The HIV-infected population is increasing, and many of these patients are presenting atypical features. It is imperative that dentists be aware of these features to permit diagnosis and early treatment. We describe the case of an adult male with parotid swelling as the initial manifestation of HIV infection. This article emphasizes the need for suspicion of HIV infection when a patient reports with a cystic swelling of the parotid gland.
Case Report
A 42-year-old man was referred to the department of maxillofacial surgery by a general physician because of a swelling of his right parotid gland that had been slowly increasing over 1 year (Fig. 1). He had no history of pain or pus discharge. During primary questioning, the man denied having any sort of multiple sexual exposures, blood transfusions or drug abuse.
Extraoral examination revealed a swelling of the tail lobe of the parotid gland just below the lobule of the patient's right ear. The swelling was firm on palpation. Mouth opening was within normal limits, and there was no cervical lymphadenopathy. On intraoral examination, the mucosa appeared moist and normal. No oral manifestation of HIV was evident. Milking of the left parotid gland produced a copious flow of clear saliva through Stensen's orifice. Aspiration of the lesion produced a colourless fluid with few lymphocytes, not suggestive of any specific pathology.
Magnetic resonance imaging revealed a well-circumscribed cystic lesion, approximately 35 mm in diameter in the superficial lobe of the right parotid gland (Fig. 2). It produced a hyperintense signal on T2-weighted images and a hypointense signal on T1 images, with no associated soft tissue component. In addition, a lesion of approximately 15-mm diameter was noted in the superficial lobe of the left parotid gland and another small exophytic cyst was observed in relation to the deep lobe of the parotid gland just anterior to the stylomastoid foramina. No adenopathy was seen.
 Figure 1: Extraoral view of the parotid swelling.
Figure 1: Extraoral view of the parotid swelling.
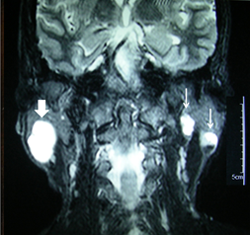 Figure 2: Hyperintense signal in T2-weighted magnetic resonance image showing a well-defined cystic lesion of the right parotid gland (broad arrow). Imaging incidentally revealed 2 cystic lesions in the left parotid gland (narrow arrows).
Figure 2: Hyperintense signal in T2-weighted magnetic resonance image showing a well-defined cystic lesion of the right parotid gland (broad arrow). Imaging incidentally revealed 2 cystic lesions in the left parotid gland (narrow arrows).
A scan using technetium-99m showed normally functioning parotid glands with a normal response to stimuli that increased salivary flow. Analysis of time–activity curves derived from the scintigraphy study looking at regions of interest over each parotid gland showed progressively increasing tracer uptake. After stimulation with oral vitamin C, spontaneous reduction of tracer activity was demonstrated by a fall in both curves, which suggested normally functioning parotid glands.
A provisional diagnosis of multiple lymphoepithelial cysts was made. As the patient denied any history of activity that would suggest an HIV infection, the etiology of the condition was assumed to be developmental. The patient requested removal of the lesion for cosmetic reasons and he was scheduled for surgery. An ELISA test for HIV, which was part of preoperative screening, was positive. The CD4 count was 540/mm3 of blood (normal range: 390–1770/mm3) and the CD8 count was 1200/mm3 (normal range: 240–1200/mm3); however, the CD4:CD8 ratio of 0.45 (normal range 0.9–1.9) indicated a high probability of HIV infection.1 When presented with this serologic evidence, the patient confessed to having visited commercial sex workers multiple times.
A superficial parotidectomy was carried out (Fig. 3). Histopathologic examination revealed multiple cystic lesions lined with squamous epithelium surrounded by fibrous connective tissue, which had been predominantly infiltrated by lymphocytes organized into follicles and germinal centres. The lumen consisted of a pale homogeneous material with foamy macrophages and lymphocytes. Some plasma cells and histiocytes were also seen.
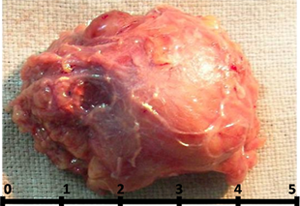 Figure 3: Excised specimen after superficial parotidectomy.
Figure 3: Excised specimen after superficial parotidectomy.
The patient tolerated the procedure well, and the postoperative phase and wound healing were uneventful. For further management of his systemic disease, the patient was referred to a physician who confirmed his positive HIV status by repeating the ELISA test, followed by a protein immunoblot test, and commenced antiretroviral therapy.
Discussion
Salivary gland diseases are important diagnostic and prognostic indicators in HIV infection. Patients with HIV infection have been reported to have parotid swellings2 of various types including salivary gland inflammatory disorders, such as sicca syndrome, diffuse infiltrative lymphocytosis syndrome, parotitis, intraparotid lymphadenopathy and benign lymphoepithelial lesions, as well as salivary gland neoplasms, such as adenoid cystic carcinoma, Kaposi sarcoma and lymphoma.
These lesions may be single or multiple and often become large, causing cosmetic embarrassment and social stigma. Although benign lesions are mostly asymptomatic, they may undergo a lymphomatous transformation; hence, there is need for constant monitoring.3 Lymphoepithelial lesions in the parotid gland are uncommon benign entities with increased incidence associated with HIV infection. The lesions are thought to reflect a localized manifestation of persistent generalized lymphadenopathy associated with HIV infection. However, it remains unclear whether these lesions develop from pre-existing salivary gland inclusions in intraparotid lymph nodes or as a lymphoepithelial lesion of the salivary parenchyma, with different authors presenting different views.4,5
Ryan and colleagues6 first reported a case of parotid swelling in HIV patients in 1985. Since then, many other authors have described various lesions of the parotid gland in HIV-positive patients. Cystic parotid swellings may be a part of diffuse infiltrative lymphocytosis syndrome, a subset of HIV disease characterized by a persistent CD8 lymphocytosis with infiltration of parotid glands, cervical lymph node and viscera by CD8 lymphocytes7 or they may be benign lymphoepithelial cysts.
Various opinions have been presented in the literature regarding the treatment of these lesions. If patients are asymptomatic and do not wish to undergo treatment, periodic observation is an accepted alternative. However, because of the risk of malignant transformation, invasive procedures, such as fine-needle aspiration cytology or biopsy, may be required if clinical examination or imaging raise suspicion.3 Most patients seek treatment for cosmetic reasons.
Pharmacotherapy with anti-retroviral drugs, either alone or with corticosteroids, has been shown to resolve certain lesions of the parotid, especially cases of diffuse infiltrative lymphocytosis syndrome, but many cystic lesions do not respond to pharmacotherapy alone.8 Both low-9 and high-dose radiotherapy regimens10 have been used to treat these lesions, with the drawbacks of high recurrence rates and malignant transformation, respectively. Although aspiration is a useful diagnostic method, it cannot be used as a definitive treatment because its effects are temporary and recurrence is rapid.11 A treatment modality with better reported response is sclerotherapy with doxycycline, which has been used to avoid surgery, especially in the pediatric population.12
Surgery is considered the most definitive modality for treating these lesions. Enucleation, where only the cyst is removed from the surrounding parotid tissue, has resulted in recurrence in certain cases.8 Superficial parotidectomy is considered the treatment of choice,13 albeit with the major risk of facial nerve damage.
Our patient presented with the major concern of the appearance of an asymptomatic swelling and complete denial of any risk factors associated with HIV. The decision to manage the lesion surgically was made without knowledge of his HIV status. Once that status was revealed, discussion of the various treatment options with the patient resulted in a final decision to carry out a superficial parotidectomy. The surgery was successful, and there was no evidence of facial nerve damage or recurrence of the lesion on clinical examination after 1 year follow up. The aim of this article is to emphasize that a patient reporting with a cystic swelling of the parotid gland should raise suspicion of an HIV infection.
THE AUTHORS
References
- Margolick JB, Donnenberg AD, Muñoz A, Park LP, Bauer KD, Giorgi JV, et al. Changes in T and non-T lymphocyte subsets following seroconversion to HIV-1: stable CD3+ and declining CD3− populations suggest regulatory responses linked to loss of CD4 lymphocytes. J Acquir Immune Defic Syndr. 1993;6(2):153-61.
- Schiodt M, Greenspan D, Daniels TE, Leggott PJ, Wara DW, Greenspan JS. Parotid gland enlargement with xerostomia associated with labial sialadenitis in HIV-infected patients. J Autoimmun. 1989;2(4):415-25.
- Mandel L, Hong J. HIV associated parotid lymphoepithelial cysts. J Am Dent Assoc. 1999;130(4):528-32.
- DiGiuseppe JA, Corio RL, Westra WH. Lymphoid infiltrates of the salivary glands: pathology, biology and clinical significance. Curr Opin Oncol. 1996;8(3):232-7.
- Ihrler S, Zietz C, Riederer A, Diebold J, Löhrs U. HIV-related lymphoepithelial cysts. Immunohistochemistry and 3-D reconstruction of surgical and autopsy material with special reference to formal pathogenesis. Virchows Arch. 1996;429(2-3):139-47.
- Ryan J, Ioachim H, Marmer J, Loubeau J. Acquired immune deficiency syndrome — related lymphadenopathies presenting in the salivary gland lymph nodes. Arch Otolaryngol. 1985;111(8):554-6.
- Mandel L, Kim D, Uy C. Parotid gland swelling in HIV diffuse infiltrative CD8 lymphocytosis syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(5):565-8.
- Finfer MD, Schinella RA, Rothstein SG, Persky MS, Cystic parotid lesions in patients at risk for the acquired immunodeficiency syndrome. Arch Otolaryngol Head Neck Surg. 1988;114(11):1290-4.
- Goldstein J, Rubin J, Silver C, Meritz K, Chao C, Ting J, et al. Radiation therapy as a treatment for benign lymphoepithelial parotid cysts in patients infected with human immunodeficiency virus-1. Int J Radiat Oncol Biol Phys. 1992;23(5):1045-50.
- Beitler JJ, Vikram B, Silver CE, Rubin JS, Bello JA, Mitnick RJ, et al. Low-dose radiotherapy for multicystic benign lymphoepithelial lesions of the parotid gland in HIV-positive patients: long-term results. Head Neck. 1995;17(1):31-5.
- Terry JH, Loree TR, Thomas MD, Marti JR. Major salivary gland lymphoepithelial lesions and the acquired immunodeficiency syndrome. Am J Surg. 1991;162(4):324-9.
- Suskind DL, Tavill MA, Handler SD. Doxycycline sclerotherapy of benign lymphoepithelial cysts of the parotid: a minimally invasive treatment. Int J Pediatr Otorhinolaryngol. 2000;52(2):157-61.
- Ferraro FJ, Rush BF, Ruark D, Oleske J. Enucleation of parotid lymphoepithelial cyst in patients who are human immunodeficiency virus positive. Surg Gynecol Obstet. 1993;177(5):524-6.
