Background: The incidence of dental caries has declined significantly among children, likely because of the widespread use of fluoride toothpaste. However, the effect of using fluoride toothpaste has not recently been investigated among older adults.
Objective: To evaluate the incidence and reversal of caries on coronal and root surfaces in a sample of caries-susceptible, community-dwelling older adults who were using fluoride toothpaste and to examine associations with risk factors for caries.
Methods: Community-dwelling adults 65 years of age or older with more than half (> 14) of their natural teeth were eligible for this study. Coronal and root surfaces were scored with the International Caries Detection and Assessment System (ICDAS) at baseline and at 6, 12, 18 and 24 months. Participants were instructed to brush their teeth twice daily for 2 minutes using fluoride toothpaste. Percent incidence and progression or reversal of carious surfaces was measured (in relation to number of surfaces per participant), and relationships with diet, age, sex, medications and systemic conditions were determined.
Results: Mean coronal caries incidence was 1.8% (standard deviation [SD] 3.0%) for noncavitated carious surfaces and 0.3% (SD 0.8%) for cavitated carious surfaces. Mean root caries incidence was 2.0% (SD 4.1%) for noncavitated carious surfaces and 1.4% (SD 3.2%) for cavitated carious surfaces. Reversal of caries for noncavitated carious surfaces was greater for root surfaces than for coronal surfaces (2.9% [SD 4.4%] vs. 0.5% [SD 1.5%]). Bivariate and multivariate analyses showed that increased incidence of root caries was associated with number of medical conditions and greater age.
Conclusion: Among community-dwelling elderly people using fluoride toothpaste, rates of progression and reversal of coronal and root carious surfaces were low.
The Canadian population is aging, with the proportion of seniors expected to double by the year 20251 and the majority of older adults continuing to live independently within the community. Rates of edentulism have declined in North America,2 and an increasing proportion of elderly people retain some or all of their natural teeth. However, the teeth and dental prostheses of older adults are prone to oral disease, which creates a need for maintenance and possibly replacement.3 The prevalence of caries has decreased markedly among both children and adults, whereas the prevalence of caries among older adults aged 70 years and older remains high.4Older adults are at greater risk for dental caries than younger adults because of age-related salivary changes, poor diet and exposure of root surfaces through gingival recession.
The initiation, progression and reversal of dental caries depend upon the balance between demineralization and remineralization of available tooth surfaces. This balance can be shifted to remineralization with the use of fluoride toothpaste,5 whereas demineralization is more likely with increased frequency of sugar consumption,6 xerostomia secondary to systemic diseases and medication,7 and female.8 Although the relation between caries and its risk factors has been studied in children,9-11 older adults12-19 and older adults residing in long-term care settings,20-21 similar information for independent-living older adults using fluoride toothpaste is limited.22
The aim of this study was to document the incidence of caries and rates of caries reversal on coronal and root surfaces in relation to caries risk factors among community-dwelling older adults using fluoride toothpaste.
Methods
A convenience sample of 100 adults 65 years of age or older living independently in the community and having tooth surfaces at risk for development of carious lesions was identified for this 2-year follow-up study. Eligible participants had more than half of their natural teeth (> 14 teeth, excluding third molars), were susceptible to caries (with between 1 and 6 root caries lesions) and had no contraindications to a dental examination or use of fluoride toothpaste.
Attendees at presentations at 14 community centres in Vancouver and its suburbs were invited to participate in the study. Potential participants underwent an oral examination, and the first 100 satisfying the selection criteria were enrolled in the study. All clinical examinations were performed in a dental operatory at the University of British Columbia faculty of dentistry dental clinic or at community centres (using a portable dental light, portable chair and a compressor for air–water syringe and suction). Those who agreed to participate in the study were reimbursed for their travel expenses up to $25 per appointment (screening, baseline examination, and 6-month, 1-year, 18-month and 2-year examinations).
A dental assistant facilitated the collection of all consent forms and all medical, dental and dietary histories. This person also questioned participants as to what treatment they had received for caries during the study, with the dentist examiner subsequently verifying this treatment information. Although complete medical histories were taken, only the number of medical conditions and the number of prescription medications were used in the current analysis. The Compendium of Pharmaceuticals and Specialties23 was used to identify medications with potential xerostomic effects. Participants were questioned about their typical dietary intake, and the daily frequency of sugar intake was calculated. The dental assistant provided a 15-minute educational program concerning daily mouth care for each participant at baseline and at each subsequent examination. Participants were asked to brush their teeth twice daily (after breakfast and before bed) for 2 minutes using fluoride toothpaste (a smear or 1 g of toothpaste on the bristles of a standard soft-bristled toothbrush [supplied]). Participants were asked to refrain from using any other fluoride-containing products, such as mouth rinses, but otherwise were to follow their usual daily mouth care practices. Each participant was given a daily mouth care reminder card, with written instructions and supporting images, along with a logbook for recording compliance. Participants were also given a 3-month supply of toothpaste at the start of the study. The dental assistant called each participant at 3 months to check compliance with the study regimen. Those complying with use of the fluoride toothpaste had their toothpaste replenished at 3-month intervals for the complete study period, and those who were noncompliant were dismissed from the study.
At baseline, 6 months, 1 year, 18 months and 2 years, the dentist re-examined each participant and scored all tooth surfaces for caries with the International Caries Detection and Assessment System (ICDAS).24 This 6-point caries-scoring system has 4 categories for progressive noncavitated caries and 2 categories for cavitated caries (Table 1), along with categories for sound and restored teeth, which allows for more refined monitoring of caries, especially over the short term. Participants were informed of the presence of any carious lesions, in which case treatment recommendations were provided.
The same experienced dentist examined each participant at baseline (0 months) and every 6 months over the 2-year study. Before every examination, each participant underwent a dental cleaning (rubber cap prophylaxis with pumice) by a dental assistant for removal of soft deposits, to facilitate scoring of all exposed coronal and root surfaces. The dentist examiner was calibrated with the principal investigator (C.C.L.W.) on measuring root and coronal caries using the ICDAS. Calibration involved performance of surface-level assessments on each tooth, after which any discrepancies in scoring were re-examined and discussed to reach consensus.
Each tooth was deemed to consist of 5 coronal surfaces (including the incisal surface) and 4 root surfaces. The examiner used a visual–tactile approach, with mouth mirrors, a no. 5 dental explorer and 2.7× magnification, to diagnose coronal and root caries. This process involved assessment of surface texture (hard, leathery or soft) and determination of the presence and degree of cavitation.25 The examiner's reliability was determined by comparing 2 sets of recordings a week apart for 29 randomly selected individuals within the study. To correct for differences among participants in numbers of teeth and exposed root surfaces, the data were analyzed in terms of percent incidence of reversal (or development) of carious lesions on noncavitated and cavitated surfaces.
To better understand variation in caries among participants, bivariate and multivariate analyses were employed. Because the distribution of specific risk factors was not normally distributed, a nonparametric bivariate statistic was applied.
SPSS version 20.0 software (IBM, Armonk, NY) was used for all analyses. Univariate descriptive statistics were used to assess patterns of caries progression or reversal on coronal and root surfaces. For the inferential bivariate and multivariate statistics, a number of known risk factors for caries, such as frequency of sugar consumption, presence of systemic diseases, use of medication, sex and age, were considered. The joint effect of risk factors for coronal and root caries was examined by means of multiple linear regression models. One of the assumptions in regression modelling is the requirement for independence among the included predictors, and violation of this assumption may lead to inflated values of regression coefficients. To test for independence among the included predictors, collinearity diagnostics were employed. The level of statistical significance for all tests was set at p < 0.05.
The study was approved by the Clinical Research Ethics Board, University of British Columbia (H06-03529).
Results
The community centre presentations were attended by a total of 524 older adults. Of these, 418 underwent an oral examination, and the first 100 satisfying the selection criteria were registered into the study. A total of 67 participants (age range 65–86 years at baseline) completed the 2-year study, of whom 41 (61%) were men and 26 (39%) were women. Of the participants who did not complete the study, 14 had no reason for drop-out, 10 were lost to follow-up, 4 did not like the fluoride toothpaste supplied (noncompliant), 2 underwent complete extractions and were fitted with dentures, 2 died, and 1 was in poor health. Although all participants were advised to see their own dentist for treatment of carious lesions detected, only 8 underwent such treatment during the study, with a total of 12 teeth receiving direct dental restorations.
The dentist examiner's reliability for scoring of carious lesions was 97%, indicating good reliability of the data reported here. Mean progression and reversal of caries on coronal and root surfaces was minimal over the 2-year follow-up period (Table 2), but the data for individual participants varied widely, ranging from a minimum 0% reversal or progression to a maximum of 23% reversal. Mean coronal caries incidence was 1.8% (standard deviation [SD] 3.0%) for noncavitated carious surfaces and 0.3% (SD 0.8%) for cavitated carious surfaces. Mean root caries incidence was 2.0% (SD 4.1%) for noncavitated carious surfaces and 1.4% (SD 3.2%) for cavitated carious surfaces. The reversal of noncavitated carious surfaces was greater for root surfaces than for coronal surfaces (2.9% [SD 4.4%] vs. 0.5% [SD 1.5%]). Mean caries incidence after 2 years was 1% for coronal tooth surfaces that were sound at baseline (Fig. 1); however, mean caries incidence for root surfaces was 4 times higher after 2 years (Fig. 2).
Table 1: International Caries Detection and Assessment System for scoring tooth surfaces24
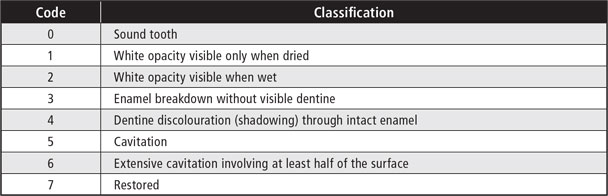
Table 2: Change in caries for coronal and root surfaces among 67 participants over 2-year follow-up period
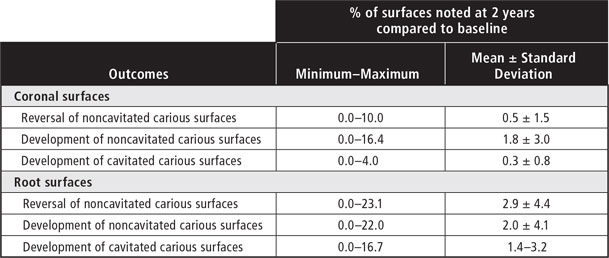
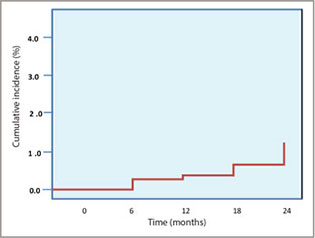 Figure 1: Cumulative incidence of caries on coronal surfaces (over 2-year follow-up period).
Figure 1: Cumulative incidence of caries on coronal surfaces (over 2-year follow-up period).
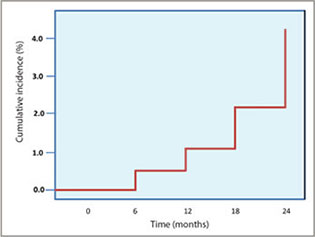 Figure 2: Cumulative incidence of caries on root surfaces (over 2-year follow-up period).
Figure 2: Cumulative incidence of caries on root surfaces (over 2-year follow-up period).
Bivariate and multivariate analyses showed that only the number of systemic medical conditions was associated with development of carious lesions (Table 3). Two linear multiple regression models, one for caries risk on coronal surfaces and the other for caries risk on root surfaces, were employed to assess risk factors of medication use, frequency of sugar intake, number of systemic conditions and age (Table 4). Collinearity diagnostics showed no violation of the assumption of independence among these risk factors (all tolerance values > 0.7; variance inflation factor for all independent predictors combined < 30), and all regression coefficients were therefore considered valid. The multiple linear regression models explained about 16% of the variation in caries incidence (R2 = 0.157). Increased age was associated with higher incidence of root carious lesions.
Table 3: Caries incidence among 67 participants over 2-year follow-up, in relation to caries risk factors
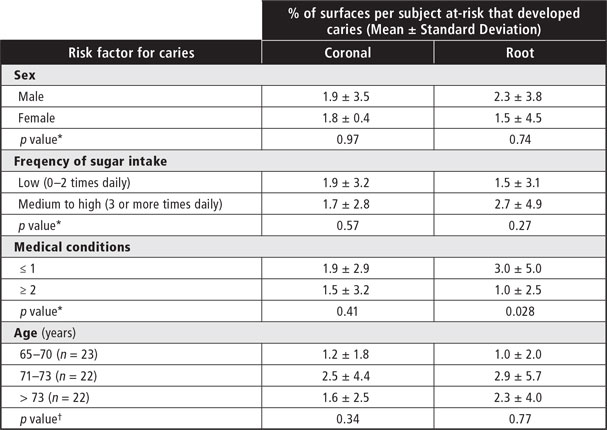
*Mann–Whitney U test.
†Kruskal–Wallis test.
Table 4: Linear multiple regression models of percent caries incidence among 67 participants after 2 years 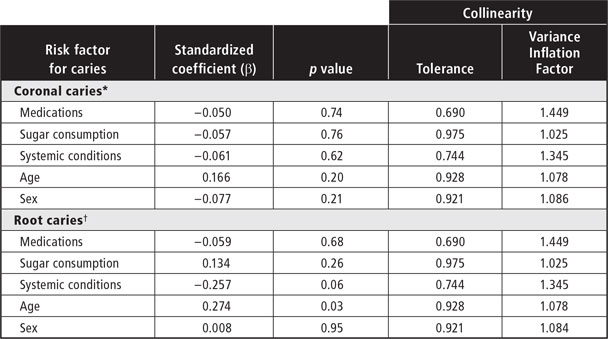
*Adjusted R2 = 0.157; p = 0.062.
†Adjusted R2 = 0.160, p = 0.060.
Discussion
In this study of community-dwelling older adults using fluoride toothpaste, rates of both progression and reversal of carious lesions were low, as has been reported in other studies.22,26,27
One challenge in assessing caries incidence in an older population is the variation in number of retained teeth among older adults. For example, in this study, 2 of the participants each acquired 2 new caries surfaces by the 1-year follow-up; however, one person retained 28 teeth (140 coronal surfaces at risk), whereas the other had only 2 teeth (10 coronal surfaces at risk). If the number of teeth retained is not considered, these 2 participants would be in the same risk category, based on 2 new caries surfaces over 1 year. However, standardizing the data in relation to number of teeth yielded values of 1.4% and 20%, respectively, for these 2 participants, indicating a greater risk level for the person with fewer teeth remaining. Therefore, new caries surfaces were calculated as percentages in relation to total number of surfaces at risk.
In this study, the mean annual caries incidence was less than 1%, similar to previously reported rates for independent-living elderly people.12-19 However, it is important to consider the presence of inter-individual variation as it relates to caries progression or reversal, whereby some participants experienced no caries at all, with others having 20% of surfaces at risk for caries. Variation in caries progression was greater on root surfaces than on coronal surfaces.
No significant risk factors were identified for progression of coronal caries; however, progression of root caries was correlated with age and number of medical conditions. Given that caries progression has been consistently related to previous caries experience,15,16,28,29 a higher rate of caries incidence was expected in this sample of older adults. It has been reported that changes in oral health experienced by elderly people are not the result of age itself, but rather are the consequences of systemic disease, use of medications with xerostomic potential, functional disabilities and cognitive impairment.7,16,18,26,30
The small convenience sample used for this study limited its generalizability, but the study does provide valuable information for community-dwelling older adults with identifiable risk for caries. Using a larger sample size or a longer follow-up period for reassessment (or both) would increase the possibility of identifying significant determinants of caries risk.
Conclusions
Minimal rates of progression or reversal of carious lesions were observed among at-risk community-dwelling older adults who were exposed twice daily to fluoride toothpaste. The incidence of root caries was correlated with age and number of concurrent medical conditions.
THE AUTHORS
References
- A Portrait of Seniors in Canada. Statistics Canada; 2006. Report No.: 89-519-XIE: 2-301.
- Elani HW, Harper S, Allison PJ, Bedos C, Kaufman JS. Socio-economic Inequalities and Oral Health in Canada and the United States. J Dent Res. 2012;91(9):865-70.
- Ettinger RL. Oral health and the aging population. J Am Dent Assoc. 2007;138 Suppl:5S-6S.
- Anusavice KJ. Dental caries: risk assessment and treatment solutions for an elderly population. Compend Contin Educ Dent. 2002;23(10 Suppl):12-20.
- Sonbul H, Merdad K, Birkhed D. The effect of a modified fluoride toothpaste technique on buccal enamel caries in adults with high caries prevalence: a 2-year clinical trial. Community Dent Health. 2011;28(4):292-6.
- Tseveenjav B, Suominen AL, Hausen H, Vehkalahti MM. The role of sugar, xylitol, toothbrushing frequency, and use of fluoride toothpaste in maintenance of adults' dental health: findings from the Finnish National Health 2000 Survey. Eur J Oral Sci. 2011;119(1):40-7.
- Chen X, Clark JJ, Naorungroj S. Length of tooth survival in older adults with complex medical, functional and dental backgrounds. J Am Dent Assoc. 2012;143(6):566-78.
- Ferraro M, Vieira AR. Explaining gender differences in caries: a multifactorial approach to a multifactorial disease. Int J Dent. 2010;2010:649643.
- Ismail AI, Sohn W, Lim S, Willem JM. Predictors of dental caries progression in primary teeth. J Dent Res. 2009;88(3):270-5.
- Kallestal C. Wall S. Socio-economic effect on caries. Incidence data among Swedish 12-14-year-olds. Community Dent Oral Epidemiol. 2002;30(2):108-14.
- Skold UM, Lindvall AM, Rasmusson CG, Birkhed D, Klock B. Caries incidence in adolescents with low caries prevalence after cessation of weekly fluoride rinsing. Acta Odontol Scand. 2001;59(2):69-73.
- Hamasha AA, Warren JJ, Hand JS, Levy SM. Coronal and root caries in the older Iowans: 9- to 11-year incidence. Spec Care Dentist. 2005;25(2):106-10.
- Griffin SO, Griffin PM, Swann JL, Zlobin N. Estimating rates of new root caries in older adults. J Dent Res. 2004;83(8):634-8.
- Thomson WM. Dental caries experience in older people over time: what can the large cohort studies tell us? Br Dent J. 2004;196(2):89-92.
- Hawkins RJ, Jutai DK, Brothwell DJ, Locker D. Three-year coronal caries incidence in older Canadian adults. Caries Res. 1997;31(6):405-10.
- Drake CW, Beck JD, Lawrence HP, Koch GG. Three-year coronal caries incidence and risk factors in North Carolina elderly. Caries Res. 1997;31(1):1-7.
- Locker D. Incidence of root caries in an older Canadian population. Community Dent Oral Epidemiol. 1996;24(6):403-7.
- Lawrence HP, Hunt RJ, Beck JD. Three-year root caries incidence and risk modeling in older adults in North Carolina. J Public Health Dent. 1995;55(2):69-78.
- Hand JS, Hunt RJ, Beck JD. Incidence of coronal and root caries in an older adult population. J Public Health Dent. 1988;48(1):14-9.
- Chalmers JM, Carter KD, Fuss JM, Spencer AJ, Hodge CP. Caries experience in existing and new nursing home residents in Adelaide, Australia. Gerodontology. 2002;19(1):30-40.
- Wyatt C. Elderly Canadians Residing in Long-Term Care Hospitals: Part II. Dental Caries Status. J Can Dent Assoc. 2002;68(6):359-63.
- Jensen ME, Kohout F. The effect of a fluoridated dentifrice on root and coronal caries in an older adult population. J Am Dent Assoc. 1988;117(7):829-32.
- Repchinsky C, editor. Compendium of pharmaceuticals and specialties. Ottawa (ON): Canadian Pharmacists Association; 2008
- Pitts N. "ICDAS"—an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health. 2004;21(3):193-8.
- Lynch E. Antimicrobial management of primary root carious lesions: a review. Gerodontology. 1996;13(2):118-29.
- Davies RM. The rational use of oral care products in the elderly. Clin Oral Investig. 2008;8(1):2-5.
- Heijnsbroek M, Paraskevas S, Van der Weijden GA. Fluoride interventions for root caries: a review. Oral Health Prev Dent. 2007;5(2):145-52.
- Ritter AV, Shugars DA, Bader JD. Root caries risk indicators: a systematic review of risk models. Community Dent Oral Epidemiol. 2010;38(5):383-97.
- Powell LV, Leroux BG, Persson RE, Kiyak HA. Factors associated with caries incidence in an elderly population. Community Dent Oral Epidemiol. 1998;26(3):170-6.
- Scully C, Ettinger RL. The influence of systemic diseases on oral health care in older adults. J Am Dent Assoc. 2007;138 Suppl:7S-14S.



