ABSTRACT
A large maxillary cyst was treated for 3 months with marsupialization and decompression, followed by surgical endodontic therapy of the affected teeth and cystectomy. Although small cystic lesions will typically heal with nonsurgical endodontic therapy, larger lesions may need additional treatment. Surgical enucleation of a large cystic lesion may lead to damage of other teeth or anatomic structures. Therefore, treatment should begin with the more conservative approach of decompression, to reduce the size of the lesion, followed by apicoectomy and cystectomy.
Introduction
Traumatic injuries to the teeth are relatively common, usually involving the anterior teeth of young patients. Such trauma is often followed by pulpal necrosis. If microbial infection occurs, a periapical lesion may develop, possibly evolving into a chronic inflammatory lesion (e.g., granuloma, periapical cyst or scar tissue). Periapical or radicular cysts are inflammatory jaw cysts affecting teeth with infected and necrotic pulp. These cysts occur as the direct sequelae of chronic apical periodontitis. Although the reported prevalence of cysts developing from apical periodontitis lesions varies from 6% to 55%, investigations based on meticulous serial sectioning and strict histopathologic criteria show that their actual prevalence is well below 20%.1
Most radicular cysts develop slowly and do not become very large. Patients do not experience pain unless acute inflammatory exacerbation is present, and the lesions are often detected only during routine radiographic examination. If the cyst does become large, symptoms such as swelling, mild sensitivity, tooth mobility and displacement may be observed. The affected tooth is nonresponsive to thermal and electrical pulp tests.2
The following case report describes the management of a particularly large maxillary cyst (involving 5 anterior teeth) by marsupialization with decompression, followed by surgical endodontic therapy and cystectomy.
Case Report
A healthy 15-year-old male was referred to the dental clinic of the faculty of dentistry of Sevilla (Spain) for treatment of a large periapical lesion around the left maxillary central incisor. The tooth was discoloured and had undergone previous filling of the root because of irreversible pulpitis following a traumatic injury. Orthopantomography (Fig. 1) revealed a large periapical radiolucency, about 4 cm in the horizontal plane and 3 cm in the vertical plane, associated with teeth 21, 22, 23, 24 and possibly 25. Clinical examination revealed labial swelling over these teeth, and the area was tender to palpation and percussion. Teeth 22, 23 and 24 did not respond to thermal and electrical pulp tests. The provisional diagnosis was radicular cyst.
Computed tomography (CT) revealed a lesion about 4 cm wide in the anteroposterior plane affecting the entire right premaxilla and contacting the floor of the nose and the maxillary sinus (Fig. 2). Swelling, a buccal cortical break and expansion of the bone were obvious; these features indicated that the lesion was benign.
 Figure 1: Panoramic radiograph for a patient with a large periapical lesion around the left maxillary central incisor.
Figure 1: Panoramic radiograph for a patient with a large periapical lesion around the left maxillary central incisor.
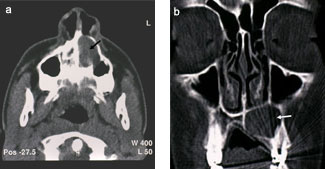 Figure 2: Maxillary computed tomography: (a) transverse plane and (b) coronal plane. The arrow in each scan points to the cystic lesion.
Figure 2: Maxillary computed tomography: (a) transverse plane and (b) coronal plane. The arrow in each scan points to the cystic lesion.
Cystectomy was considered, but the disadvantages of this treatment included the need to perform root canal treatment and apicoectomy of all affected teeth, possible damage to the floor of the nose or the maxillary sinus, and the need for general anesthesia. After consultation with the patient, his parents and various specialists, marsupialization with decompression was selected as an alternative approach. Specifically, the treatment plan called for decompression over a minimum of 12 weeks, followed by root canal treatment of teeth 22, 23 and 24, apicoectomy of teeth 21, 22 and 23, and enucleation of the residual lesion.
After infiltration of anesthetic, a Neumann trapezoidal flap was created between the root eminences of teeth 11 and 23. Upon entry into the cyst cavity, there was copious drainage of the typical straw-coloured fluid associated with cystic lesions of inflammatory origin, without purulent secretion (Fig. 3). Lavage with sterile saline was performed, and a sample of the cystic capsule was taken for biopsy; histologic examination confirmed the diagnosis of inflammatory cyst. An orifice was created through the mucosa, and a 2-cm length of no. 10 French radiopaque latex tubing was inserted to the depth of the cystic cavity. Two 4-0 gut sutures were placed, one above and the other below the drain. A third suture was placed through the drain and the surrounding mucosa to stabilize the drain during the initial healing (Fig. 4). The patient was instructed to irrigate through the lumen of the latex tubing 3 times a day with chlorhexidine 0.12%, consistent with a published protocol.3
After 3 months, radiographic examination revealed substantial healing (Fig. 5). Specifically, trabecular bone was forming and the radiolucent area had diminished, as had the distances between the cyst and the nasal cavity and the maxillary sinus. However, healing was still incomplete, and surgical endodontic therapy and enucleation of the cyst were indicated.
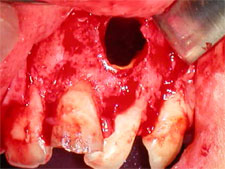 Figure 3: Appearance of the cavity created when the cyst was opened and drained.
Figure 3: Appearance of the cavity created when the cyst was opened and drained.
 Figure 4: Clinical image after insertion of a radiopaque latex drain into the cavity.
Figure 4: Clinical image after insertion of a radiopaque latex drain into the cavity.
 Figure 5: Panoramic radiograph after decompression.
Figure 5: Panoramic radiograph after decompression.
Endodontic treatment of teeth 22 to 24 was performed. Briefly, following local anesthesia and isolation with a rubber dam, an endodontic access cavity was created. The root length was estimated with an apex locator (AFA Apex Finder, Analytic Technology, Orange County, CA) and confirmed by periapical radiography. After apical patency was established, the canal of each tooth (2 canals in tooth 24) was cleaned, shaped, dried and obturated by cold lateral condensation of gutta-percha (Dentsply Maillefer, Ballaigues, Switzerland) and sealer (AH Plus, Dentsply DeTrey, Konstanz, Germany). The access openings of the teeth were filled with acid-etched composite resins.
Six days later, cystectomy was performed under local anesthesia. The buccal flaps were raised, and the cyst was enucleated. A full histologic study of the cystic capsule, performed to exclude any other tumour type, confirmed the previous diagnosis of inflammatory cyst. The drain was removed, the mucosal orifice was sutured, and apicoectomy of teeth 21, 22 and 23 was performed (Figs. 6a, 6b and 7).
One week after the operation, the surgical sites showed good healing (Fig. 8). Clinical examinations at 1, 3 and 6 months showed no sensitivity to percussion or palpation, and the soft tissues were healthy. After 8 months, clinical healing and radiographic resolution of the maxillary radiolucency were complete (Figs. 9 and 10).
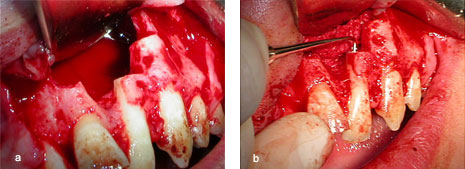 Figures 6a and 6b: Enucleation of the cyst and apicoectomy of teeth 21, 22 and 23.
Figures 6a and 6b: Enucleation of the cyst and apicoectomy of teeth 21, 22 and 23.
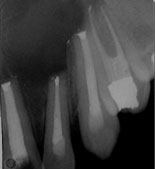 Figure 7: Periapical radiographs after apicoectomy.
Figure 7: Periapical radiographs after apicoectomy.
 Figure 8: Clinical image 1 week after the operation.
Figure 8: Clinical image 1 week after the operation.
 Figure 9: Panoramic radiograph 8 months after the operation.
Figure 9: Panoramic radiograph 8 months after the operation.
 Figure 10: Clinical image 8 months after the operation.
Figure 10: Clinical image 8 months after the operation.
Discussion
A wide variety of cysts and neoplasms may occur in the maxillofacial region, and their identification can be difficult. The most important of these are maxillary cysts.1 A cyst is a pathological cavity with a defined wall of connective tissue and an epithelial carpet, filled with liquid, semiliquid or gaseous content. Growth of a cyst is typically slow, centrifugal and infiltrative.4 Radicular cysts are thought to arise from epithelial cell rests of Malassez in the periodontal ligament, and they are believed to proliferate as a result of periapical inflammation caused by infection of the root canal system. They are particularly frequent in the maxillary anterior region, presumably as a result of trauma.5
The management of large cystic lesions has been the subject of prolonged debate.6 The treatment options for large periapical lesions range from conventional nonsurgical root canal treatment with long-term calcium hydroxide therapy to various surgical interventions. Some endodontists maintain that true cysts (those containing cavities completely enclosed by epithelial lining) can be successfully treated only by surgical means,7 but the current endodontic philosophy for the treatment of large periapical lesions involves initial use of nonsurgical root canal treatment.8 Such treatment is not always successful, and epidemiological studies of the Spanish population have shown a high prevalence of root-filled teeth with chronic apical periodontitis.9,10 Therefore, patients should undergo clinical and radiological evaluation 6 months after the initial root canal treatment, to verify resolution of the lesion. However, a variety of scenarios may lead to the need for further surgical treatment of a lesion that presents greater compromise to the adjacent structures than was the case in the initial stages.6 For example, the original diagnosis may have been incorrect, or the initial treatment may have been unsuccessful but the patient does not return until the situation has worsened and symptoms have reappeared. In this situation, additional options must be considered, such as nonsurgical retreatment or periapical surgery.
For several reasons, surgical treatment may be the preferred approach to treating a large periapical cyst. For example, if the apical radiolucency is very large (diameter > 20 mm or cross-sectional area > 200 mm2), surgical removal may be the best option.11 Long-standing infection and necrosis of the pulp causing a large apical radiolucency may be deemed refractory to conventional treatment because of the high probability that the lesion is a cyst.12 Surgical treatment may also be recommended when the canal appears “calcified” or obstructed and cannot be negotiated with instruments. This is often assumed to be the case when the canal cannot be visualized radiographically, particularly if root-end surgery has already been performed. Failure of treatment with a metal obturating material is yet another reason for surgery.
The usual surgical treatments for radicular cyst include total enucleation of small lesions, marsupialization for decompression of larger cysts or a combination of these techniques. Should surgical intervention become necessary, the clinician must decide whether to raise a flap and completely enucleate the lesion or to try “decompression” first.13,14 If marsupialization with decompression is attempted first, the size of the lesion will be reduced, which will make it less difficult to remove, with less risk of damage to the associated teeth and vital structures.15 For the case reported here, the surgical literature clearly indicated enucleation of the cyst as the preferred option, because marsupialization carries the risk that any cystic cells left behind may become malignant.16,17 However, for this patient, it was felt that marsupialization was the best treatment option, thus avoiding the risk of damage to the floor of the nose or the maxillary sinus, and the need for general anesthesia.
In the debate over surgical versus nonsurgical options, surgeons may point to the diagnostic value of periapical surgery in confirming the diagnosis. This raises the issue of whether a dentist should recommend enucleation and biopsy of periapical lesions of apparently endodontic origin or whether conservative treatment should be attempted, with surgery being suggested only if there is doubt regarding the endodontic origin of the lesions. The literature offers no clear answer to this dilemma. The divergence of criteria and results is probably related to the presence of both periapical lesions and true periapical cysts in the cases that have been analyzed. Periapical cysts have an epithelial covering and expansive growth but still communicate with the root apex and could therefore be referred to as pseudocysts. A certain percentage of these pseudocysts become involuted with adequate canal treatment. In contrast, true periapical cysts have no communication with the root canal.
When the lesions are very extensive, as in the case reported here, the undesirable consequences of surgical curettage have led to the use of a tube decompression procedure, followed by apicoectomy and enucleation of the cyst. The marsupialization and decompression techniques are intended to reduce the size of the lesion.18 However, they depend on the patient’s cooperation, they take a long time, and they do not maintain the basic principles of endodontic therapy, especially with regard to preventing bacterial contamination throughout the oral environment. The percentage of radicular cysts that can be expected to heal with marsupialization and decompression alone is unknown, but this treatment modality bears consideration for the treatment of large, presumptively cystic lesions.15 Furthermore, the decompression technique has been proposed as an alternative to apical surgery for large areas of rarefaction involving anatomic structures.15 However, we suggest that decompression be considered only as the first phase in treating large cystic lesions, with the intention of reducing the size of the lesion and facilitating subsequent surgical procedures.
In the case reported here, a steady decrease in the radiolucent area was apparent after 3 months of marsupialization and decompression, and cystectomy was performed easily. Resolution of the lesion was complete after 8 months.
THE AUTHORS
References
- Nair PN, Sundqvist G, Sjögren U. Experimental evidence supports the abscess theory of development of radicular cysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):294-303. Epub 2008 Jun 13.
- Lin LM, Ricucci D, Lin J, Rosenberg PA. Nonsurgical root canal therapy of large cyst-like inflammatory periapical lesions and inflammatory apical cysts. J Endod. 2009;35(5):607-15.
- Brondum N, Jensen VJ. Recurrence of keratocysts and decompression treatment. A long-term follow-up of forty-four cases. Oral Surg Oral Med Oral Pathol. 1991;72(3):265-9.
- Asián-González E, Pereira-Maestre M, Conde-Fernández D, Vilchez I, Segura-Egea JJ, Gutiérrez-Pérez JL. Dentigerous cyst associated with a formocresol pulpotomized deciduous molar. J Endod. 2007;33(4):488-92. Epub 2007 Jan 4.
- Lin LM, Huang GT, Rosenberg PA. Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 2007;33(8):908-16. Epub 2007 Apr 2.
- Gallego Romero D, Torres Lagares D, García Calderón M, Romero Ruiz MM, Infante Cossio P, Gutiérrez Pérez JL. Differential diagnosis and therapeutic approach to periapical cysts in daily dental practice. [Article in English, Spanish]. Med Oral. 2002;7(1):54-62.
- Nair PN, Sjögren U, Schumacher E, Sundqvist G. Radicular cysts affecting a root-filled human tooth: a long-term post-treatment follow-up. Int Endod J. 1993;26(4):225-33.
- Çaliskan MK. Prognosis of large cyst-like periapical lesions following nonsurgical root canal treatment: a clinical review. Int Endod J. 2004;37(6):408-16.
- Jiménez-Pinzon A, Segura-Egea JJ, Poyato-Ferrera M, Velasco-Ortega E, Ríos-Santos JV. Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. Int Endod J. 2004; 37(3):167-73.
- Segura-Egea JJ, Jiménez-Pinzón A, Poyato-Ferrera M, Velasco-Ortega E, Ríos-Santos JV. Periapical status and quality of root fillings and coronal restorations in an adult Spanish population. Int Endod J. 37(8):525-30.
- Ramachandran Nair PN, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(1):93-102.
- Lalonde ER, Luebke RG. The frequency and distribution of periapical cysts and granulomas: an evaluation of 800 specimens. Oral Surg Oral Med Oral Pathol. 1968;25(6):861-8.
- Freedland JB. Conservative reduction of large periapical lesions. Oral Surg Oral Med Oral Pathol. 1970;29(3):455-64.
- Neaverth EJ, Burg HA. Decompression of large periapical cystic lesions. J Endod. 1982;8(4):175-82.
- Martin SA. Conventional endodontic therapy of upper central incisor combined with cyst decompression: a case report. J Endod. 2007;33(6):753-7. Epub 2007 Mar 21.
- Gardner AF. A survey of odontogenic cysts and their relationship to squamous cell carcinoma. Dent J. 1975;41(3):161-7.
- Schneider LC. Incidence of epithelial atypia in radicular cysts: a preliminary investigation. J Oral Surg. 1977;35(5):370-4.
- Mejia JL, Donado JE, Basrani B. Active nonsurgical decompression of large periapical lesions – 3 case reports. J Can Dent Assoc. 2004;70(10):691-4.
