An 8-year-old girl attended the authors' clinic for investigation of a stable, asymptomatic lesion on the dorsum of the tongue, which had developed over the previous 6 months. The patient admitted to biting the lesion occasionally. Her medical history was of no relevance. Oral exploration showed an exophytic tumoural lesion 4 mm in diameter located on the right side of the tongue dorsum, whitish in colour and nondeformable to pressure, of fibrous consistency and with no appreciable depth (Fig. 1). The clinical impression was of a pyogenic granuloma. Excision was performed, and a sample of tissue was sent for histopathologic examination.
Differential diagnostic considerations for the lesion included pyogenic granuloma, benign fibrous histiocytoma, atypical or juvenile xanthogranuloma, nevomelanocytic lesion and irritative keratosis.
Histologically, the lesion was characterized by a submucosal, cellular aggregation of spindle-shaped, fibroblast-like cells with relatively pale, oval nuclei. Scattered, round histiocytic cells were also present (Fig. 2a).
The diagnosis was confirmed using immunostaining for vimentin (positive), CD68 marker (positive), CD34 marker (positive), Ki-67 protein (positive), protein S-100 (negative), CD117 marker (negative), Leu7 marker (negative), desmin (negative) and α-smooth muscle actin (negative) (Fig. 2b). In the 3 years since the intervention, there has been no recurrence.
 Figure 1: Clinical image of the dorsum of the tongue of an 8-year-old patient. The exophytic lesion has a whitish appearance and is well delimited.
Figure 1: Clinical image of the dorsum of the tongue of an 8-year-old patient. The exophytic lesion has a whitish appearance and is well delimited.
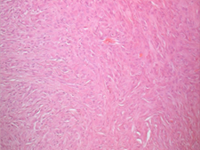 Figure 2a: Histologic sample stained with hematoxylin and eosin. The distribution of lesional cells appears homogeneous, and these cells did not extend into the deeper connective tissues. The lesional cells displayed both epithelioid and spindle-shaped morphology. The spindle-shaped cells occurred in a storiform pattern.
Figure 2a: Histologic sample stained with hematoxylin and eosin. The distribution of lesional cells appears homogeneous, and these cells did not extend into the deeper connective tissues. The lesional cells displayed both epithelioid and spindle-shaped morphology. The spindle-shaped cells occurred in a storiform pattern.
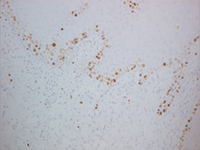 Figure 2b: Sample of the lesion after immunohistochemical staining with antibodies to Ki-67 protein, a cellular marker for proliferation. There is a lack of staining in the connective tissue, but staining has occurred in the basal layer of the epithelium. Ki-67–positive cells are rare in this type of tumour.
Figure 2b: Sample of the lesion after immunohistochemical staining with antibodies to Ki-67 protein, a cellular marker for proliferation. There is a lack of staining in the connective tissue, but staining has occurred in the basal layer of the epithelium. Ki-67–positive cells are rare in this type of tumour.
What is the provisional diagnosis?
Discussion
Benign fibrous histiocytoma (BFH) is a mesenchymal tumour that has been described as a benign neoplasm composed of fibroblasts and histiocytes, occurring in the cutaneous and noncutaneous soft tissues.1-3 Intraoral presentation is rare.
The clinical diagnosis of oral BFH should be based on the clinical features, specifically a slowly enlarging, well-circumscribed lesion, with no aggressive behaviour in relation to the overlying intact mucosa. However, BFH cannot be differentiated on a clinical basis from other soft-tissue neoplasms. Histological examination reveals mitosis (rarely), absence of cellular atypia and characteristic immunochemistry patterns.
The diagnosis of BFH is controversial because of its uncertain histogenesis.4,5 Histologically, the cells in some cases resemble myofibroblasts, primitive mesenchymal cells or cells having intermediate or mixed features. Other histological features frequently described for BFH are the presence of multinucleated giant cells, abundant vascularity and inflammatory infiltrate. The main differential diagnosis of oral BFH includes nodular fasciitis, solitary fibrous tumour, neurofibroma and dermatofibroma.
Because of the lack of specific markers for fibrohistiocytic lesions, the diagnosis of BFH is generally based on the absence of markers for cells of other lineages. Immunohistochemically, BFH is characterized by a strong and diffuse positivity for vimentin, moderate positivity for factor XIIIa and negativity for protein S-100. However, like the case reported here, some previously published cases have reported BFH lesions that do not stain for factor XIIIa. The treatment of choice is complete resection of the tumour, which results in an excellent prognosis and a recurrence rate of almost zero. Fewer than 5% of cutaneous fibrous histiocytomas recur following local excision, and most reported cases of oral BFH have featured no recurrence. BFH has no metastatic potential, and neither radiotherapy nor chemotherapy currently plays a role in its management.
THE AUTHORS
References
- Femiano F, Scully C, Laino G, Battista G. Benign fibrous histiocytoma (BFH) of the cheek: CD68-KP1 positivity. Oral Oncol. 2001;37(8):673-5. Review.
- Alves SA, Vargas PA, Coelho Siqueira SA, Coletta RD, de Almeida OP. Benign fibrous histiocytoma of the buccal mucosa: case report with immunohistochemical features. J Oral Maxillofac Surg. 2003;61(2):269-71
- Silverman JS, Glusac EJ. Epithelioid cell histiocytoma--histogenetic and kinetics analysis of dermal microvascular unit dendritic cell subpopulations. J Cutan Pathol. 2003;30(7):415-22.
- Rawal YB, Kalmar JR, Shumway B, Mallery SR. Presentation of an epithelioid cell histiocytoma on the ventral tongue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100(1):75-83.
- Ertas U, Büyükkurt MC, Cicek Y. Benign fibrous histiocytoma: report of case. J Contemp Dent Pract. 2003;4(2):74-9.
