Abstract
Objective: This study was undertaken to determine the effect of temperature on the microhardness and viscosity of 4 resin composite materials.
Methods: To investigate microhardness, samples of each of the 4 composite materials, prepared by standard insertion of resin into prefabricated moulds, were divided into 2 groups (n = 10 per group). On the first group, the resin composite materials were inserted into the moulds at room temperature and cured. On the second group, the resin composite materials were pre-heated in a heating device, inserted into the moulds and immediately cured. Microhardness after curing (both immediately and after 24 hours of storage) was determined (using a 300g load applied for 10 seconds) and averaged for 5 randomly selected points on the top and bottom surfaces of each sample. To investigate viscosity, 0.5 g samples of room temperature or preheated resin composite (n = 15 per group) were placed under a 454 g load for 45 seconds before light-curing (40 seconds). After curing, each sample was photographed and the surface area calculated. Data were analyzed by t tests or one-way analysis of variance and Tukey’s test.
Results: Preheating the resin composites increased the microhardness and decreased the viscosity of the samples. Filtek Supreme Ultra resin composite had the highest mean microhardness, and Vit-l-escence resin composite had the lowest viscosity.
Conclusions: The effects of preheating resin composites may allow easier placement of restorations and greater monomer conversion.
Despite improvements in resin composite materials, some drawbacks still compromise the longevity of resin composite restorations. The most frequently reported limitations are related to shrinkage during polymerization, mismatch in thermal expansion, resistance to abrasion and wear, toxicity, marginal leakage and recurrent caries.1-5
To overcome these problems, attempts have been made to improve the mechanical properties of these materials, including changes in the amount, size and type of fillers and/or the use of non-methalcrylate-based monomers. As well, different clinical procedures have been proposed to compensate for the stress associated with polymerization shrinkage and to facilitate better marginal adaptation between the resin composite and the cavity walls. Several techniques for placing restorations6-9 have been suggested to improve the seal of resin composite restorations, such as incremental layering to reduce the configuration factor, 10 soft-start and pulsed-curing methods to modify the reaction rate11 and use of flowable composites to promote better marginal adaptation.7,8 Flowable composites, with their marked fluidity, have been frequently advocated as stress absorbers and adaptation promoters.7-9,12,13 However, because of the lower filler content of flowable composite materials, greater polymerization-induced stress is expected relative to standard resin composites.14-16
Studies have suggested that heating traditional resin composites can improve marginal adaptation by enhancing fluidity.16,17 In addition, preheating composites may improve their physical and mechanical properties through a higher degree of monomer conversion,14,18-22 which has in turn been associated with greater mechanical strength, rigidity and resistance to degradation in the oral environment.23 Conversely, incomplete polymerization can lead to increased wear due to reduced mechanical strength, and unreacted monomers may be cytotoxic, leading to allergic and sensitivity reactions.24
Microhardness has often been used to assess the physical properties of restorative materials, and this property correlates well with the degree of conversion of resin composites.23,25-28 Therefore, this study was undertaken to determine the effect of preheating on microhardness (measured as Knoop hardness number [KHN]) and viscosity (measured as area after compression) of 4 resin composite materials. The following null hypotheses were considered:
1. There is no significant difference in mean postcuring microhardness between preheated samples of resin composite and samples cured at room temperature without preheating.
2. There is no significant difference in mean postcuring microhardness among different resin composite restorative materials.
3. There is no significant difference in the viscosity of different resin composites under different temperature conditions.
Materials and Methods
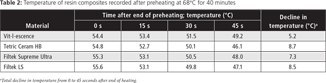
Microhardness
Four resin composite restorative materials (Table 1), 3 methacrylate-based composites and 1 silorane-based composite, were used to prepare a total of 80 disk-shaped samples (20 samples of each composite). The samples were prepared by inserting uncured resin composite into circular metallic moulds (5 mm diameter × 2 mm height). The moulds were covered with a polyester strip and a clear glass cover slip (Micro Slides, Gold Seal) on both upper and lower surfaces to remove excess material and standardize surface finishing. The samples of each composite were divided into 2 groups of 10 samples each. For each composite, one group of samples was light-cured at room temperature (24°C ± 1°C) without pretreatment, and the other group was light-cured after preheating. Light-curing was applied to the top surface of each sample for 40 seconds with a light-emitting diode curing unit (Valo, Ultradent). The light intensity was nominally 1200 mW/cm2 and was checked with a radiometer (Patterson curing light meter). For the 4 groups of samples that were preheated before light-curing, each resin composite material was placed in a heating device (CalSet 3 temperature unit, AdDent) for 40 minutes at the highest setting (68°C). Each resin composite material was inserted into the mould within 45 seconds after removal from the heating device. The metallic moulds, clear glass cover slips and plastic filling instrument were all warmed to 37°C before insertion of the resin. The internal temperature of each preheated sample was determined by inserting a thermometer (HRC5A Heater Controller, Thermocouple) into the resin composite syringe after the warming period. To determine the rate of heat loss, additional temperature measurements were performed after 15, 30 and 45 seconds (Table 2). The surface microhardness was measured on the top and bottom surfaces of each specimen (Knoop diamond with a 300 g load for 10 seconds; Micromet, Buehler). Five randomly selected points for each surface were measured immediately and 24 hours after curing. Between measurements, the samples were stored at 37°C in distilled water in a darkened incubator.
NOTE: Click to enlarge tables.
Viscosity
The viscosity of each of the 4 resin composites was measured at room temperature with and without preheating. Preheating (to the same temperature as used for the microhardness tests) was accomplished with a hot platform (Advanced Hot Plate Stirrers, VWR). Sample temperature was verified with a thermometer (HRC5A Heater Controller, Thermocouple). Viscosity was determined by calculating and comparing the surface area of 0.5 g samples of each material. Each sample (n = 15 for each material) was placed between 2 glass slides under a load of 454 g for 45 seconds to obtain a flat surface before light-curing for 40 seconds with the same light-curing unit described above. After curing, a digital photograph of each sample was obtained and the surface area calculated using Image J software (version 1.44, National Institutes of Health, http://rsbweb.nih.gov/ij/).
Data were recorded in an Excel spreadsheet (Microsoft Corp, Redmond, WA) and then imported into SPSS (IBM, Armonk, NY) for analysis. Three-way analysis of variance(ANOVA) with the factors of material, time and preheating for both top and bottom surfaces was used to compare microhardness measurements, and 2-way ANOVA with the factors of material and temperature was used to compare viscosity measurements. Because of significant interaction terms for both of these analyses, one-way ANOVA was used to test for significant differences among the 4 composite materials. Tukey’s test was applied for pairwise comparisons when the ANOVA result was significant. Student t tests with Bonferroni correction (p ≤ 0.017) was used to compare microhardness and viscosity measurements of samples cured at room temperature with samples of the same material cured after preheating.
Results
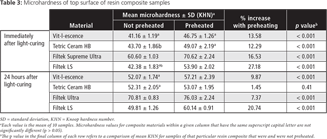
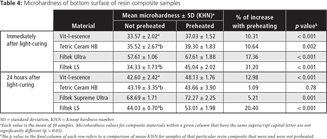
Microhardness
For all but one of the resin composite materials, mean microhardness of both the top (Table 3) and the bottom (Table 4) surfaces increased significantly with preheating. The exception to this general finding was Tetric Ceram HB. Although there was a significant increase in microhardness on the top and bottom surfaces of samples of this resin composite immediately after curing, no significant increase was evident on either surface after 24 hours.
Of the 4 resin composite materials tested, Filtek Supreme Ultra displayed the highest microhardness values under the various experimental conditions.
Viscosity
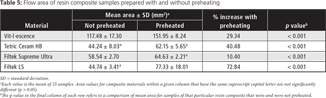
Preheating resin composites resulted in a statistically significant decrease in viscosity for all resin composites tested (Table 5). The materials with the highest viscosity (smallest area) at room temperature were Tetric Ceram HB (area 44.24 ± 8.03 mm2) and Filtek LS (area 44.74 ± 3.41 mm2), with no statistically significant difference between them. Vit-l-escence exhibited the lowest viscosity at both temperatures.
Discussion
Microhardness
On the basis of the results reported here, the first null hypothesis, stating that there is no significant difference in mean postcuring microhardness between samples of resin composite that have been preheated and those cured at room temperature without preheating, should be rejected. For all 4 resin composites used in the present study, mean microhardness increased with preheating, on both top and bottom surfaces of the samples. These findings are in accordance with the results of previous studies.26,28-32 The increase in mean microhardness of the top surface attained with preheating ranged from 1.45% (Tetric Ceram HB, after 24 hours of storage) to 27.18% (Filtek LS, immediately after curing). For the bottom surface, the increase in microhardness ranged from 1.09% (Tetric Ceram HB, after 24 hours of storage) to 31.20% (Filtek LS, immediately after curing). All of the increases were statistically significant, except that for Tetric Ceram HB resin composite after 24 hours of storage.
As noted above, an increase in mean microhardness was observed after 24 hours of storage (except with Tetric Ceram HB resin composite). This finding is in agreement with the results of other studies,21,25,27 which have highlighted that polymerization starts immediately after light exposure and continues for 24 hours and that during this period, a reduction in the number of free radicals and a slight but significant increase in the degree of conversion is observed. Post-irradiation curing occurs because of unreacted species with free radicals that become trapped within the more rigid network during polymerization.19 The trapped radicals are the result of self-deceleration, which takes place because of reduced mobility of both monomer and unreacted pendant double bonds in the viscous media. As the polymerization reaction progresses, both propagation and termination reactions become diffusion-controlled.19-21,33-35 Over time, these residual unpolymerized species find pendant groups and are involved in further reaction. The post-irradiation hardening pattern achieved by resin composites is characterized by enhanced polymer cross-linking.20
The greater increase in microhardness achieved at the top surface of samples relative to the bottom surface can be explained by the attenuation of light (because of reflection, absorption and dispersion phenomena) as it travels through the composite. In the current study, microhardness at the top and bottom surfaces was measured at 2 mm depth, the suggested increment thickness for composite placement.9,19 At a depth of 2 mm, the attenuation of light may reduce irradiance to approximately 75% of that reaching the top surface.9,32
It has been reported that, on average, resin composites can achieve 50% to 70% conversion of monomers at room temperature.36 During polymerization, monomer conversion occurs as soon as exposure to light is initiated. As the reaction progresses, the viscosity of the resin composite increases through the formation and growth of polymer chains, which result in decreased molecular movement. The increased viscosity prevents completion of the polymerization process because movement of molecules in this vitrified state becomes limited.14,19 Conversely, preheated composites exhibit increased monomer mobility, as a result of higher thermal energy, which leads to less viscosity and enhanced molecular motion.14,26,29,37 Also, any delay in both propagation and termination of diffusion-controlled reactions will permit enhanced conversion. Such delay will result in a greater number of collisions, since free radicals are able to diffuse and react before self-deceleration occurs, which in turn increases the degree of monomer conversion before vitrification.14,19,22,31,33 Daronch and colleagues18 suggested that curing time may be reduced by up to 75% with preheating of composites. These authors reported that light-curing of a warmed resin composite for 5 seconds resulted in a greater degree of conversion than light-curing at room temperature for 40 seconds. Furthermore, in another study,19 these authors showed that when resin composites were polymerized at 3°C, the final conversion was less than 35%. The decreased monomer conversion achieved at lower temperatures (e.g., when resin composites are stored in the refrigerator) was attributed to the higher viscosity of the material, which resulted in slower propagation. A correlation between monomer conversion and Knoop hardness values has been reported in several studies.20,25,23,30,31 In one recent study,25 the microhardness test was more sensitive than Fourier transform infrared spectroscopy in identifying small changes in monomer conversion after 24 hours.
In the current study, the maximum resin temperature achieved after 40 minutes of heating at 68°C ranged from a low of 54.4°C (Vit-l-escence) to a high of 55.6°C (Filtek LS). After 45 seconds, the average temperature decline ranged from 5.2°C to 8.7°C (Table 2). Heat loss was also reported in several other studies.19,28,29,33,37 Daronch and colleagues18 reported that even when preheated composites had cooled to below 54°C, monomer conversion was still superior to that achieved by resin composites cured at room temperature.
The second null hypothesis, stating that there are no significant differences in mean postcuring microhardness among the different resin composites tested, was also rejected. The Filtek Supreme Ultra resin composite exhibited the highest mean microhardness under the various experimental conditions investigated, and its microhardness was significantly greater than that of the other materials (Table 3 and 4). These findings are in agreement with another study, in which the same resin composite was used.28 The high microhardness values achieved by Filtek Supreme Ultra resin composite may be related to the amount and type of filler. This material has a high filler content (72.5 % by weight) and employs nanofiller technology. Eliades and colleagues20 also found that hardness patterns are extended as inorganic loading increases.
This study included a silorane-based resin composite (Filtek LS) for comparison with the methacrylate-based composites. Silorane resin composite contains a siloxane backbone with 4 attached oxirane rings that open to form a polymer chain, which offsets the shrinkage resulting from monomer conversion into polymer.38 Other studies have reported similar mechanical properties of siloranes relative to methacrylate-based composites.38,39 In the present study, the mean microhardness of the silorane-based resin composite was similar to that of the methacrylate-based composites tested, which is in accordance with previous reports.38-40
Viscosity
Viscosity is the property that determines the degree of molecular mobility of a resin composite. Preheating puts the monomers into a state of thermal agitation that increases molecular motion, enhancing fluidity.14,26,29,37 It has been reported that the use of low-viscosity materials results in superior marginal adaptation because of greater fluidity and capacity to promote better contact with the prepared tooth surfaces.14,17 Although some studies have reported decreased microleakage when composites were warmed,16,17 others have shown no significant difference with warming.14,37 Deb and colleagues 14 observed that although marginal adaptation may be better because of the enhanced flowability of preheated resin composites, shrinkage may also be greater, because of higher monomer conversion. They highlighted that increased shrinkage may counteract the improved adaptation achieved by warming composites, leading to no difference in microleakage of composites cured under different temperature conditions.
The third null hypothesis, stating that there is no significant difference in the viscosity of different resin composites under different temperature conditions, was also rejected. Viscosity declined with preheating for all resin composites evaluated in the present study. This result is in agreement with the results of previous investigations, which showed higher fluidity of preheated composites.14,26,29,37 In addition, the extent of flow differed among the resin composites tested. Vit-l-escence resin composite had the lowest viscosity at both room temperature and after preheating.
Conclusions
Within the limitations of this in vitro study, it was determined that preheating resin composites increases their microhardness and flowability. These effects may result in easier placement and greater conversion of monomers.
THE AUTHORS
References
- Cramer NB, Stansbury JW, Bowman CN. Recent advances and developments in composite dental restorative materials. J Dent Res. 2011;9(4)0:402-16.
- Kubo S, Kawasaki A, Hayashi Y. Factors associated with the longevity of resin composite restorations. Dent Mater J. 2011;30(3):374-83.
- Puckett AD, Fitchie JG, Kirk PC, Gamblin J. Direct composite restorative materials. Dent Clin North Am. 2007;51(3):659-75, vii.
- Ilie N, Hickel R. Resin composite restorative materials. Aust Dent J. 2011;56 Suppl 1:59-66.
- Ferracane JL. Current trends in dental composites. Crit Rev Oral Biol Med. 1995;6(4):302-18.
- Lutz F, Krejci I, Barbakow F. Quality and durability of marginal adaptation in bonded composite restorations. Dent Mater. 1991;7(2):107-13.
- Korkmaz Y, Ozel E, Attar N. Effect of flowable composite lining on microleakage and internal voids in Class II composite restorations. J Adhes Dent. 2007;9(2):189-94.
- Roggendorf MJ, Krämer N, Appelt A, Naumann M, Frankenberger R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent. 2011;39(10):643-7.
- Rueggeberg FA, Caughman WF, Curtis JW Jr. Effect of light intensity and exposure duration on cure of resin composite. Oper Dent. 1994;19(1):26-32.
- Carvalho RM, Pereira JC, Yoshiyama M, Pashley DH. A review of polymerization contraction: the influence of stress development versus stress relief. Oper Dent. 1996;21(1):17-24.
- Oliveira KM, Lancellotti AC, Ccahuana-Vásquez RA, Consani S. Shrinkage stress and degree of conversion of a dental composite submitted to different photoactivation protocols. Acta Odontol Latinoam. 2012;25(1):115-22.
- Fabianelli A, Sgarra A, Goracci C, Cantoro A, Pollington S, Ferrari M. Microleakage in class II restorations: open vs closed centripetal build-up technique. Oper Dent. 2010;35(3):308-13.
- Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJ. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent. 2012;40(6):500-5. Epub 2012 Mar 3.
- Deb S, Di Silvio L, Mackler HE, Millar BJ. Pre-warming of dental composites. Dent Mater. 2011;27(3):e51-9.
- Oliveira LC, Duarte S Jr, Araujo CA, Abrahão A. Effect of low-elastic modulus liner and base as stress-absorbing layer in composite resin restorations. Dent Mater. 2010;26(3):e159-69.
- Wagner WC, Aksu MN, Neme AM, Linger JB, Pink FE, Walker S. Effect of pre-heating resin composite on restoration microleakage. Oper Dent. 2008;33(1):72-8.
- dos Santos RE, Lima AF, Soares GP, Ambrosano GM, Marchi GM, Lovadino JR, et al. Effect of preheating resin composite and light-curing units on the microleakage of Class II restorations submitted to thermocycling. Oper Dent. 2011;36(1):60-5.
- Daronch M, Rueggeberg FA, De Goes MF. Monomer conversion of pre-heated composite. J Dent Res. 2005;84(7):663-7.
- Daronch M, Rueggeberg FA, De Goes MF, Giudici R. Polymerization kinetics of pre-heated composite. J Dent Res. 2006;85(1):38-43.
- Eliades GC, Vougiouklakis GJ, Caputo AA. Degree of double bond conversion in light-cured composites. Dent Mater. 1987;3(1):19-25.
- Tarumi H, Imazato S, Ehara A, Kato S, Ebi N, Ebisu S. Post-irradiation polymerization of composites containing bis-GMA and TEGDMA. Dent Mater. 1999;15(4):238-42.
- El-Korashy DI. Post-gel shrinkage strain and degree of conversion of preheated resin composite cured using different regimens. Oper Dent. 2010;35(2):172-9.
- Muñoz CA, Bond PR, Sy-Muñoz J, Tan D, Peterson J. Effect of pre-heating on depth of cure and surface hardness of light-polymerized resin composites. Am J Dent. 2008;21(4):215-22.
- Ausiello P, Cassese A, Miele C, Beguinot F, Garcia-Godoy F, Di Jeso B, et al. Cytotoxicity of dental resin composites: an in vitro evaluation. J Appl Toxicol. 2013(6):451-7. Epub 2011 Nov 26.
- Yan YL, Kim YK, Kim KH, Kwon TY. Changes in degree of conversion and microhardness of dental resin cements. Oper Dent. 2010;35(2):203-10.
- Froes-Salgado NR, Silva LM, Kawano Y, Francci C, Reis A, Loguercio AD. Composite pre-heating: effects on marginal adaptation, degree of conversion and mechanical properties. Dent Mater. 2010;26(9):908-14.
- Ciccone-Nogueira JC, Borsatto MC, de Souza-Zaron WC, Ramos RP, Palma-Dibb RG. Microhardness of composite resins at different depths varying the post-irradiation time. J Appl Oral Sci. 2007;15(4):305-9.
- Tantbirojn D, Chongvisal S, Augustson DG, Versluis A. Hardness and postgel shrinkage of preheated composites. Quintessence Int. 2011;42(3):e51-9.
- Lucey S, Lynch CD, Ray NJ, Burke FM, Hannigan A. Effect of pre-heating on the viscosity and microhardness of a resin composite. J Oral Rehabil. 2010;37(4):278-82.
- Awliya WY. The influence of temperature on the efficacy of polymerization of composite resin. J Contemp Dent Pract. 2007;8(6):9-16.
- Calheiros FC, Kawano Y, Stansbury JW, Braga RR. Influence of radiant exposure on contraction stress, degree of conversion and mechanical properties of resin composites. Dent Mater. 2006;22(9):799-803.
- Calheiros FC, Daronch M, Rueggeberg FA, Braga RR. Degree of conversion and mechanical properties of a BisGMA:TEGDMA composite as a function of the applied radiant exposure. J Biomed Mater Res B Appl Biomater. 2008;84(2):503-9.
- Lohbauer U, Zinelis S, Rahiotis C, Petschelt A, Eliades G. The effect of resin composite pre-heating on monomer conversion and polymerization shrinkage. Dent Mater. 2009;25(4):514-9.
- Dewaele M, Truffier-Boutry D, Devaux J, Leloup G. Volume contraction in photocured dental resins: the shrinkage-conversion relationship revisited. Dent Mater. 2006;22(4):359-65.
- Schneider LF, Consani S, Ogliari F, Correr AB, Sobrinho LC, Sinhoreti MA. Effect of time and polymerization cycle on the degree of conversion of a resin composite. Oper Dent. 2006; 31(4):489-95.
- Cook WD, Beech DR, Tyas MJ. Resin-based restorative materials—a review. Aust Dent J. 1984;29(5):291-5.
- Sabatini C, Blunck U, Denehy G, Munoz C. Effect of preheated composites and flowable liners on Class II gingival margin gap formation. Oper Dent. 2010;35(6):663-71.
- Weinmann W, Thalacker C, Guggenberger R. Siloranes in dental composites. Dent Mater. 2005;21(1):68-74.
- Palin WM, Fleming GJ, Nathwani H, Burke FJ, Randall RC. In vitro cuspal deflection and microleakage of maxillary premolars restored with novel low-shrink dental composites. Dent Mater. 2005;21(4):324-35.
- Ilie N, Hickel R. Silorane-based dental composite: Behavior and abilities. Dent Mater J. 2006;25(3):445-54.