ABSTRACT
Currently, there are many options for single-tooth replacement: metal–ceramic, all-ceramic, direct or indirect fibre-reinforced composite fixed dental prostheses (FDPs) or implants. Inlay-retained FDPs may especially be indicated when adjacent teeth have been previously restored and when implant placement is not possible or not indicated. In such cases, both metal–ceramic and fibre-reinforced composite FDPs have certain disadvantages. In this paper, we describe the use of all-ceramic inlay-retained FDPs with zirconia frameworks, veneered using a press-on technique.
Introduction
A number of treatment modalities using various materials exist to replace a missing tooth in the posterior region of the mouth. When patients reject implant therapy, with or without previous reconstructive surgery,1 and in cases where abutment teeth have previously been restored, minimally invasive procedures based on an adhesive approach may offer an alternative to conventional retained full-coverage fixed dental prostheses (FDPs), which require more tooth preparation.2 Pre-existing fillings can minimize the need to remove tooth structure and promote retention of the inlay-retained FDP, making it into a more conservative option than a full coverage metal–ceramic FDP.3 It also allows greater preservation of healthy tooth structure4 and makes periodontal assessment easier.5
Although full-coverage metal–ceramic FDPs are still viewed as the gold standard for tooth replacement, they have disadvantages: decreased likelihood of retention, associated soft-tissue pigmentation and an opaque-to-darkish appearance in the cervical area of the abutment teeth.6 Although alternative, tooth-coloured non-metal materials have been proposed, high-strength pressed ceramics have the potential for debonding7,8 and have insufficient fracture resistance.9 Fibre-reinforced composites may result in fibre exposure10; delamination may occur and hairline microcracks may form in the composite veneering material.11,12
The mechanical properties of yttria tetragonal zirconia polycrystal (Y-TZP), especially those related to its strength, may prevent the failures associated with other metal-free materials. However, zirconia is not etchable by commonly used agents, such as hydrofluoric acid,14 and adhesion to the tooth structure still presents a challenge because of its single-phase tetragonal crystalline structure.
The purpose of this article is to describe clinical procedures related to the placement of inlay-retained FDPs made from a Y-TZP framework veneered with a pressed ceramic and luted with a completely adhesive approach.
Indications and Contraindications
Inlay-retained FDPs are indicated in patients with good oral hygiene and low susceptibility to caries, who have a minimum coronal tooth height of 5 mm, parallel abutments and a maximum mesiodistal edentulous gap of 12 mm (Fig. 1). Contraindications include severe parafunctions, the absence of enamel on the preparation margins, extensive crown defects and abutment-tooth mobility.
Preparation
The cavity is prepared for inlay-retained zirconia FDPs according to the following guidelines:
- occlusal depth: 2.5 mm (floor of isthmus to central groove)
- vestibular–palatal/lingual width of the intercuspal isthmus: 3 mm
- depth of proximal box: 2 mm (shoulder with rounded internal angle)
- buccal vestibular width: maximum of 4.5 mm (3 mm of zirconia framework and 0.5–0.6 mm of ceramic veneer on each side)
- minimum dimensions of connectors: 3 × 3 mm
- cusps are included in the preparation when an abutment tooth has a wide bucco-oral defect (> 50%) or has been devitalized
- divergence angle of the cavity: approximately 6° (Fig. 2)
 Figure 1: Baseline status of a representative case in which an inlay-retained fixed dental prosthesis (FDP) was indicated for restoring a missing tooth. Note the insufficient interdental bone.
Figure 1: Baseline status of a representative case in which an inlay-retained fixed dental prosthesis (FDP) was indicated for restoring a missing tooth. Note the insufficient interdental bone.
 Figure 2: Occlusal view of cavities made in abutment teeth framed by rubber dam. The conservative approach has to respect the guidelines for cavity preparation.
Figure 2: Occlusal view of cavities made in abutment teeth framed by rubber dam. The conservative approach has to respect the guidelines for cavity preparation.
Options for the Framework Design
After impressions are made and gypsum or epoxy models are poured, 2 design options for zirconia frameworks may be considered based on the depth of the prepared cavity:
- Cavity depth 2.5 to 3.3 mm: The zirconia framework lies on the cavity floor and has a reduced circumference, leaving space for etchable glass ceramic at the margins (Figs. 3a and 3b).
- Cavity depth > 3.3 mm: The zirconia framework is enclosed by overpressed ceramic (Figs. 3c and 3d); thus, all inner surfaces of the retainer are covered by the etchable glass ceramic.
 Figure 3a: Zirconia framework after milling.
Figure 3a: Zirconia framework after milling.
 Figure 3b: Ceramic veneer pressed onto zirconia framework before glazing.
Figure 3b: Ceramic veneer pressed onto zirconia framework before glazing.
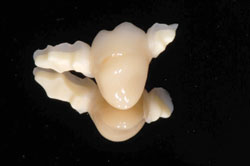 Figure 3c: Inlay retained zirconia framework veneered with pressable ceramic. Note that all margins are etchable with hydrofluoric acid.
Figure 3c: Inlay retained zirconia framework veneered with pressable ceramic. Note that all margins are etchable with hydrofluoric acid.
 Figure 3d: Finished inlay-retained FDP on the epoxy resin model.
Figure 3d: Finished inlay-retained FDP on the epoxy resin model.
Luting Procedures
FDP Conditioning
Ceramic surfaces are etched with 9.6% hydrofluoric acid for 60 seconds, rinsed for 60 seconds and dried. The ceramic surfaces are treated with silane coupling agent for 5 minutes at 60°C, then a single layer of bonding agent is applied and air thinned.
Cavity Conditioning
The enamel and dentin surfaces are then etched with 35% phosphoric acid for 30 seconds and 15 seconds, respectively. Etching gel is removed by rinsing for 20 seconds with an air/water spray, and primer from the same adhesive system used for the FDP is applied for 20 seconds and gently evaporated. The bonding agent is applied with a microbrush, but not polymerized.
Insertion
A 2-mm layer of restorative composite material, previously heated to 60°C, is placed in the cavity with a spatula. Following removal of excess composite, it is polymerized on each side (Fig. 4). Excess luting material is removed using a scaler and the margins are finished using composite polishing points. Figure 5 shows the FDP at follow-up after 3 years.
 Figure 4: Inlay-retained FDP after luting procedures.
Figure 4: Inlay-retained FDP after luting procedures.
 Figure 5: Lingual view of inlay-retained FDP after 3 years of service.
Figure 5: Lingual view of inlay-retained FDP after 3 years of service.
Discussion
Inlay-retained FDPs should be considered when implants are not indicated or are considered too expensive. Furthermore, in implant dentistry, the problems of peri-implantitis and marginal bone loss around implants have not been thoroughly solved.15 Inlay-retained FDPs may be considered a conservative alternative to complete coverage FDPs. Although macromechanical retention might give complete coverage FDPs a long survival rate, biological complications, such as caries around the restorations, loss of vitality or periodontal problems are commonly reported.2 When abutment teeth contain restorative fillings adjacent to the missing tooth, inlay-retained FDPs should be considered as they require only minimum removal of tooth structure beyond the filling extension. The techniques described in this article may address the problem of debonding of metal–ceramic inlay retained FDPs16 or indirect fibre-reinforced composite FDPs.17 Although direct fibre-reinforced composite FDPs do not seem to suffer from debonding,18 their fabrication is technically more difficult. Moreover, ceramics have the advantages of high polishability and good colour match. In the case of a fracture, they may be repaired intraorally with durable results.19,20
Conclusion
Inlay-retained FDPs allow for single-tooth substitution when implant placement is not possible or not indicated. The bone-tissue loss during implantation and tooth-tissue loss during preparation of abutment teeth needed for full coverage FDPs can be avoided. The use of a press-on ceramic for marginal or full contouring of the retainer, allowing an adhesive approach, may enhance the long-term stability of such restorations.
THE AUTHORS
References
- Misch CE, Misch-Dietsh F, Silc J, Barboza E, Cianciola LJ, Kazor C. Posterior implant single-tooth replacement and status of adjacent teeth during a 10-year period: a retrospective report. J Periodontol. 2008;79(12):2378-82.
- Sailer I, Pjetursson BE, Zwahlen M, Hammerle CH. A systematic review of the survival and complication rates of all-ceramic and metal–ceramic reconstructions after an observation period of at least 3 years. Part II: fixed dental prostheses. Clin Oral Implants Res. 2007;18(Suppl. 3):86-96.
- Edelhoff D, Spiekermann H, Yildirim M. Metal-free inlay-retained fixed partial dentures. Quintessence Int. 2001;32(4):269-81.
- Edelhoff D, Sorensen JA. Tooth structure removal associated with various preparation designs for posterior teeth. Int J Periodontics Restorative Dent. 2002;22(3):241-9.
- Freilich MA, Niekrash CE, Katz RV, Simonsen RJ. Periodontal effects of fixed partial denture retainer margins: configuration and location. J Prosthet Dent. 1992;67(2):184-90.
- Tan K, Pjetursson BE, Lang NP, Chan ES. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15(6):654-66.
- Sorensen JA, Cruz M, Mito WT, Raffeiner O, Meredith HR, Foser HP. A clinical investigation on three-unit fixed partial dentures fabricated with lithium disilicate glass-ceramic. Pract Periodontics Aesthet Dent. 1999;11(1):95-106.
- Wolfart S, Bohlsen F, Wegner SM, Kern M. A preliminary prospective evaluation of all-ceramic crown-retained and inlay-retained fixed partial dentures. Int J Prosthodont. 2005;18(6):497-505.
- Kiliçarslan MA, Kedici PS, Küçükeşmen HC, Uludağ BC. In vitro fracture resistance of posterior metal–ceramic and all-ceramic inlay-retained resin-bonded fixed partial dentures. J Prosthet Dent. 2004;92(4):365-70.
- Göhring TN, Roos M. Inlay-fixed partial dentures adhesively retained and reinforced by glass fibers: clinical and scanning electron microscopy analysis after five years. Eur J Oral Sci. 2005;113(1):60-9.
- Monaco C, Ferrari M, Caldari M, Baldissara P, Scotti R. Comparison of 2 bonding systems and survival of fiber-reinforced composite inlay fixed partial dentures. J Prosthodont. 2006;19(6):577-85.
- Monaco C, Krejci I, Bortolotto T, Perakis N, Ferrari M, Scotti R. Marginal adaptation of 1 fiber-reinforced composite and 2 all-ceramic inlay fixed partial denture systems. Int J Prosthodont. 2006;19(4):373-82.
- Ohlmann B, Rammelsberg P, Schmitter M, Schwarz S, Gabbert O. All-ceramic inlay-retained fixed partial dentures: preliminary results from a clinical study. J Dent. 2008;36(9):692-6. Epub 2008 Jun 11.
- Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008;24(3):299-307. Epub 2007 Jul 19.
- Meffert RM. Periodontitis and periimplantitis: one and the same? Pract Periodontics Aesthet Dent. 1993;5(9):79-80, 82.
- Creugers NH, Käyser AF, Van't Hof MA. A seven-and-a-half-year survival study of resin-bonded bridges. J Dent Res. 1992;71(11):1822-5.
- van Heumen CC, van Dijken JW, Tanner J, Pikaar R, Lassila LV, Creugers NH, et al. Five-year survival of 3-unit fiber-reinforced composite fixed partial dentures in the anterior area. Dent Mater. 2009;25(6):820-7. Epub 2009 Mar 31.
- Özcan M. Direct, inlay-retained, fiber-reinforced-composite restorations with two pontics: 5-year clinical follow-up. J Dent Res. 2008;87(Special Issue B):Abstract 1605.
- Özcan M, Niedermeier W. Clinical study on the reasons for and location of failures of metal–ceramic restorations and survival of repairs. Int J Prosthodont. 2002;15(3):299-302.
- Bagis B, Ustaomer S, Lassila LV, Vallittu PK. Provisional repair of a zirconia fixed partial denture with fibre-reinforced restorative composite: a clinical report. J Can Dent Assoc. 2009:75(2);133-7.
