A swollen lip is common in clinical practice, but the differential diagnosis and management of the condition may be challenging. Lip swelling may be related to a local or systemic condition, and it can be the earliest manifestation of a systemic disease. The differential diagnosis can be simplified by grouping findings into broad categories: trauma, inflammation, infection, metabolic diseases, neoplasm and idiopathic conditions (Box 1). In this article, we present a clinical case to illustrate the diagnostic approach and associated recommendations for care.
Box 1 Differential diagnosis of lip swelling
| Category | Diseases |
| Trauma |
|
| Immunodysregulation or inflammation |
|
| Infection |
|
| Metabolic disease |
|
| Neoplasm |
|
| Idiopathic condition |
|
Case Report
A 21-year-old man presented with a 4-month history of lower lip swelling that began without a clearly identifiable precipitating event. The inner aspects of his cheeks also felt swollen and sore. A system review revealed a recent history of occasional dark bloody stool that prompted priority medical assessment, including colonoscopy. The results of these tests were nondiagnostic, but symptoms resolved satisfactorily and no additional investigations were recommended.
The patient was otherwise well. He was taking no prescription medications and had no known drug allergies. Examination revealed no facial asymmetry. Cranial nerve function was normal. Facial skin was intact and without erythema. His lower lip was diffusely swollen, soft and not tender to palpation (Fig. 1a). No fissuring or irregularity in the contour of the lip mucosa was noted. There was no cervical lymphadenopathy. Intraorally, the oral mucosa was moist. Fissuring and ulceration were noted on the posterior buccal mucosa and retromolar areas bilaterally (Figs. 1b and 1c). The dentition was intact and oral hygiene was satisfactory. There were no palpable masses.
 |
 |
 |
|
Figure 1: Clinical images showing (a) diffuse swelling of the lower lip with intact vermillion and overlying mucosa, and fissuring and ulceration of the (b) left and (c) right posterior buccal mucosa. |
||
Differential Diagnosis
More than 180 conditions may present with lip swelling1 and the pertinent diagnostic features do not always appear simultaneously. In addition to use of a standardized approach to the evaluation of an oral mucosal lesion,2 6 main questions can be used to categorize most conditions or diseases associated with lip swelling (Fig. 2):
- Was the onset acute or is this a recurring or persistent condition?
- Is the lip swelling localized or diffuse?
- Is there any history of trauma to the area?
- Is there any relevant medical history?
- Are there any systemic signs or symptoms?
- Are there any perioral or oral signs or symptoms?
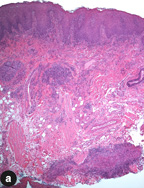
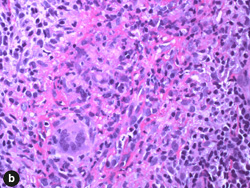
This man presented with diffuse lip swelling of acute onset. The swelling was progressive with intraoral fissuring and ulceration. No significant medical findings were initially identified and there was no history of trauma to the area. This narrowed the diagnostic possibilities to orofacial granulomatosis, Crohn disease, sarcoidosis and cutaneous T-cell lymphoma. A biopsy was performed to render a definitive diagnosis. Histopathology showed noncaseating granulomatous inflammation (Fig. 3). Special stains for fungal microorganisms and mycobacterium were negative. No foreign body was identified. The diseases associated with noncaseating granulomatous inflammation are described in Box 2.
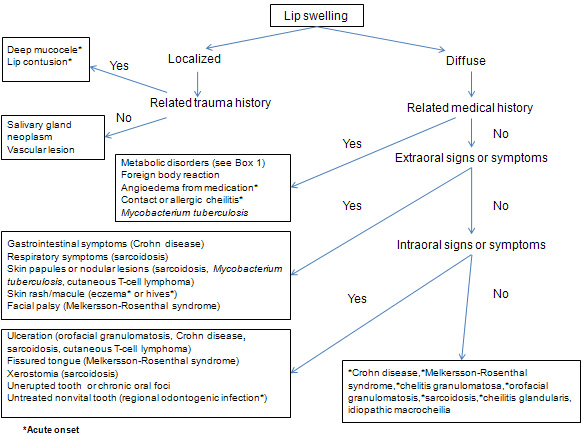 Figure 2: Flowchart showing pertinent questions and differential diagnosis of lip swelling.
Figure 2: Flowchart showing pertinent questions and differential diagnosis of lip swelling.
 |
 |
|
Figure 3: Photomicrographs of the lip biopsy specimen showing (a) densely packed clusters of lymphohistiocytic infiltrates in the submucosa and (b) noncaseating granuloma with multinucleated giant cells. Hematoxylin and eosin staining; original magnification: a, 40× and b, 400×. |
|
Box 2 Diseases involving lips with noncaseating granulomatous inflammation
| Disease | Clinical features |
| Crohn disease | Chronic granulomatous inflammation can involve the entire gastrointestinal tract. Lip swelling is sometimes the earliest symptom, followed by gastrointestinal tract manifestations (abdominal cramping and pain, nausea, diarrhea, weight loss and malnutrition). Associated intraoral lesions can present as linear ulcerations with a cobblestone appearance involving the buccal vestibule and mucogingival fold, aphthous-like ulcerations or small suppurative ulcers such as pyostomatitis vegetans. This disease can sometimes involve skin, eyes and joints. |
| Sarcoidosis | A multisystem granulomatous disorder, the common manifestations include dyspnea, dry cough, chest pain, fever, malaise, fatigue, arthralgia and weight loss. Perioral and intraoral signs can include lip swelling or a submucosal mass, an isolated papule or ulceration. Can sometimes mimic Sjogren syndrome with dry mouth or present with ill-defined radiolucencies in the jaw without bony expansion. Extraoral manifestations may include bilateral hilar lymphadenopathy, which can be identified on chest radiographs, lupus pernio on the face and erythema nodosum on the lower legs. |
| Orofacial granulomatosis | This disease requires a diagnosis of exclusion. It presents with lip swelling as the initial symptom, followed by linear ulceration in the buccal vestibule, erythematous swelling of the gingiva, a cobblestone appearance of the buccal mucosa and hyperplastic papules on the palate. |
As a result of the findings noted above, the patient was referred to a gastroenterologist for assessment for possible sarcoidosis or Crohn disease. This consultation took place approximately 10 months after the initial investigations. The patient's chest radiograph was normal. Repeat colonoscopy with biopsy was performed, and this time histopathology revealed focal moderate active ileitis and marked ulceration of the ileocecal valve, consistent with Crohn disease.
Management
Granulomatous cheilitis has been recognized as an early manifestation of Crohn disease,3 and orofacial granulomatosa has been reported as the initial manifestation.4 Therefore, a patient with undiagnosed Crohn disease may present for dental assessment.
Crohn disease is a systemic condition typically requiring medical management.5 If a patient is receiving systemic therapy, such as oral steroids, azathioprine, thalidomide or infliximab, local treatment of lip swelling may or may not be indicated. Close collaboration with the treating physician is, therefore, required.
For dentists, contributions to management of isolated intraoral or perioral manifestations of Crohn disease may include topical or intralesional corticosteroids, with intralesional therapy typically preferred.
Conclusion
Lip swelling can sometimes be a sign of systemic disease. A step-by-step evaluative approach to diagnosis is recommended. Local treatment may be indicated, with consideration of prompt medical referral if systemic signs or symptoms are present. A collaborative approach is critical in optimizing care.
THE AUTHORS
References
- Collins RD. Lip swelling. In: Differential diagnosis in primary care. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 297.
- Williams PM, Poh CF, Hovan AJ, Ng S, Rosin MP. Evaluation of a suspicious oral mucosal lesion. J Can Dent Assoc. 2008;74(3):275-80. Available: www.cda-adc.ca/jcda/vol-74/issue-3/275.html.
- Triantafillidis JK, Valvi FZ, Merikas E, Peros G, Galitis ON, Gikas A. Granulomatous cheilitis associated with exacerbations of Crohn's disease: a case report. J Med Case Reports. 2008;2:60.
- Al Johani K, Moles DR, Hodgson T, Porter SR, Fedele S. Onset and progression of clinical manifestations of orofacial granulomatosis. Oral Dis. 2009;15(3):214-9. Epub 2008 Feb 16.
- Fatahzadeh M, Schwartz RA, Kapila R, Rochford C. Orofacial Crohn's disease: an oral enigma. Acta Dermatovenerol Croat. 2009;17(4):289-300.
