ABSTRACT
Dental providers must determine the presence of orofacial injury, and diagnose and treat dental and orofacial outcomes of trauma caused by motor vehicle collisions. Determination of causation and relation to the trauma is indicated. Dental trauma includes concussion, subluxation and dislocation of teeth, and fracture of teeth and maxillofacial bone, in addition to soft tissue injury that may cause ecchymosis, hematoma and laceration or abrasion. This article focuses on orofacial injury and dental complaints following motor vehicle collisions, while part 2 focuses on temporomandibular symptoms.
Introduction
Motor vehicle collisions (MVCs) may result in orofacial trauma. In addition to undergoing medical evaluation and possible treatment, victims of MVCs should be investigated for possible dental, oral and jaw-related injuries.
The history should include questions about any new symptom in the head, neck and dentition and the nature of the incident, including time, date, location and events leading to the MVC. The patient should be questioned about any direct impact (e.g., whether any portion of the head, face, jaws, mouth or teeth struck or was struck by any object), pain (severity and location) and dysfunction (e.g., difficulty opening the mouth, range of jaw movement, altered occlusion, noises in the temporomandibular joints [TMJs], difficulty speaking or chewing and mobile teeth), and numbness (of the lip or chin).
These patients should be carefully examined extraorally and intraorally.1-3 If the history or examination suggests hard tissue (maxilla or mandible) involvement, appropriate diagnostic imaging should be obtained: screening pantomographic view, plain films, dental imaging, conventional or cone beam computed tomography (CT). Suspected soft tissue injuries may require magnetic resonance imaging that includes the TMJ area.
Unless all crowns, prostheses and teeth are accounted for, radiographic examination of the periapical tissues, chest, abdominal region and perioral soft tissues should be considered to detect any missing fragments.3,4
Fractures of the mandible or maxilla are likely to be treated surgically shortly after the accident, involving open (with internal fixation) or closed reduction with or without intermaxillary fixation. In cases of condylar fractures, observation and physiotherapy might be deemed most appropriate.5-7 Lacerations in the intraoral and perioral areas are generally sutured early in the post-accident period.
Traumatic Dental Injuries
Following an MVC, a patient may be seen in a general dental practice for orofacial or dental injuries. The following are common traumatic dental injuries. The discussion below pertains to permanent teeth. There are some differences in the management of such injuries to primary teeth and the reader is advised to review other sources.8
Infraction
Infraction is cracking of the enamel without loss of tooth structure; it is best viewed using transillumination. Pulpal complications are rare (0–3.5% of cases), unless the infraction is associated with a luxation injury (see below). Pulp treatment is unnecessary unless irreversible pulpitis or pulp necrosis develops. Pulp sensitivity testing (cold test or electric pulp test) should be performed 3 and 12 months after the injury and radiography at 12 months to assess calcific metamorphosis (intrapulpal calcification).9
Fractures
Uncomplicated crown fractures may involve enamel and dentin without pulp exposure. Pulp sensitivity may be negative initially indicating transient pulpal damage. Radiographs (90° horizontal angle through the damaged tooth, occlusal view, lateral view from the mesial or distal aspect of the tooth, or cone beam (CT) may be taken to rule out displacement or fracture of the root. Radiographs of lip or cheek lacerations may also be indicated to identify tooth fragments or foreign material. Available tooth fragments can be bonded to the tooth. Exposed dentin can be covered with glass ionomer or bonding and composite resin.
Pulpal complications are rare when only enamel is fractured (0–1%) or when both enamel and dentin are involved (0–6%). However, higher rates of pulp necrosis are seen in enamel fractures with a luxation injury (8.5%) and enamel and dentin fractures with a luxation injury (up to 25%). Clinical and radiographic follow-up should be conducted at 6–8 weeks and 1 year after the injury (and perhaps yearly thereafter).9,10
Complicated crown fractures involve enamel, dentin and the pulp. Pulp sensitivity testing is usually not indicated initially, but should be performed at follow-up visits. Radiographic examination should be conducted as described above. In young patients, it is advantageous to preserve pulp vitality by pulp capping or partial pulpotomy using either calcium hydroxide or (white) mineral trioxide aggregate.11,12 In adult patients, endodontic treatment is the treatment of choice, although pulp capping or partial pulpotomy may also be selected. If the pulp becomes necrotic, endodontic treatment is indicated to preserve the tooth. In complicated crown fractures without an associated luxation injury, pulp necrosis does not usually occur immediately, although this is inevitable if exposed pulp remains untreated for 1 month (except for immature teeth). These teeth should be followed clinically and radiographically at 6–8 weeks and 1 year.9,10
Crown-root fractures may be associated with pulp exposure, and pulp sensitivity testing is usually positive. Radiographs from more than one angle or cone beam CT may be necessary to detect root fracture. Treatment recommendations are the same as for complicated crown fractures. Stabilizing loose segments of the tooth by bonding may be advantageous until a definitive treatment plan can be formulated. However, other options may need to be considered depending on the fracture specifics. The clinical and radiographic follow-up schedule is the same as for crown fractures.9,10
With root fracture, the coronal segment may be mobile and displaced. The tooth may be tender to percussion. Pulp sensitivity testing may yield negative results initially, indicating transient or permanent pulpal damage; therefore, monitoring is recommended. Transient crown discolouration (red or gray) may occur. Root fractures in the horizontal plane can usually be detected in a regular 90° radiographic image with the central beam through the tooth, and this is usually the case with fractures in the cervical third of the root. If the plane of fracture is more diagonal, which is common in apical or middle third fractures, an occlusal view or cone beam CT image is more likely to show the fracture.13
If the coronal segment of the tooth is displaced, it should be repositioned as soon as possible and its position assessed radiographically. The tooth should be stabilized with a flexible splint for 4 weeks. If the root fracture is near the cervical area of the tooth, stabilization is beneficial for a longer period (up to 4 months). It is advisable to monitor healing for at least 1 year.
If pulp necrosis develops, endodontic treatment of the coronal tooth segment to the fracture line is indicated. Clinical and radiographic follow-up should take place at 4 weeks, 6–8 weeks, 4 and 6 months, 1 year and 5 years.10 If necrosis develops (20–44% of cases), it is generally detectable after 2–5 months. If the fracture line is communicating with the oral cavity, the coronal fragment is removed, whereas if the fracture does not communicate with the gingiva and is not mobile or displaced, treatment may not be necessary, although follow-up is needed. If pulp necrosis and infection develop, the pulp is removed from the fracture site and apexification procedures involving the use of calcium hydroxide, mineral trioxide aggregate or both are suggested.9
Alveolar bone fractures may also extend to adjacent bone resulting in segment mobility and dislocation. An occlusal change due to misalignment of the fractured alveolar segment may be noted. Pulp sensitivity may or may not be positive. Fracture lines, which may be located at any level from the marginal bone to the root apex, can be detected in appropriate radiographs. Treatment involves repositioning and splinting of the displaced segment for 4 weeks. The clinical and radiographic follow-up schedule is the same as for root fracture cases.10
Concussion
Concussion is an injury to the tooth-supporting structures without abnormal loosening or displacement of the tooth, displaying a marked reaction to percussion (in a horizontal or vertical direction). There may be no bleeding from the gingiva. Pulp sensitivity tests are likely to be positive and no abnormalities are seen radiographically.
No treatment is needed for these teeth, except for possible selective occlusal adjustment of the opposing teeth and follow-up. However, the pulpal condition should be monitored for at least 1 year (including at 4 weeks and 6–8 weeks). If clinical findings, including pulp sensitivity tests and radiographic examination, show no abnormalities, monitoring may be terminated at that time.
Following a concussion injury, pulpal necrosis of open apex teeth is rare and fewer than 5% of teeth with a closed apex undergo pulpal necrosis within 1 year. External root resorption occurs in approximately 4% of concussed teeth.8,10,14-16 Pulp canal obliteration is an infrequent complication (2–7% of cases).9
Subluxation
Subluxation is an injury to the tooth-supporting structures with loosening, but not displacement of the tooth, and can cause sensitivity to percussion and occlusal forces. Bleeding from the gingival crevice may be noted. Pulp sensitivity may be negative initially, indicating transient pulpal damage; however, these teeth usually respond positively to sensitivity tests. Radiographic abnormalities are usually not found, although a slight widening of the periodontal ligament space may be seen in cases with marked mobility.
Treatment may include selective occlusal adjustment of the opposing teeth and a flexible splint (for up to 2 weeks) in the case of multiple tooth injuries. The pulpal condition of teeth that have undergone subluxation should be monitored for at least 1 year (including at 4 weeks and 6–8 weeks and perhaps up to 5 years), as pulpal necrosis occurs in approximately 15% of closed apex cases (generally within 1 year) and rarely in teeth with an open apex. Root resorption is rare: 2% incidence for subluxated teeth and 0.5% incidence of inflammatory root resorption.8,10,14-16 Canal calcification occurs in 9–12% of teeth.9
Luxation
Extrusive luxation occurs when a tooth is extruded apically from its socket with minimal damage to the socket wall. The tooth appears elongated and is mobile. Pulp sensitivity will likely be negative. Pulp revascularization may occur in mature teeth; it often occurs in teeth with open apices. Radiographs show an increased periodontal ligament space apically.
The tooth should be gently repositioned in the socket and stabilized for 2 weeks with a flexible splint. Follow-up radiography and pulp sensitivity testing should be done at 2 weeks; 1, 2, 6 and 12 months; and yearly for at least 5 years. Pulp necrosis has been reported in 43% of teeth (usually within 1 year), pulp calcification in 35% and progressive root resorption in 5.5%. Endodontic treatment should begin immediately (particularly in immature teeth) if evidence of pulp necrosis with infection or root resorption is observed.9,10
A tooth exhibiting lateral luxation is displaced, usually in a palatal–lingual or labial direction, and is accompanied by fracture or comminution of the socket wall. The tooth will be immobile and percussion generally produces a high, metallic (ankylotic) sound. Pulp sensitivity tests will likely produce negative results. Pulpal revascularization usually occurs in immature teeth. The periodontal ligament space is widened and best visualized on eccentric or occlusal exposures or cone beam CT imaging.
The tooth should be gently repositioned in its original location as soon as possible to disengage it from its bony lock and stabilized for 4 weeks using a flexible splint. Pulp necrosis (40% in children and 58% in adults), pulp canal calcification (40%) and root resorption (26%) are common sequelae. Clinical and radiographic follow-up should occur at 2 weeks, 6–8 weeks, 6 months, 1 year and then yearly for 5 years. If the pulp becomes necrotic, endodontic treatment is indicated to prevent root resorption.9,10
Intrusive luxation is likely to result in pulpal necrosis and root resorption, depending on the extent of intrusion. Intruded teeth are not mobile; percussion may produce a high, metallic sound and pulp sensitivity tests are likely to be negative. On radiographs, the periodontal ligament space may be absent from all or part of the root. For teeth with complete root formation, the tooth should be repositioned either orthodontically or surgically as soon as possible. In immature teeth, pulpal revascularization may occur. For teeth with incomplete root formation, spontaneous repositioning should be allowed to take place. However, if no movement is noted in 3 weeks, rapid orthodontic repositioning or surgical repositioning might be necessary in some cases. The pulp will likely be necrotic and endodontic treatment using a temporary filling with calcium hydroxide is recommended to retain the tooth. Splinting for 4 weeks has been suggested for some cases. Pulp necrosis is usually diagnosed within 6 months, but may develop years later in open-apex teeth.9,10 Progressive root resorption occurs in nearly 50% of cases. Teeth should be followed clinically and radiographically at 2 weeks, 6–8 weeks, 6 months, 1 year and then yearly for 5 years. Almost all surviving intruded immature teeth undergo pulpal calcification. An adverse outcome is common following intrusive luxation.
Avulsion
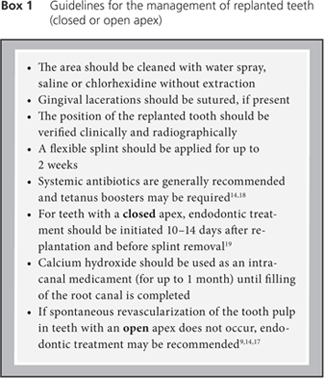
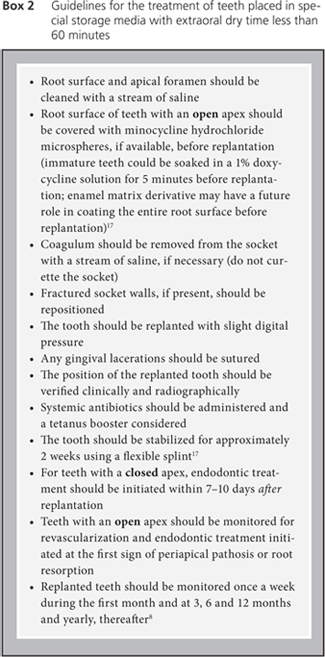
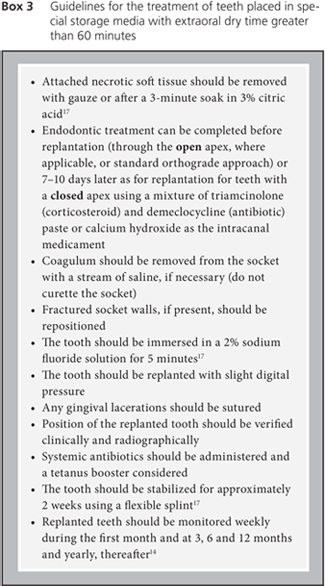
Avulsion is a broad topic and beyond the scope of this article. Excellent reviews have been published elsewhere.9,14,17 However, several factors can influence the approach to avulsed teeth, including whether the tooth has a closed or open (1 mm or more) apex, whether it has been replanted, whether it has been kept in special storage media and whether the extraoral dry time is less than or longer than 60 minutes, as the critical limit for dry time is reported to be no more than 20 minutes.17 Guidelines for the management of avulsed teeth are presented in Boxes 1–3.
| Click on the boxes to view larger versions. | ||||
|---|---|---|---|---|
 |
 |
 |
||
Resorption
Inflammatory root resorption is the primary cause of loss of replanted teeth (as many as 68% develop resorption). The revascularization rate of replanted teeth has been reported to range from 8% in mature teeth to 25–34% in immature teeth. Success rates of 24–57% have been reported relative to periodontal ligament healing. When it has been confirmed that a replanted tooth is undergoing osseous replacement resorption (ankylosis), decoronation should be considered along with options for permanent restoration. Ankylosis may occur in approximately half of replanted avulsed teeth and inflammatory root resorption in a quarter of replanted teeth.17
Pain Referred to the Dentition
Pain arising in the muscles of mastication may be referred to the dentition, most often to posterior teeth, and this must be considered before dental intervention. Pain reported in the teeth can also be referred from maxillary sinuses, as well as nasal mucosa, cardiac, migrainous/vascular, neuropathic and psychogenic causes/sources.20
Neurologic Symptoms
Patients may have complaints of numbness extraorally or intraorally due to a direct blow to the area causing soft tissue injury, fracture or injury to the trigeminal nerve. Furthermore, chronic neuropathic pain in the head and neck regions with an orofacial distribution can occur. Facial paralysis involving the VIIth cranial nerve may result from temporal bone fracture.21
Temporomandibular Disorders
Head and neck pain and temporomandibular disorders following an MVC could be referred to dental practitioners. These injuries are discussed in part 2 of this article.
THE AUTHORS
References
- Ceallaigh PO, Ekanaykaee K, Beirne CJ, Patton DW. Diagnosis and management of common maxillofacial injuries in the emergency department. Part 5: Dentoalveolar injuries. Emerg Med J. 2007;24(6):429-30.
- Lynham AJ, Hirst JP, Cosson JA, Chapman PJ, McEniery P. Emergency department management of maxillofacial trauma. Emerg Med Australas. 2004;16(1):7-12.
- Elias H, Baur DA. Management of trauma to supporting dental structures. Dent Clin North Am. 2009;53(4):675-89.
- Subramanian K, Chogle SM. Medical and orofacial considerations in traumatic dental injuries. Dent Clin North Am. 2009;53(4):617-26.
- Andreasen JO, Storgard Jensen S, Kofod T, Schwartz O, Hillerup S. Open or closed repositioning of mandibular fractures: is there a difference in healing outcome? A systematic review. Dent Traumatol. 2008;24(1):17-21.
- Nussbaum ML, Laskin DM, Best AM. Closed versus open reduction of mandibular condylar fractures in adults: a meta-analysis. J Oral Maxillofac Surg. 2008;66(6):1087-92.
- Stacey DH, Doyle JF, Mount DL, Snyder MC, Gutowski KA. Management of mandible fractures. Plast Reconstr Surg. 2006;117(3):48e-60e.
- Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F, et al. Guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth. Dent Traumatol. 2007;23(3):130-6.
- Moule AJ, Moule CA. Minor traumatic injuries to the permanent dentition. Dent Clin North Am. 2009;53(4):639-59.
- Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F, et al. Guidelines for the management of traumatic dental injuries. I. Fractures and luxations of permanent teeth. Dent Traumatol. 2007;23(2):66-71.
- Accorinte ML, Loguercio AD, Reis A, Carneiro E, Grande RH, Murata SS, et al. Response of human dental pulp capped with MTA and calcium hydroxide powder. Oper Dent. 2008;33(5):488-95.
- Dammaschke T, Wolff P, Sagheri D, Stratmann U, Schafer E. Mineral trioxide aggregate for direct pulp capping: a histologic comparison with calcium hydroxide in rat molars. Quintessence Int. 2010;41(2):e20-30.
- Bornstein MM, Wolner-Hanssen AB, Sendi P, von Arx T. Comparison of intraoral radiography and limited cone beam computed tomography for the assessment of root-fractured permanent teeth. Dent Traumatol. 2009;25(6):571-7. Epub 2009 Oct 14.
- Flores MT, Malmgren B, Andersson L, Andreasen JO, Bakland LK, Barnett F, et al. Guidelines for the management of traumatic dental injuries. III. Primary teeth. Dent Traumatol. 2007;23(4):196-202.
- Andreasen FM, Pedersen BV. Prognosis of luxated permanent teeth—the development of pulp necrosis. Endod Dent Traumatol. 1985;1(6):207-20.
- Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. Hoboken (NJ): Blackwell Munksgaard; 2007.
- McIntyre JD, Lee JY, Trope M, Vann WF Jr. Permanent tooth replantation following avulsion: using a decision tree to achieve the best outcome. Pediatr Dent. 2009;31(2):137-44.
- Hinckfuss SE, Messer LB. An evidence-based assessment of the clinical guidelines for replanted avulsed teeth. Part II: prescription of systemic antibiotics. Dent Traumatol. 2009;25(2):158-64.
- Hinckfuss SE, Messer LB. An evidence-based assessment of the clinical guidelines for replanted avulsed teeth. Part I: Timing of pulp extirpation. Dent Traumatol. 2009;25(1):32-42.
- Okeson JP, Falace DA. Nonodontogenic toothache. Dent Clin North Am. 1997;41(2):367-83.
- Hung T, Thomas R. Facial paralysis after a road traffic accident. J R Soc Med. 1998;91(6):322-3.
