevention activities in these regions, especially for communities with documented high rates of dental surgery.
The results from this study have already been shared with the Healthy Smile Happy Child28 and Manitoba Health and should allow these organizations to direct their resources into areas with high rates of pediatric dental surgery. The Healthy Smile Happy Child project is currently collating statistics for general anesthesia in the Winnipeg region on a quarterly basis and providing this information to project stakeholders and community facilitators, with the goal of identifying areas within Winnipeg with higher rates of dental surgery. This approach will allow policy-makers and staff to focus limited resources in areas with the greatest need.
One limitation to this study involves its reliance on administrative data, which are only as reliable as the coding and entry. A lack of available data from private surgical centres may have led to underestimation of the number of rehabilitative surgeries. Although the true proportion of children undergoing dental rehabilitative surgery for caries may also have been underestimated by the exclusive use of dental extraction codes to identify cases involving extractions, the findings of this study suggest that this approach remains an acceptable proxy measure for the most serious cases of severe ECC. RHAs and health departments in other jurisdictions may want to consider using this proxy measure to gain some sense of the burden of severe ECC in their populations, for example, as a surveillance measure. However, using extractions as a proxy measure for the most severe cases may overestimate the true proportion, as some families without insurance may have opted for extractions instead of complex restorative care. Another possibility is that general dentists, who perform many of these surgeries in rural and remote communities, may be more inclined to extract primary teeth than to provide complex restorative procedures. Despite these limitations, the sample for this investigation remains robust and is representative of all children undergoing dental surgery under general anesthesia over the 10-year period examined.
Conclusions
For several Manitoba RHAs and several Winnipeg community areas, the rate of dental surgery increased over the study period. About half of the provincial RHAs experienced significant increases in extraction rates, with northern RHAs experiencing the highest extraction rates. Additionally, community areas in central Winnipeg experienced extraction rates well above those of other communities. Regional extraction rates can serve as a proxy measure for severe ECC for community health assessment purposes, especially when epidemiological data are not directly available. These findings also provide relevant information that may be used to inform decisions about funding and resource allocation, allowing for targeted early childhood oral health promotion and severe ECC prevention activities.
THE AUTHORS
References
- American Academy of Pediatric Dentistry. Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2013;35(6):50-2.
- Schroth RJ, Moffatt ME. Determinants of early childhood caries (ECC) in a rural Manitoba community: a pilot study. Pediatr Dent. 2005;27(2):114-20.
- Werneck RI, Lawrence HP, Kulkarni GV, Locker D. Early childhood caries and access to dental care among children of portuguese-speaking immigrants in the city of Toronto. J Can Dent Assoc. 2008;74(9):805.
- Schroth RJ, Cheba V. Determining the prevalence and risk factors for early childhood caries in a community dental health clinic. Pediatr Dent. 2007;29(5):387-96.
- Schroth RJ, Dahl PR, Haque M, Kliewer E. Early childhood caries among Hutterite preschool children in Manitoba, Canada. Rural Remote Health. 2010;10(4):1535.
- Schroth RJ, Morey B. Providing timely dental treatment for young children under general anesthesia in a government priority. J Can Dent Assoc. 2007;73(3):241-3.
- Schroth RJ, Smith W.F. A review of repeat general anesthesia for pediatric dental surgery in Alberta, Canada. Pediatr Dent. 2007;29(6):480-7.
- American Academy of Pediatric Dentistry. Guideline for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatr Dent. 2012;34(6):194-210.
- Schroth RJ, Harrison RL, Moffatt ME. Oral health of indigenous children and the influence of early childhood caries on childhood health and well-being. Pediatr Clin North Am. 2009;56(6):1481-99.
- Almeida AG, Roseman MM, Sheff M, Huntington N, Hughes CV. Future caries susceptibility in children with early childhood caries following treatment under general anesthesia. Pediatr Dent. 2000;22(4):302-6.
- Eidelman E, Faibis S, Peretz B. A comparison of restorations for children with early childhood caries treated under general anesthesia or conscious sedation. Pediatr Dent. 2000;22(1):33-7.
- Schroth RJ, Moore P, Brothwell DJ. Prevalence of early childhood caries in 4 Manitoba communities. J Can Dent Assoc. 2005;71(8):567.
- Schroth RJ, Smith PJ, Whalen JC, Lekic C, Moffatt ME. Prevalence of caries among preschool-aged children in a northern Manitoba community. J Can Dent Assoc. 2005;71(1):27.
- Manitoba Health. Annual Statistics 2011-2012. Winnipeg: Manitoba Health; 2013.
- Schroth RJ, Cheba V. Determining the prevalence and risk factors for early childhood caries in a community dental health clinic. Pediatr Dent. 2007;29(5):387-96.
- Schroth RJ, Moore P, Brothwell DJ. Prevalence of early childhood caries in 4 Manitoba communities. J Can Dent Assoc. 2005;71(8):567.
- Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;(248):1-92.
- News Media Services. Health Minister announces new initiatives to reduce tooth decay, lower pediatric dental wait times – $1.2 million to expand Health Smiles Program: Sale. Government of Manitoba; 2005 Nov 10 [cited 2005 Nov 10]. Available: http://www.gov.mb.ca/chc/press/top/2005/11/2005-11-10-02.html
- al Shalan TA, Erickson PR, Hardie NA. Primary incisor decay before age 4 as a risk factor for future dental caries. Pediatr Dent. 1997;19(1):37-41.
- Peretz B, Ram D, Azo E, Efrat Y. Preschool caries as an indicator of future caries: a longitudinal study. Pediatr Dent. 2003;25(2):114-8.
- Stijacic T, Schroth RJ, Lawrence HP. Are Manitoba dentists aware of the recommendation for a first visit to the dentist by age 1 year? J Can Dent Assoc. 2008;74(10):903.
- Hussein AS, Schroth RJ, Abu-Hassan MI. General dental practitioners' views on early childhood caries and timing of the first dental visit in Selangor, Malaysia. Asia Pac J Public Health. 2013 Feb 17. [Epub aheadof print].
- Anderson HK, Drummond BK, Thomson WM. Changes in aspects of children's oral-health-related quality of life following dental treatment under general anaesthesia. Int J Paediatr Dent. 2004;14(5):317-25.
- Sheehy E, Hirayama K, Tsamtsouris A. A survey of parents whose children had full-mouth rehabilitation under general anesthesia regarding subsequent preventive dental care. Pediatr Dent. 1994;16(5):362-4.
- Berkowitz RJ. Causes, treatment and prevention of early childhood caries: a microbiologic perspective. J Can Dent Assoc. 2003;69(5):304-7.
- Canadian Dental Association. CDA position on First visit to the dentist. Canadian Dental Association 2005 Feb [Reaffirmed 2012 Mar]. Available: https://www.cda-adc.ca/en/about/position_statements/.
- Ismail AI. Prevention of Early Childhood Caries. Community Dent Oral Epidemiol. 1998;26(1 Suppl):49-61.
- Macintosh AC, Schroth RJ, Edwards J, Harms L, Mellon B, Moffatt M. The impact of community workshops on improving early childhood oral health knowledge. Pediatr Dent. 2010;32(2):110-7.