Abstract
The greater palatine nerve and the greater palatine canal are common sites for maxillary anesthesia during dental and maxillo-facial procedures. The greater palatine nerve is thought to course as a single trunk through the greater palatine canal, branching after its exit from the greater palatine foramen. We describe intra-canalicular branching variations of the greater palatine nerve found in 8 of 20 embalmed dissection specimens. Such variation is previously unreported in the literature. We characterize the variations in branching pattern and discuss the possible implications for clinical practice.
The greater palatine nerve (GPN), which is the continuation of the descending palatine nerve, innervates palatal tissues and the palatal gingiva posterior to the canines after passing through the greater palatine foramen. Anesthetising the GPN (i.e., GPN block) at the greater palatine foramen is common during procedures on the maxillary teeth and palate. The greater palatine canal also provides access for maxillary anesthesia in dental practice.1 Studies have suggested that the greater palatine neurovascular bundle is the most critical structure to be identified during subepithelial connective tissue palatal graft procedures.2 Multiple studies in clinical practice have demonstrated that a GPN block produces the most effective, consistent and prolonged analgesia following palatoplasty in children with cleft palate.3 Although a number of studies have shown anatomical variations in greater palatine foramen location, number and morphology,4,5 studies describing anatomical variations in the GPN within and outside the canal are sparse.
Classically, the GPN is thought to descend through the greater palatine canal as a single trunk accompanied by the descending palatine artery.2 After its exit from the foramen, the nerve splits into numerous branches between the osseous roof of the palate and the mucoperiosteum to supply sensory and secretory fibres to the major part of the mucous membrane of the hard palate and palatal gingivae as far as the premaxillary palatine mucosa. Any anatomical variations in the nerve or its branching may have implications for the surgeons and anesthesiologists working in the area. We describe 4 anatomical variations in the normal branching pattern of the GPN in the canal and discuss the implications for clinical practice.
Methods
Twenty (20) well-embalmed cadaveric hemi-sectioned heads (11 male, 9 female) were dissected for study purposes at the University of Western Ontario's Schulich School of Medicine and Dentistry.* None had anatomical deformities. Sectioning was carried out to ensure intact hard palate mucosa and nasal septum in each specimen. After localization of the greater palatine foramen by blind needle insertion, the greater palatine neurovascular bundle was exposed by making a transverse incision through the full thickness of the palatal mucosa just behind the point of needle entry. An anterior flap of the mucoperiosteum was then raised laterally to the alveolar margin, with the help of a blunt periosteal elevator. Careful blunt dissection of the neurovascular bundle was performed to separate the nerve and vessels from the surrounding connective tissue near the greater palatine foramen. Blunt dissection of the hard palate mucosa was also performed to observe the branching pattern of the GPN as it traveled anteriorly from the molar region toward the mucosa covering the incisive fossa behind the maxillary incisor teeth.
After removal of the bony septum and the lateral wall of the nose using a chisel and hammer, the GPN was successfully traced superiorly within the greater palatine canal and pterygopalatine fossa. The greater palatine artery was identified as a tortuous structure lying anterior to the nerve in the pterygopalatine fossa in 19 specimens and as a single neurovascular bundle behind the maxillary antrum in 1 case. The greater palatine artery was tied with a thread to distinguish it from the greater palatine nerve and its branches. We noted that 8 of the 20 GPN specimens had variations in the branching pattern within the canal. They were photographed and separated into 4 types.
Results
In 12 of the 20 specimens, the GPN exited through the foramen as a single slender trunk that, as it proceeded anteriorly within the mucosal tissue lying medial to the maxillary premolars, divided into 2 or 3 major branches, which divided further into smaller branches (Fig. 1a). These smaller branches finally intermingle with the branches of the nasopalatine nerves within the mucosa.
In the remaining 8 specimens (40%), 5 male and 3 female, the GPN emerged from the foramen as 2 or more trunks. The trunks traveled anteriorly to further divide normally within the mucosa of the hard palate. In all 8 cases, all branches were confined to the greater palatine canal. However, after emerging from the greater palatine foramen, the distribution of these branches did not follow a normal course, but lateral branches traveled more laterally and medial branches traveled more medially, branching anteriorly along their course.
We observed 4 patterns of intra-canalicular branching (Table 1). In 2 specimens (10%), 2 distinct trunks were noted within the canal, both trunks giving rise to 2 slender branches close to the greater palatine foramen. In 4 specimens (20%), the nerve divided into 2 trunks within the canal exiting the foramen as a thick lateral trunk and a slender medial trunk. In 1 specimen, the nerve divided into 3 slender trunks after emerging from the sphenopalatine ganglion (Fig. 1b). In another case, the nerve divided into 2 trunks within the canal, each giving rise to 2 thread-like branches resulting in 4 such branches exiting the greater palatine foramen (Fig. 1c). In the most common variation (4 cases), the nerve exited the greater palatine foramen in the form of a thick lateral trunk and a slender medial trunk (Fig. 1d). Both of these trunks later ramified extensively within the mucosa of the hard palate.
| No. of specimens (male/female) | Branching pattern | Relation to greater palatine artery within the canal |
|---|---|---|
| 2 (1/1) | 2 distinct trunks dividing into 2 slender branches close to the greater palatine foramen | Artery posterior to the nerves in the canal |
| 1 (1/0) | 3 slender trunks exiting the foramen | Artery posterior to the nerves in the canal |
| 1 (0/1) | 4 thread-like branches exiting the greater palatine foramen | Artery posterior to the nerves in the canal |
| 4 (3/1) | A thick lateral trunk and a slender medial trunk | Mainly posterior course of the artery except in 1 case where it lay along the medial nerve trunk after its exit from the greater palatine foramen |
Figure 1: Anatomical variations in the branching of the greater palatine nerve (GPN) in the greater palatine canal.
NOTE: To view the labels for each Figure, please hover your cursor over each image and they will appear.
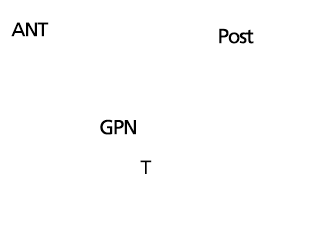
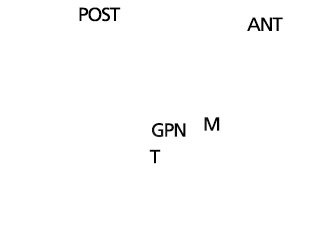
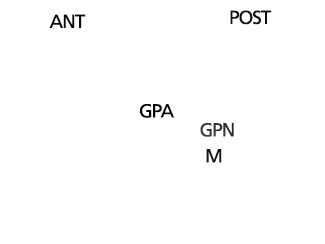
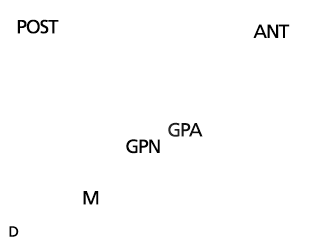
Note: Ant = anterior direction, GPA = greater palatine artery, GPN = greater palatine nerve, M = mucosa of the hard palate, Post = posterior direction, T = tongue.
Unlike the GPN, the greater (descending) palatine artery did not show much variation in its course as it exited the greater palatine foramen. In 6 out of 8 specimens, the vessel ran superior to the nerve and closely adhered to the bony vault of the hard palate. In 1 specimen, the artery exited the foramen lying inferior to the nerve trunks, but then wound around the neurovascular bundle and became superior to the nerves. In the other specimen, the vessel ran parallel to the medial trunk of the nerve.
Discussion
Accurate knowledge of the course and branching pattern of the GPN and artery is extremely important to dental and oro-maxillofacial surgeons and otolaryngologists.6,7 GPN block is a local anesthetic procedure used for multiple maxillary and nasal treatments.8 Block anesthesia of the GPN near the greater palatine foramen is often used in minor oral surgery, periodontics and general dentistry. Furthermore, the mucosa covering the area of the greater palatine foramen is a donor site for soft tissue grafts.2
The location of the greater palatine foramen can vary as noted in several studies,9-11 and 3-dimensional CT studies have been used consistently to locate the foramen.3 However, anatomical variations in the GPN, such as additional branches to molar and premolar teeth, have been reported only sparsely.5 In this study, we observed that in 8 out of 20 specimens (40%), the GPN did not emerge from the greater palatine foramen as a single trunk. In the most frequently observed pattern, the GPN exited the foramen in the form of a thick medial and slender lateral nerve trunk (Fig. 1d). Observations focusing on variation in branching pattern of the GPN within the canal have previously not been reported in the literature; however, our study shows the common occurrence of such variations. This is significant clinically, as the greater palatine canal is frequently used as a route for maxillary nerve blocks during many maxillofacial procedures. The canal and pterygopalatine fossa are also approached in the ligation of the internal maxillary artery or any of its branches to reduce intra-operative bleeding during such surgical procedures as total maxillectomy.12
This study may have further implications in terms of maxillary anesthesia.13 The position of the artery close to the branches might explain the high incidence of epistaxis and intraneural injections14 and should be considered when accessing the greater palatine canal. Multiple branches of the GPN may lie in the path of a needle used to induce maxillary block through the greater palatine canal, thus increasing the possibility of paresthesia and nerve injury. The occurrence of single anatomical variations in the course of the greater palatine artery after its exit from the greater palatine foramen needs further evaluation in a larger sample. Interference in the fusion of the palatine bone with the maxilla during embryonic development, similar to that reported for the mandibular canal,15 could result in variations in the branching of nerves or the course of blood vessels.
The embryologic origin of variations in branching cannot be verified absolutely, and it may only account for high-branching patterns wherein the individual branches form along with the inferior posterior nasal branches. Such variation may also be related to facial biotype, which may affect the location and course of the greater palatine canal and foramen.4 The incidence and possible causes of these anatomical variations require further study. A preliminary ultrasound scan may identify the neurovascular anatomical variations and the location of the greater palatine foramen consistently, thereby increasing the safety of these procedures.12
Anatomical variations in the GPN can also have important implications for dental, maxillofacial surgeons and otolaryngologists performing orthognathic Le Fort I surgeries and sinonasal surgeries.3,16 It has been suggested that patients undergoing Le Fort I osteotomy should be warned of the potential for sensory morbidity, particularly if the planned treatment might necessitate division of the GPN.7,17 Furthermore, during endoscopic surgeries, injury to the GPN can occur if the anatomy of this region is not understood clearly.18
Conclusions
To conclude, anatomical variations in branching of the GPN may occur, with or without associated anatomical variations in the associated blood vessels. Knowledge of such variations may have important implications in terms of improving the safety of surgical procedures performed around the palate, nose and maxilla.
* All cadaveric specimens were obtained with permission from the body bequeathal program at Western University (London, Ontario), in accordance with the Anatomy Act of Ontario and Western's Committee for Cadaveric Use in Research.
THE AUTHORS
References
- Wong JD, Sved AM. Maxillary nerve block anaesthesia via the greater palatine canal: a modified technique and case reports. Aust Dent J. 1991;36(1):15-21.
- Benninger B, Andrews K, Carter W. Clinical measurements of hard palate and implications for subepithelial connective tissue grafts with suggestions for palatal nomenclature. J Oral Maxillofac Surg. 2012;70(1):149-53.
- Jonnavithula N, Durga P, Madduri V, Ramachandran G, Nuvvula R, Srikanth R, et al. Efficacy of palatal block for analgesia following palatoplasty in children with cleft palate. Pediatr Anaesth.2010;20(8):727-33.
- Kang SH, Byun IY, Kim JH, Park HK, Kim MK. Three-dimensional analysis of maxillary anatomic landmarks for greater palatine nerve block anesthesia. J Craniofac Surg. 2012;23(3):e199-e202.
- Ikuta CR, Cardoso CL, Ferreira-Júnior O, Lauris JR, Souza PH, Rubira-Bullen IR. Position of the greater palatine foramen: an anatomical study through cone beam computed tomography images. Surg Radiol Anat. 2013;35(9):837-42.
- Attar BM, Far NF. Neurosensory changes of palatal mucosa following Le Fort I osteotomy. J Res Med Sci. 2009;14(5):269-75.
- Mellema JW, Tami TA. An endoscopic study of the greater palatine nerve. Am J Rhinol. 2004;18(2):99-103.
- Schwartz-Arad D, Dolev E, Williams W. Maxillary nerve block — a new approach using a computer-controlled anesthetic delivery system for maxillary sinus elevation procedure. A prospective study. Quintessence Int. 2004;35(6):477-80.
- Methathrathip D, Apinhasmit W, Chompoopong S, Lertsirithong A, Ariyawatkul T, Sangvichien S. Anatomy of greater palatine foramen and canal and pterygopalatine fossa in Thais: considerations for maxillary nerve block. Surg Radiol Anat. 2005;27(6):511-6. Epub 2005 Oct 15.
- Chrcanovic BR, Custódio AL. Anatomical variation in the position of the greater palatine foramen. J Oral Sci. 2010 Mar;52(1):109-13.
- Du Tolt DF, Nortjé C. The maxillae: integrated and applied anatomy relevant to dentistry. SADJ. 2003;58(8):325-30.
- Wang CP, Yang TL, Ko JY, Lou PJ. Ligation of the internal maxillary artery to reduce intraoperative bleeding during total maxillectomy. Laryngoscope. 2007;117(11): 1978-81.
- Garisto GA, Gaffen AS, Lawrence HP, Tenenbaum HC, Haas DA. Occurrence of paresthesia after dental local anesthetic administration in the United States. J Am Dent Assoc. 2010;141(7):836-44.
- Sved AM, Wong JD, Donkor P, Horan J, Rix L, Curtin J, Vickers R. Complications associated with maxillary nerve block anaesthesia via the greater palatine canal. Aust Dent J. 1992 ;37(5):340-5.
- Chávez-Lomeli ME, Mansilla Lory J, Pompa JA, Kjaer I. The human mandibular canal arises from three separate canals innervating different tooth groups. J Dent Res. 1996;75(8):1540-4.
- Bleier BS, Schlosser RJ. Endoscopic anatomy of the postganglionic pterygopalatine innervation of the posterolateral nasal mucosa. Int Forum Allergy Rhinol. 2011;1(2):113-7.
- Al-Din OF, Coghlan KM, Magennis P. Sensory nerve disturbance following Le Fort I osteotomy. Int J Oral Maxillofac Surg. 1996;25(1):13-9.
- Sharp JF, O'Grady G. Dehiscence of the greater palatine nerve. A risk factor in inferior turbinectomy? Clin Otolaryngol Allied Sci. 1993;18(4):253-6.






