Abstract
Introduction: Many Canadian children are affected by early childhood caries (ECC) and require treatment under general anesthesia. The purpose of this study was to determine the burden of day surgery for children with ECC in Canada.
Methods: Day surgery abstracts for children < 6 years of age with ECC were extracted from the Canadian Institute for Health Information Discharge Abstract Database and National Ambulatory Care Reporting System for 4 years, 2010/11 to 2013/14. All provinces and territories participated except Quebec. Variables considered included sex, age, proportion of immigrants in the neighbourhood, Aboriginal concentration, material deprivation index and rurality. Rates were calculated for the pooled 4-year cohort.
Results: The overall rate of dental surgery to treat ECC was 12.1 per 1000 children 12–59 months of age, accounting for 31.0% of all day surgeries performed on this age group in Canada. Rates of dental surgery for children from neighbourhoods with a high proportion of Aboriginal people were 7.8 times those for children living in areas with a low proportion (84.5 vs. 10.9 per 1000). For children from rural regions of Canada, rates were 3.2 times those of urban dwelling children (31.2 vs. 9.8 per 1000). Children from the least-affluent regions had dental surgery rates 3.7 times higher than those from the most-affluent communities (25.7 vs. 6.9 per 1000). Total hospital-associated costs of treating ECC under general anesthesia averaged $21 184 545 annually.
Conclusion: Dental surgery for ECC is far too common and occurs more often among children from the least-affluent households, rural regions and communities with a high proportion of Aboriginal people. Dental surgery rates can serve as an important population health indicator.
One of the most telling signs of the oral health status of children is the demand for dental surgery to treat severe cases of early childhood caries (ECC). By definition, children under 6 years of age are considered to have ECC if they have experienced any past or current decay involving the primary teeth.1 In some children, ECC may involve only a single tooth; in others, multiple teeth may be affected by caries. The complexity of treatment required to rehabilitate the dentition of those with severe ECC, along with their young age, often warrants the use of general anesthesia.
Rates of dental surgery to treat caries under general anesthesia can serve as an indicator for monitoring and benchmarking population health.2 Dental surgery data can provide information on the volume of surgeries, socioeconomic distribution and regional trends.2,3 Few Canadian data exist to support the enhancement and redirection of existing resources to address the burden of severe ECC. Providing health care decision-makers with such information could inform resource planning and oral health promotion activities.2
Guidelines on the use of general anesthesia for the delivery of dental care exist.4-6 Some of the recognized indications include children who cannot cooperate because of a lack of psychological or emotional maturity or mental, physical or medical disability; those for whom local anesthesia is ineffective because of acute infection, anatomic variations or allergy; those who are extremely uncooperative, fearful, anxious and uncommunicative; those requiring significant surgical procedures; and those requiring immediate comprehensive dental care.4
The purpose of this study was to quantify the human and economic burden of day surgery for ECC, identify populations at higher risk for day surgery to treat caries and raise awareness of the extent of this problem facing Canadian children, the dental profession and the public.
Methods
In the absence of national prevalence data on ECC, day surgery under general anesthesia was selected as a suitable proxy to study severe dental caries in Canadian children. Day surgery abstracts for ECC for fiscal years 2010/11 to 2013/14 were extracted from the Canadian Institute for Health Information (CIHI) Discharge Abstract Database (DAD) and National Ambulatory Care Reporting System (NACRS). All provinces and territories except Quebec participated. Given the potential for small numbers of day surgery operations in remote regions, data were pooled for the 4 fiscal years.
Study population
The cohort was constructed based upon the following criteria.7
- Inclusion criteria: Day surgery records from DAD and NACRS; age < 6 years (for population-based rates, the cohort was restricted to ages 1 to < 5 years); discharge records containing an identified diagnosis of dental caries anywhere in the abstract (International Statistical Classification of Diseases and Related Health Problems, 10th rev, World Health Organization, 1992: diagnostic codes K02 and K04.7) and an identified surgical dental procedure (filling, extraction and/or other [Canadian Classification of Health Interventions codes: 1.FE.57.JA, 1.FF.56, 1.FF.89, 1.FE.89, 1.FE.29, 1.FE.53.JA-RV, 1.FF.59.JA, 1.FD.52, 1.FE.87.JA-H1, 1.FF.53, 1.FF.80 or 1.FF.87]) anywhere in the abstract.
- Exclusion criteria: Potential duplicate discharge records; discharge records containing an identified diagnosis of dental trauma or developmental handicap anywhere in the abstract; and discharge records that could not be assigned valid provincial and regional information based on patient postal code.
Variables
Key analytical variables considered included sex, age, immigrant tercile, Aboriginal concentration, material deprivation index (MDI) and rurality.7
- Immigrant tercile: Postal Code Conversion File version 5J (PCCF+; Statistics Canada, Ottawa, Canada) was used to group discharge records into immigration terciles based on dissemination area, the smallest geographic census unit. The immigrant (foreign-born) terciles were constructed using the following thresholds for immigrant concentration in the dissemination area: high ≥ 51.8%; mid 27.0–51.8%; and low < 27.0%.8 Discharge records that could not be assigned an immigrant tercile were excluded from the immigrant tercile analysis.
- Aboriginal concentration: The term "Aboriginal" refers to people who identified themselves as North American Indian (First Nations), Inuit, Métis and other Aboriginal or as having multiple Aboriginal identities in the 2006 census.9 Aboriginal concentration was assigned using the Aboriginal Geozones File developed at Statistics Canada and grouping discharge records into high and low proportions of Aboriginal people based on dissemination area: high Aboriginal concentration ≥ 32.5%; low Aboriginal concentration < 32.5%. In the 2006 census, there were 22 incompletely enumerated First Nations reserves and settlements, which will lead to under-coverage of the overall Aboriginal population. Discharge records that could not be assigned an Aboriginal concentration were excluded from the Aboriginal concentration analysis.
- Material deprivation index (MDI): The MDI, which was developed and is maintained by the Institut national de santé publique du Québec (INSPQ),10 groups discharge records into MDI quintiles based on dissemination area. In this analysis, the most recent 2006 version was used, and the variable was a composite of 3 indicators: education (ratio of people aged 15 years and older with no high school diploma to the population aged 15 years and older), employment (ratio of people aged 15 years and older who are employed to the population aged 15 years and older) and income (average personal income of the population aged 15 years and older). Discharge records that could not be assigned an MDI were excluded from the MDI analysis.
Location of procedure (hospital or private clinic):
- In some jurisdictions, dental day surgery occurs in private institutions, which then report discharge records to the DAD or NACRS. Day surgeries occurring in private institutions were identified in the following provinces. In Alberta, private institutions apply for the designation "non-hospital surgical facility." These facilities report to NACRS and are identified with a unique identifier. In British Columbia, day surgery operations occurring in private institutions are reported to the DAD by the public facility through which the procedure is contracted. These can be identified using the Special Project Field in the DAD, specifically project number 225. In Saskatchewan, the process is very similar to that in British Columbia, but private institutions are identified with project number 925.
Anesthetic technique:
- The type of anesthetic must be recorded in the DAD and NACRS. In this report, anesthetic group 1 (general, spinal, epidural, neuraxial) was considered general anesthetic.
Methods used to calculate rates of day surgery for ECC
Health region, age and sex: Rates for these variables were calculated by dividing the number of procedures in the pooled 4-year cohort (2010/11 to 2013/14) by the sum of the projected population in each group on July 1 of each year beginning in 2010. The populations are taken from Statistics Canada's CANSIM tables 051-0001 and 109-5325 and are summed, as the procedures are taken over a 4-year period.
Material deprivation index, immigrant tercile, Aboriginal concentration and rurality: Projected populations broken down by these variables are not produced by Statistics Canada. Thus, the most recent available census data (2006) were used as the denominators when calculating these rates. Each of these variables was assigned at the dissemination area level, and dissemination area populations were taken from the full 2006 census dissemination file, with the exception of immigrant tercile. The immigrant tercile denominators were taken from a file associated with the PCCF+ (the quintile of adjusted income per person equivalent (QAIPPE) file within PCCF+).
Methods used to calculate costs of day surgery for ECC
Data on costs of day surgery were only available for the first 2 fiscal years under study (2010/11 and 2011/12).7
Facility-level cost per weighted case was derived based on the Canadian Management Information Systems (MIS) database. Discharge-record-level resource intensity weights were calculated using CIHI's Comprehensive Ambulatory Care Classification System (CACS), which groups discharge records into homogenous resource groups. Discharge-record-level hospital cost estimates were then derived using the following formula: discharge-record-level hospital cost = facility-level cost per weighted case × discharge-record-level resource intensity weight. These results were then aggregated based on the patient's jurisdiction. Discharge records from Nunavut were not included, as Nunavut does not report to the Canadian MIS database. Discharge records that could not be assigned a facility-level cost per weighted case were excluded from the hospital cost analysis.
Results
Figure 1: Percentage of pediatric day surgeries in Canada by type of procedure, 2010/11 to 2013/14.
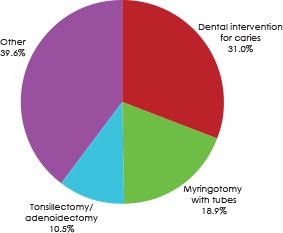
Over the 4-year study period, 57 249 day surgeries to treat severe ECC were performed in Canada (excluding Quebec), accounting for an overall rate of 12.1 per 1000 children aged 12–59 months. Treating ECC under general anesthesia was the most common day surgery in Canada for this age group; it represented 31.0% of all pediatric day surgeries (Fig. 1).
Pooled and annual rates of day surgery for treating severe caries varied by province and territory (Fig. 2). The pooled rate ranged from 8.2 per 1000 children in Ontario to 110.9 per 1000 children in Nunavut. Three provinces (Saskatchewan, Manitoba and Newfoundland and Labrador) and 2 territories (Nunavut and the Northwest Territories) had pooled rates above 25 per 1000 children aged 12–59 months.
When rates of dental surgery by health region in participating provinces and territories are mapped by rate quartile (Fig. 3), they appear to be higher in central and northern regions of Canada. Overall, 31.2% (17 875 of 57 249) of day surgeries occurred among children living in 18 health regions with a rate ≥ 25 per 1000. Health regions in northern Saskatchewan and Manitoba had the highest rates of day surgery. Specifically, the Mamawetan Churchill River Regional Health Authority and the Athabasca Health Authority in Saskatchewan had rates of 135.2 per 1000 and 221.4 per 1000, respectively. The Northern Regional Health Authority in Manitoba had a pooled 4-year rate of 109.3 per 1000.
Figure 2: Rate of day surgery for dental caries among children 1–4 years old, by province or territory.
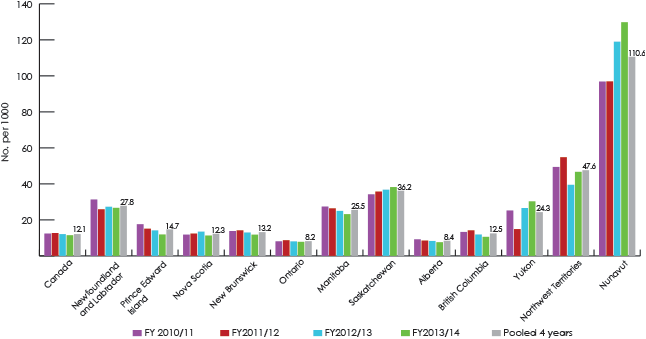
Figure 3: Rate of day surgery for dental caries among children 1–4 years old, by health region, pooled over 4 years, 2010/11–2013/14.

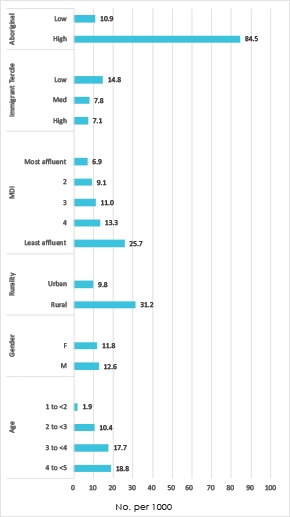
Rates of dental surgery were then calculated for key covariables of interest (Fig. 4). Rates of surgery for children from neighbourhoods with a high proportion of Aboriginal people were 7.8 times greater than for children living in areas with a low proportion (84.5 vs. 10.9 per 1000). Children in rural regions of Canada had rates 3.2 times those of urban-dwelling children (31.2 vs. 9.8 per 1000). There was also an inverse relation between rate of dental surgery and MDI, which is a measure of socioeconomic status based on income, employment and education. Children from the least-affluent regions had dental surgery rates 3.7 times higher than those from the most-affluent communities (25.7 vs. 6.9 per 1000).
Table 1: Hospital cost of day surgery to treat dental caries among children 1–4 years old by province or territory, 2010/11 to 2011/12.
| Province or territory | Cost ($) | ||
|---|---|---|---|
| Average annual | Average/day surgery | Pooled 2-year total |
|
| British Columbia | 3 516 560 | 1515 | 7 033 121 |
| Alberta | 2 281 077 | 1963 | 4 562 155 |
| Saskatchewan | 3 292 791 | 1699 | 6 585 582 |
| Manitoba | 2 767 564 | 1643 | 5 535 127 |
| Ontario | 6 506 893 | 1408 | 13 013 786 |
| New Brunswick | 448 047 | 1271 | 896 094 |
| Nova Scotia | 730 607 | 1657 | 1 461 214 |
| Prince Edward Island | 136 151 | 1441 | 272 302 |
| Newfoundland and Labrador | 971 998 | 1734 | 1 943 996 |
| Yukon | 61 193 | 1912 | 122 386 |
| Northwest Territories | 188 881 | 1379 | 377 761 |
| Nunavut | 282 784 | 1454 | 565 567 |
| Total | 21 184 545 | 1564 | 42 369 090 |
Treating ECC in the operating room has a financial impact on the health care system, on social programs targeted at low-income families, on private dental insurers and on families in terms of out-of-pocket expenditures, time and opportunity costs. However, only hospital-related costs were available (Table 1). The average annual total hospital-associated costs of treating ECC under general anesthesia in Canada (excluding Quebec) were $21 184 545. This translates into an average hospital cost of $1564 per child.
Discussion
This study focused on the treatment of severe ECC among preschool children receiving rehabilitative surgery under general anesthesia. Our results reveal that ECC is the most common reason for day surgery among this age group in Canada. As we studied only 4 years' worth of data (2010/11 to 2013/14), we were unable to determine whether rates of dental surgery are increasing. However, a recent publication from Manitoba suggests that surgery rates there have increased.2 Demand for general anesthesia when treating caries in young children also appears to be increasing in several countries.11-13
The challenge of ECC is that its origins are multifactorial and it is influenced by both biomedical and social determinants of health.14,15 It is apparent from this study that Indigenous children and those from rural and remote regions of Canada are more likely to develop severe ECC that warrants treatment under general anesthesia (Fig. 3). This is not surprising as Indigenous children (American Indian, Alaska Natives, First Nations, Métis and Inuit) have all been identified as being at high risk for developing extensive caries.16-18 Rates of dental surgery in northern Manitoba, where many First Nations communities are situated, have increased significantly over time.2 High rates of dental surgery have also been reported for Alaska Native children.19 The American Academy of Pediatrics and the Canadian Paediatric Society have published a joint position statement on ECC in Indigenous communities, which helps to raise awareness of the oral health challenges facing these children.16,17 Their recommendations include improved access to care and research on the epidemiology, prevention, management and microbiology of ECC in Indigenous children.16,17
Our study also reveals that surgery rates for children living in rural regions are over 3 times those of children in urban centres. A recent Canadian publication also supports these findings.2 Children in rural communities face several issues that influence access to care and their oral health, including lack of water fluoridation, lack of dental professionals in their community and the need to travel outside their community for oral health care.19-21
Figure 4: Rate of pediatric day surgery for dental caries by covariable.
An interesting and somewhat unexpected observation is that surgical rates appear to be somewhat higher in neighbourhoods with relatively few immigrants. Previous studies have reported a higher prevalence of ECC among immigrant groups, but have tended to focus on particular newcomer and refugee communities.22-24 The findings from this study could be explained if, from a pan-Canadian perspective, immigrants had a relatively high socioeconomic status, allowing them to access preventive care. Alternatively, children from immigrant communities may not have been represented in our study cohort as they are less likely to be treated because of challenges accessing and affording dental care.
Our material deprivation variable reveals a clear inverse relation between socioeconomic status and rate of dental surgery, with higher rates among children from the least-affluent neighbourhoods than those from more-affluent areas. Higher rates of general anesthesia during caries treatment have been reported among children from families of low socioeconomic status.12 This is not surprising, as children from disadvantaged households typically have poorer oral health than those from more affluent families and have challenges in affording and accessing regular care.25,26
Treating caries in young children is necessary, as rampant caries can have a negative impact on childhood well-being.18,27,28 Unfortunately, the sobering fact is that there is a high recurrence of caries and relapse among children undergoing surgery.29-33 This might be explained by difficulties parents have in changing and adopting better oral health habits for their child following surgery.34 Further, treating caries has little impact in reducing a child's risk of developing decay in the future, as past caries experience is the greatest predictor of future caries risk.
There is an obvious need for better targeted prevention measures to improve the oral health of vulnerable preschoolers in Canada. Promising methods include promoting the concept of the dental home and the first dental visit by the first birthday.35,36 Children benefitting from early dental care are reported to require less restorative and emergency dental care, more likely to receive preventive dental care and have lower ongoing treatment costs.37-39 Unfortunately, early dental visits are still not common practice in Canada,40,41 although some jurisdictions have developed innovative ways to raise awareness of the first dental visit and improve access to early first dental visits.41-44
Administrative data used in this study were collected and analyzed by CIHI, as their mandate involves the evaluation of information on health and health care in Canada and making such evidence publicly available. CIHI's goal is to provide timely, accurate and comparable information. Data arising from this research have already been shared with provincial and territorial government health departments. The hope is that evidence from this study can increase decision-maker awareness of how a preventable disease like dental caries can place significant strain on families, communities and health care resources.
In this era of limited a nd strained health care financing, analyzing dental surgery rates can be a practical and more economical way to monitor the burden of severe ECC in young children than cross-sectional oral health surveys. Surgery rates for ECC should be adopted as a useful proxy measure of severe dental caries in children. These data can then be used by provincial and territorial governments and health authorities to advocate increased oral health promotion and preventive services directed toward at-risk children. Surgery rates for ECC have been proposed as an outcome to measure the success of population health interventions aimed at improving early childhood oral health.3,21
The costs associated with treating ECC in the operating room are substantial.45 They include hospital-associated costs, dental costs, travel costs and costs borne by the family. In Canada, the hospital-associated costs are absorbed by the universal health care system. Considering that the hospital costs alone for day surgery to treat ECC exceed $21 million annually, dental and pediatric organizations should lobby government for appropriate and sustained funding for research into finding effective prevention strategies for ECC, including addressing parental attitudes and behaviours that place young children at risk for caries. Current research funding devoted to this condition is limited and may be low on the priority lists of health care decision-makers and granting agencies.
This study does have limitations. Because we relied on administrative data related to treating ECC under general anesthesia, we concentrated on the most severe cases. Therefore, this report underestimates the true burden of ECC in Canada, as many children with much milder forms are cared for in the traditional ambulatory clinical setting. Children on waiting lists for ECC-related day surgery were also not captured in these analyses. In addition, we focused on children aged 1 to < 5 years to calculate rates of surgery, as that is a category of Canadian census data for the youngest age groups (< 1, 1 to < 5, and 5 to < 9). We excluded cases among children < 1 year because of the small volume (13 day surgery procedures over 2 years) and those aged 5 to < 6 years (8760), as the census data do not match this category. The frequency of repeat dental surgeries for the children was also not considered in this study.
Some of the day surgery rates for ECC are presented by selected characteristics of neighbourhoods, e.g., the percentage of Aboriginal people or immigrants, rural residents or those considered materially deprived (as measured by the MDI). These rates do not measure characteristics of the individual children who do, or do not, undergo day surgery for ECC, but rather those of the neighbourhoods in which the children reside.
Although the benefits of water fluoridation in preventing caries are well known, information was not available for this report to evaluate the effect of access to fluoridated water systems on dental surgery rates. Children who had disabilities were also excluded, as analyses of day surgeries associated with a diagnosis of a developmental handicap were not possible because of the small numbers.
In summary, dental surgery for ECC is far too common and often occurs among children from less-affluent households, rural regions and communities with a high proportion of Aboriginal people. Rates of dental surgery under general anesthesia to treat caries can serve as an important population health indicator for monitoring, needs assessment and benchmarking purposes.




