Abstract
Background: Oral, lip and oropharyngeal cancer accounts for up to 75% of head and neck cancers. Dental professionals contribute to improved treatment outcomes through early detection of these cancers. Oral and maxillofacial surgeons (OMFS) are trained to participate in numerous phases of care for patients with oral, lip and oropharyngeal cancer.
Objective: To quantify the participation of Ontario OMFS in various phases of oral, lip and oropharyngeal cancer care.
Methods: A survey assessing participation of Ontario OMFS in screening, education, prevention, diagnosis, surgical oncology, reconstruction and rehabilitation of patients with oral, lip and oropharyngeal cancer was conducted in January and February 2013.
Results: Of the 210 OMFS registered with the Royal College of Dental Surgeons of Ontario, 191 were contacted, and 95 (49.7%) responded to the survey. Of the respondents, 98.9% were involved in cancer screening, 96.8% were involved in prevention and early intervention (monitoring and treatment) of premalignant lesions and 94.7% participated in diagnosis and staging. Early stage oral, lip and oropharyngeal cancer was managed surgically by 44.1% of the respondents, while 6.4% managed late-stage disease. Oral rehabilitation was managed by 77.7% of respondents.
Conclusion: OMFS are an integral part of all phases of oral and oropharyngeal cancer care including primary surgical oncology in Ontario. Dental professionals can help improve outcomes of this care through early identification of cancer using surveillance examinations at all routine dental visits. This early detection contributes directly to disease-free survival and quality of life.
Oral, lip and oropharyngeal cancer accounts for up to 75% of all head and neck cancers,1 which constitute 2% of all cancers in women and 4% in men.2 In Canada, an estimated 4000 people were diagnosed with oral cancer in 2012.3 With an incidence of 12 in 100 000, oral cancer is the 7th most common cancer in Canadian men, and the lifetime probability of developing oral cancer is 1 in 66.3,4 Outside North America, oral and pharyngeal cancer is an even greater burden: for example, incidence rates are as high as 42 in 100 000 in Southeast Asia.5 Outcomes for patients with oral and oropharyngeal cancer are largely dependent on early detection and stage of the disease at diagnosis.2,6,7Early-stage lesions requiring less surgical and radiation therapy are associated with a higher survival rate, less morbidity and better quality of life.2,6,7 The 5-year survival rate for early-stage (stages 1 and 2) oral and oropharyngeal cancer ranges from 60% to 80%, whereas that for late-stage (stages 3 and 4) cancer is 20–50%.2 The 2-year survival rate for stage 1 upper aerodigestive tract cancer (including oral, lip and oropharyngeal cancer) is approximately 90%, compared with 50% for stage 4 cancer at the same sites.6Despite the importance of early detection, only 7% of adults in the United States report having had an oral cavity examination in the past year, and only 14% at any point during their life.2,8
In Canada, dentists are the primary point of care for oral cavity examination and screening. Common dental visits, such as those for the treatment of caries, periodontal maintenance, recall visits and prosthodontic reconstruction (i.e., visits excluding specific examinations for symptoms of neoplasia or cancer) provide an opportunity to carry out oral cancer screening along with other procedures. General dental practitioners are the most likely primary care providers to identify early-stage malignancies incidentally while examining the oral and maxillofacial complex.2 This is likely because dentists routinely examine the mouth and jaws and spend more time studying oral and maxillofacial pathology during training than primary care physicians.
Cancer care is not limited to primary oncologic surgery. Education about the risk factors for cancer, prevention through risk-factor modification and appropriate screening also play important roles in minimizing the impact of these cancers. After identification of a suspicious lesion, diagnosis and staging using tissue biopsies and computed tomography imaging are important steps in characterizing the lesion and, ultimately, directing definitive management of the cancer. Consequences of radiotherapy and some surgical therapy include xerostomia, trismus, osteoradionecrosis, dysgeusia, altered speech, loss of teeth, loss of soft and hard tissue support and reduced masticatory efficiency, among others. Oral and maxillofacial surgeons (OMFS) are involved in all of these aspects of oral, lip and oropharyngeal cancer care, but are not currently included as primary oncologic surgeons in tertiary care multidisciplinary head and neck cancer teams in Ontario.
As a result, there may be a disconnect between the diagnosis and surgical management of oral and oropharyngeal cancer patients. Multiple visits to uninvolved general medical and dental practitioners and specialists (dental specialists, otolaryngologists, plastic surgeons, general surgeons) can lead to delays in definitive treatment. OMFS can provide a direct clinical and educational link between the dental community and delivery of cancer care, just as they are for other diseases, disorders and deformities of the teeth, mouth, jaws and face. Delays in time from identification of the suspected cancer to definitive treatment result in poorer patient outcomes.2,7 As the most important prognostic factor in oral and oropharyngeal cancer is the stage at diagnosis,7,9 initiating treatment as soon as possible is essential to improve outcomes. In addition, the lack of a true multidisciplinary approach may result in surgical reconstruction that does not reflect a feasible prosthodontic/oral prosthetic rehabilitation plan and contributes to reduced quality of life for the patient.
Despite their absence from multidisciplinary head and neck cancer teams, dentists and dental specialists, including OMFS, provide many phases of oral and oropharyngeal cancer care on a routine basis. Dental professionals are trained and involved in the rehabilitation of these complex patients. To quantify the participation of Ontario OMFS in oral, lip and oropharyngeal cancer care, we conducted a survey to determine such participation at various phases of care.
Methods
Survey design
Six questions were developed to evaluate the participation of OMFS in the management of oral, lip and oropharyngeal cancer. Six phases in cancer care —screening, prevention and education, early intervention, premalignant lesion management, surgical oncologic management, and post-treatment rehabilitation — were addressed in the survey's design (Table 1). Possible responses to the questions were yes or no, indicating an OMFS's involvement.
|
Yes/No |
|
Yes/No |
|
Yes/No |
|
Yes/No |
|
Yes/No |
|
Yes/No |
Survey implementation
The 2012 Royal College of Dental Surgeons of Ontario (RCDSO) source guide was used to identify all OMFS licensed to practise in Ontario; 210 were identified. Surgeons with no address listed (8) and with a practice address outside Ontario (14) were excluded from the survey. The remaining list was cross-referenced with the list of members of the Ontario Society of Oral and Maxillofacial Surgeons (OSOMS). Surgeons who were not members of OSOMS as well as those without an active email address available through OSOMS were contacted via telephone to obtain a current contact email address and verbal consent to forward the online survey to their email of preference. Five surgeons were excluded because of a lack of active email address. A total of 191 surgeons were contacted electronically by the OSOMS and OMFS department at the University of Western Ontario (Fig. 1). A reminder email was sent 1 week following the initial notification. The survey was closed 1 month following the initial contact.
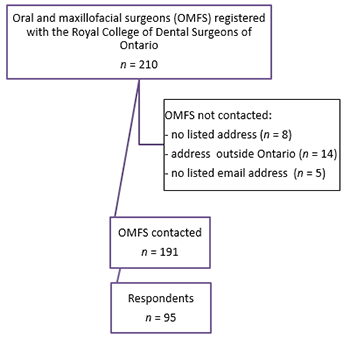 Figure 1: Selection of Ontario oral and maxillofacial surgeons for emailed survey.
Figure 1: Selection of Ontario oral and maxillofacial surgeons for emailed survey.
Results
Of the 191 OMFS contacted, 95 responded to the online survey, resulting in a 49.7% response rate.
Ontario OMFS provide all phases of oral, lip and oropharyngeal cancer care (Fig. 2), including primary oncologic surgery for malignant disease. Of the respondents, 98.9% were involved in cancer screening as assessed by question 1. In addition, 96.8% were involved in early intervention, prevention of cancer and management of pre-cancerous lesions as assessed through question 2. This included education about risks as well as the identification, monitoring and treatment of premalignant lesions. Diagnosis and staging of cancer (question 3) were performed by 94.7% of respondents. Primary surgical treatment of oral, lip and oropharyngeal cancer was divided into early-stage (stages 1 and 2, question 4) and late-stage (stages 3 and 4, question 5) disease management. Early-stage oral, lip and oropharyngeal cancer was managed by 44.1% of respondents, while 6.4% managed late-stage disease. Rehabilitation was managed by 77.7% of respondents as assessed by question 6.
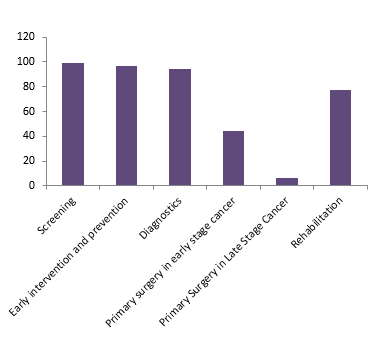 Figure 2: Involvement of Ontario oral and maxillofacial surgeons in 6 phases of oral and oropharyngeal cancer care.
Figure 2: Involvement of Ontario oral and maxillofacial surgeons in 6 phases of oral and oropharyngeal cancer care.
Discussion
Oral and maxillofacial surgeons are actively involved in the treatment and overall management of patients with head and neck cancer. Nearly all (98.9%) survey respondents indicated participation in screening. Screening tests for oral cavity cancer using adjunctive aids, such as brush biopsy, tissue fluorescence and methylene blue, are not supported by the National Comprehensive Cancer Network as publicly funded public health screening measures because of their low specificity and high sensitivity. However, despite the lack of support for universal routine oral cancer screening, thorough examination of the oral cavity should be carried out while treating or examining patients for other diseases, such as caries and periodontal disease. Prevention, early intervention and treatment of premalignant lesions was carried out by 96.8% of respondents.
The lower proportion of respondents indicating they participate in primary surgical management of early- (44.1%) versus late-stage (6.4%) oral and oropharyngeal cancer was expected. Traditionally in Canada, post-residency fellowship training in head and neck cancer surgery has been available to ear, nose and throat surgeons and plastic surgeons. With the recent increase in post-residency fellowships for OMFS in head and neck cancer, we expect to see more OMFS treating these diseases in Canada.
Contemporary management of head and neck cancer typically involves a multidisciplinary approach, including radiation oncology, medical oncology, surgical oncology, diagnostic pathology, dentistry, prosthodontics, speech pathology, physiotherapy, social work, nursing and dietary support.10,11 Surgical management of extensive lesions (stages 3 and 4) often results in large ablative defects requiring more advanced reconstructive techniques (i.e., microvascular free-tissue transfer) and cervical lymphadenectomy, as well as intensive medical support. As a result, these patients are unlikely to be cared for outside a tertiary care centre. The surgical training required to treat these cancers should include significant experience (post-residency fellowship training) in major head and neck surgery, including cervical lymphadenectomy and major maxillofacial reconstructive techniques; this is not part of the core residency training in all programs in North America.
Post-cancer rehabilitation, such as pre-prosthetic surgery, management of trismus, rehabilitation of speech, swallowing and management of masticatory deficiencies including placement of dental implants, was performed by 77.7% of respondents. Prosthodontic rehabilitation consisting of implant-supported prosthesis results in superior function and higher quality of life than non-rehabilitated mouths.12,13 The success of dental implant placement in irradiated patients treated for head and neck cancer is 90% at 3 years.14 Historically, funding has been a limitation to access by some head and neck cancer patients to dental implant and prosthodontic reconstruction. A provincial funding program is currently being developed to help these patients achieve a better quality of life through comprehensive oral rehabilitation involving dental implants and prosthodontics.
The requirements of operating time in a tertiary care centre, as well as fellowship training, likely account for the low number of OMFS treating late-stage cancer in Ontario. In the United States, 25% of residency training programs feature oncologic surgery with microvascular reconstruction as part of the core surgical curriculum.15 As a result, more North American graduating OMFS are gaining significant experience in the management of head and neck cancer patients. With this increased exposure in the United States and a similar recent increase in exposure to maxillofacial oncologic surgery in Canadian OMFS programs, it is conceivable that the number of OMFS providing definitive surgical management for oral, lip and oropharyngeal cancer will increase. The presence of OMFS on true tertiary care multidisciplinary head and neck cancer teams is required to align Ontario with industrialized countries, such as the United States, Britain, Ireland, Australia and Germany where OMFS are among the core primary oncologic surgeons working in conjunction with other allied professionals in the management of these complex patients.2,10,11 OMFS can fulfill 2 distinct roles on a tertiary care multidisciplinary team. An OMFS can act as an adjunctive surgeon providing oral rehabilitation consisting of pre-prosthetic and dental implant surgery as well as management of complications. Alternatively, or in addition to these services, an OMFS can operate as primary oncologic and reconstructive surgeon.
General practitioners (general dentists and family physicians) have the opportunity to contribute to a number of phases of oral, lip and oropharyngeal cancer care. Early detection through screening at all oral health visits combined with preventive education likely helps reduce the number of tumours presenting as late-stage disease. General dentists have been shown to detect earlier-stage oral and oropharyngeal cancer than primary care physicians.2 On detection of a suspicious lesion, biopsy and early, close follow up is recommended regardless of the age of the patient.16 The importance of thorough oral cancer screening in routine dental visits, as well as appropriate timely referral to an OMFS for diagnosis and/or treatment, cannot be underestimated.
Though a large number of OMFS claim to participate in oral rehabilitation (e.g., rehabilitation of the dentition through pre-prosthetic surgery, implants and dentures/obturators) after cancer surgery, we suspect many do not participate very often. An internal chart audit at the London Health Sciences Centre (LHSC) Dental Clinic of 100 active patients in follow up for cancer care revealed that the rate of definitive oral cavity rehabilitation was quite low (< 5%) . Other centres where OMFS are involved on regional tumour boards and where public funding is available to cover costs successfully rehabilitate up to 49% of patients with oral cancer with implant-supported prosthodontics.17,18 We suspect that LHSC's lower rate of definitive prosthodontic rehabilitation is representative of other sites in the province, and is in need of improvement.
Conclusion
OMFS are active participants in the management of oral, lip and oropharyngeal cancer in Ontario. The dental community as a whole has an important role to play in improving the outcomes of oral and oropharyngeal cancer care through early detection, prevention, screening and diagnosis. Although the vast majority of OMFS are actively involved in these phases of care, opportunities exist for an increase in the number of OMFS involved in management of patients after oncologic surgery, radiotherapy and chemotherapy. In Ontario, there is a significant need to establish multidisciplinary head and neck cancer teams featuring appropriately trained OMFS oncologists and OMFS interested in oral rehabilitation. The unique background (medicine and dentistry) of OMFS with significant experience in maxillofacial oncology and reconstructive surgery would help improve the education of future dentists and physicians about their role in management of oral, lip and oropharyngeal cancer. Inclusion of OMFS as primary members of multidisciplinary teams will likely increase the number of patients who go on to post-treatment rehabilitation, thus increasing their quality of life.
THE AUTHORS
References
- Werning JW. Oral cancer: diagnosis, management and rehabilitation. New York: Thieme Medical Publishers; 2007:1-7.
- Holmes JD, Dierks EJ, Homer LD, Potter BE. Is detection of oral and oropharyngeal squamous cancer by a dental health care provider associated with a lower stage at diagnosis? J Oral Maxillofac Surg. 2003;61(3):285-91.
- Canadian Cancer Society's Steering Committee on Cancer Statistics. Canadian cancer statistics 2012. Toronto, ON: Canadian Cancer Society; 2012.
- American Cancer Society. Cancer statistics 2013 slide presentation. Available: http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2013/index.
- Boyle P, Levin B, editors. World cancer report 2008. Geneva: WHO Press, World, Health Organization; 2008. Available: http://www.iarc.fr/en/publications/pdfs-online/wcr/2008/
- Collins R, Flynn A, Melville A, Richardson R, Eastwood A. Effective health care: management of head and neck cancers. Qual Saf Health Care. 2005;14(2):144-8.
- Dave B. Why do GDPs fail to recognise oral cancer? The argument for an oral cancer checklist. Br Dent J. 2013;214(5):223-5.
- Horowitz AM, Nourjah PA. Factors associated with having oral cancer examinations among US adults 40 years of age or older. J Public Health Dent. 1996; 56(6):331-5.
- Garzino-Demo P, Dell'Acqua A, Dalmasso P, Fasolis M, La Terra Maggiore GM, Ramieri G, et al. Clinicopathological parameters and outcome of 245 patients operated for oral squamous cell carcinoma. J Craniomaxillofac Surg. 2006;34(6):344-50.
- National Institute for Clinical Excellence (NICE). Guidance on cancer services – Improving outcomes in head and neck cancers – The manual. London: NICE; 2004.
- Scottish Intercollegiate Guidelines Network (SIGN). Diagnosis and management of head and neck cancer: a national clinical guideline. Edinburgh: SIGN, 2006.
- Teoh KH, Patel S, Hwang F, Huryn JM, Verbel D, Zlotolow IM. Prosthetic intervention in the era of microvascular reconstruction of the mandible — a retrospective analysis of functional outcome. Int J Prosthodont. 2005;18(1):42-54.
- Schoen PJ, Reintsema H, Bouma J, Roodenburg JL, Vissink A, Raghoebar GM. Quality of life related to oral function in edentulous head and neck cancer patients posttreatment. Int J Prosthodont. 2007;20(5):469-77.
- Wolff KD, Follmann M, Nast A. The diagnosis and treatment of oral cavity cancer. Dtsch Arztebl Int. 2012;109(48):829-35.
- Fattahi T, Fernandes R. Value of microvascular surgery in academic oral and maxillofacial surgery. J Oral Maxillofac Surg. 2013;71(1):189-91.
- Lydiatt D. Cancer of the oral cavity and medical malpractice. Laryngoscope. 2002; 112(5):816–9.
- Pace-Balzan A, Rogers SN. Dental rehabilitation after surgery for oral cancer. Curr Opin Otolaryngol Head Neck Surg. 2012;20(2):109-13.
- Shaw RJ, Sutton AF, Cawood JI, Howell RA, Lowe D, Brown JS, et al. Oral rehabilitation after treatment for head and neck malignancy. Head Neck. 2005;27(6):459-70.


