Abstract
Objectives:
In most North American jurisdictions, guidelines for use of biologic indicators (BIs) in general dental practice have recommended testing at least weekly. However, in 2011, Alberta mandated a change to daily testing, and other provinces have adopted similar protocols. This study of general dental practices in Alberta assessed factors related to implementation of the changed requirement.
Methods
A survey of 705 randomly selected dental offices queried factors related to implementation of the daily BI testing protocol, including the number of positive test results. We compared findings to analogous data from external laboratory BI tests obtained on a weekly or monthly basis over the preceding 10 years.
Results:
The response rate was a 32.6%. The survey results indicated almost complete compliance with the daily testing requirement and a universal shift to in-office testing. A commensurate 76-fold increase in testing was accompanied by a 15-fold decrease in positive results compared with previous laboratory data. However, although not statistically significant, more offices identified defective sterilizer function through internal testing compared with less-frequent external laboratory testing (5.7% vs 3.2%). The offices reporting positive test results had a significantly higher mean number of repeat positive tests (internal 3.1, SD 1.9 vs. external 1.1, SD 0.11).
Conclusions:
The daily testing requirement was accompanied by a concomitant universal shift from external laboratory to internal office testing. A large decline in the rate of positive testing results was observed, although possibly more offices identified defective sterilizer function.
In general dental practice, sterilizers are monitored during every cycle, with mechanical indicators showing time, temperature and pressure changes and chemical indicators showing changes to process variables. The additional use of biologic indicators (BIs) in such settings has been more variable, despite the fact that they are regarded as the most reliable indication of a successful sterilization cycle. The BI system involves placing viable spores into the sterilizer and culturing them after the sterilization cycle to determine survival. Unlike the guidelines for mechanical and chemical indicators, recommendations regarding frequency of BI use in general dental practices have varied. In Europe, BIs are not routinely used. In North America, most jurisdictions require BI monitoring in general dental practice to be performed at least weekly.1-7 However, if a BI test proves positive, it would be better to have this information as quickly as possible; thus, some organizations recommend daily monitoring.2,6,7 In the past, a practical impediment to daily BI monitoring has been the need to send spore samples to a laboratory by courier. The delay in obtaining results has defeated the purpose of a more timely testing system. However, the development of rapid-readout “in office” BI systems, which can show results within minutes and are as effective as testing by a professional laboratory,8 has provided a regulatory opportunity to recommend or mandate daily BI monitoring.
In 2011, in Alberta, Canada, general dental practices became required to carry out daily BI tests, as part of their infection prevention and control (IPC) protocol.9 Subsequently, other provinces have adopted similar policies. The practical implications of this requirement have been to require general dental practices to set up their own BI testing with the rapid-readout systems. Thus, the earlier arrangement using an external audit of sterilizer efficacy on a weekly or monthly basis by a professional lab has been replaced by a daily internal audit.
The purpose of this study was to provide information regarding this regulatory change by surveying general dental practices in Alberta to confirm the switch to internal biologic monitoring and to determine who is doing the testing and the frequency of positive BI results. These data were compared with test results from an external professional laboratory for the same general dental office population before the regulatory change.
Methods
Survey Instrument and Sample
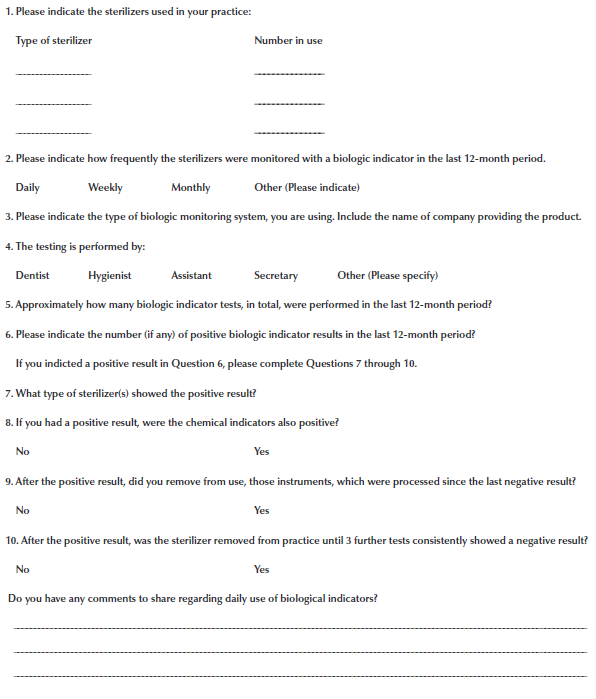
We used a structured single-page survey (Appendix A) to gather data on the implementation and outcomes of daily monitoring in Alberta general dental offices. The survey contained questions about frequency of biological monitoring, type of BI monitoring system, number and types of sterilizers, individuals responsible for the testing, number of BI tests in the previous 12 months, number of positive test results, whether chemical or mechanical indicators concomitantly showed sterilizer failure and follow-up action after a positive test result. The survey also included an unstructured open-comment section.
Before the survey format was finalized, it was reviewed by a focus group of 10 dental offices, who were asked to comment on clarity and any other issues that might interfere with completion of the survey. In addition to some wording suggestions, this group emphasized the need for absolute confidentiality and recommended limiting the length to improve the likelihood of a response.
At the time of the study, there were 1426 registered dental facilities in Alberta. Surveys were distributed by fax to a randomized selection of 705 offices representing approximately 50% of all offices in the province. The cover letter to participants included notification of ethical approval and assurance of anonymity. The returned faxed forms were clipped to remove identifiers before review, and the absence of electronic records ensured complete anonymity.
BI Test Results from External Laboratory
A detailed record of BI test results from the Sterilization Monitoring Service at the dental school at the University of Alberta provided the comparative data. These records were compiled for a 10-year period (2002–2011) directly preceding the introduction of the new guidelines. In total, 59 260 tests were performed. Of these, 52 872 (89.2%) involved steam sterilizers, 4856 (8.2%) involved chemical sterilizers and 1532 (2.6%) involved dry-heat sterilizers. Only results for steam sterilizers were used for comparison with the survey results because the post-2011 regulations mandated the use of steam sterilizers only.
Analytic Methods
Descriptive statistical analysis generated a profile of the results from both the survey and external laboratory records. Differences between internal and external test results were determined using χ2 analysis to reveal proportionate differences and Mann-Whitney tests to compare interval data. Differences were considered significant when P < 0.05.
Ethical Review
The University of Alberta Research Ethics Board reviewed and approved the protocol for this study.
Results
Survey Findings
With 230 of 705 offices returning completed surveys, we obtained a 32.6% response rate (confidence level 95%; confidence interval: 6). In total, testing from 498 sterilizers was reported (mean 2.2 sterilizers/office). All were steam sterilizers in accordance with the new provincial regulations. Further, compliance with the requirement for daily BI monitoring was 98%. The remaining 2% of offices reported weekly or biweekly monitoring.
All offices were using in-office “rapid readout” BI testing kits; 334 individuals were carrying out the tests. Most of the responsible testers were dental assistants (73%), followed by hygienists (17%), “specially designated” individuals (8%) and dentists (2%). The “specifically designated” individuals were identified by the respondents as sterilizer technicians (26%), sterilizer assistants (19%), reprocessing technicians (19%), sterilizer clerks (7%) and sterilizer staff (7%), with the remaining single individuals identified as a registered nurse, an instrument sterilizing specialist, a sterilizer aide, a lab coordinator, a sterilizer person and “not specified.” Collectively, the offices reported 117 115 tests (mean 509.2 tests/office/year). Among these were 40 positive tests in a 1-year period. Thus, the percentage of positive results from total tests was 0.034%.
The reports of 40 positive BI tests were by 13 offices (5.7%). These offices indicated that they had performed 7914 tests, representing a positive test rate of 0.51% in this subgroup. In 2 of the 40 cases, the chemical indicators had concomitantly indicated an unsuccessful sterilization cycle. Of these offices, 3 reported only a single positive result, and the remaining 10 reported 2–6 positive tests. The mean number of repeat positive tests from all 13 offices was 3.1 (standard deviation [SD] 1.9). Identification of the positive tests was by assistants (60%), hygienists (27%) and specially designated individuals (13%).
With respect to office follow up after a positive result, in all cases, the instruments processed after the last negative result were removed from use. In 8 cases, sterilizers were removed from service until 3 negative tests were obtained; in 1 case, the sterilizer was replaced; and in the remaining 4 cases, the sterilizer was returned to service after 1 negative test.
In the open commentary section, 55 comments were submitted. One indicated a strongly positive view of the new policy; the remainder expressed a range of generally negative views. The primary complaint was the cost of the testing (14 comments).
External Laboratory Testing Results
Over the 10-year study period, 59 049 BI tests were performed. A mean of 878 offices/year (SD 149) submitted test samples; thus, the mean number of tests/office annually was 6.7 (SD 0.4). Most (89%) of the tests were performed on steam sterilizers, the remainder on chemical and dry-heat sterilizers.
The rate of positive test results was 0.6% for all tested sterilizers. This included 277 positive tests for steam sterilizers (0.52% failure rate) and 77 positive tests for chemical and dry heat sterilizers (1.20% failure rate).
Among the results from offices using steam sterilizers only, a mean of 24.5 offices (SD 7.9) or about 3.2% of offices recorded positive test results each year. In 95% of positive cases, following communication and review of the result from the lab, a follow-up test was negative. For the remaining offices, the second attempt resulted in resolution of sterilizer failure in 88% of cases. The mean number of positive tests was 1.12 (SD 0.11). The maximum number of repeat tests was 4 on a single occasion during the 10-year period.
Comparison of External and Internal Results
The survey confirmed the almost entire removal of chemical and dry heat sterilizers from use in this jurisdiction.
Compared with data from external testing in the preceding 10-year period, there was a significant 76-fold increase in the number of tests/office annually and a significant 15-fold decrease in the rate of positive test results (internal 0.034% vs. external 0.52%). The percentage of offices reporting positive test results based on the internal daily testing protocol (5.7%) was greater than the percentage of offices with positive results documented from the previous external laboratory testing protocol (3.2%). However, it was not possible to demonstrate whether this difference was significant. In offices with positive test results, there was a significant increase in the number of repeated positive tests after offices switched to internal testing (internal 3.1 tests vs. external 1.1 tests).
Discussion
Although more frequent BI monitoring would appear to be a more stringent sterilization practice, the implications of this policy change have not been evaluated and the benefits or other unanticipated outcomes are unknown. This study provides the first data regarding implementation of a mandatory policy for daily BI monitoring in general dental practices. Comparison with analogous data accumulated through external laboratory testing, which predated implementation of the new policy, revealed both anticipated and unexpected differences.
Our study demonstrated almost universal compliance with the regulations requiring daily BI testing. This finding was not surprising, as dental offices were audited by their regulatory body to evaluate their IPC procedures and to confirm compliance. The shift from an external to an internal BI protocol was predictable because obtaining same-day results with external laboratory testing was not possible and, thus, would defeat the purpose of a daily testing regimen. Also, predictably, the survey showed a 76-fold increase in the number of BI tests/office annually compared with testing before the regulatory change.
The failure rate (positive test rate) reported for internal same-day testing in our study was 0.034%. In comparison, the external test data over the previous 10 years showed a failure rate of 0.6% for all sterilizer types and 0.52% for steam sterilizers only. Our external test data were comparable to those for BI failure rates in other studies: 0.75% to 1.4%.1,5,10,11 Thus, the failure rate for internal daily testing represented an approximately 15-fold decrease from analogous external testing in our study and even greater compared with other studies. It appears that simply increasing the number of tests does not result in a commensurate linear increase in the reported number of positive tests. The reason for this significant drop in the rate of positive test results under the new daily internal testing protocol is uncertain.
A related but separate question was whether more offices were able to identify faults in their sterilizers or sterilizing procedures with the new testing protocol. Examination of this possibility was done by assessing the number of offices that reported positive test results. This analysis showed that more offices might have been able to identify an operating defect in their sterilizer with increased internal testing (5.7%) compared with less frequent external testing (3.2%) although this did not represent a statistically significant difference.
Further data review raised an unexpected concern. Offices with a positive test result subsequently continued to produce follow-up positive results at a significantly higher rate than was documented in the external testing data (3.1 internal positive tests vs. 1.1 external positive tests). It is not clear why this should be the case. Possibly, this was related to the absence of professional follow-up consultation provided by an external testing laboratory. Alternatively, the absence of external oversight may have been associated with a more complacent attitude by office staff. Related to the last consideration, it is also possible that the comparative historical external testing data was obtained from a more motivated group of clinicians, as indicated by the fact that they were doing BI monitoring, before it was mandated. Obviously, these are not mutually exclusive possibilities and, regardless, it remains a concern that, with internal testing, affected offices seem to have a higher rate of continuing sterilization problems.
Our study did not attempt to determine whether the daily BI testing protocol resulted in a decreased incidence of cross-infection ascribed to dental offices. Although this would appear to be an obvious outcome parameter, it is difficult to assess as there is a paucity of data indicating that dental practices are a vector for cross-infection. A 2012 review of all dental-office-related cross-infection studies indicated that the transmission of viruses or bacteria in dental practice was rare,13 a conclusion supported by other reports.13,14 The best documentation has been for hepatitis B cross-infection by infected dental health care workers. A well-documented case report described hepatitis B cross-infection between 2 patients in a dental practice setting although common dental instruments were not used, indicating this was not related to sterilization failure of instruments.15 A further retrospective report suggests 5 possible cases of hepatitis B transmission in a mobile dental clinic, which the authors indicated did not follow adequate IPC precautions.16 Other concerns related to dental office acquired infections, such as infections acquired from contaminated water, which in at least 1 case resulted in death, are not related to sterilization problems.17
Despite only scattered documentation regarding cross-infection in general dental office settings, it is quite clear that there is no room for complacency, as this might be related to underreporting.12 Further, it is evident that dental instruments will be contaminated with oral microbes and represent an obvious risk for cross-infection.18,19 This has resulted in comprehensive discipline-specific IPC guidelines, including sterilizing any reusable dental instrument that has been exposed to the mouth.1,3 These IPC protocols appear to be widely accepted, and studies examining IPC practice in general dental settings primarily have identified concerns regarding IPC compliance or knowledge.5,14,20-22 Thus, the important challenge in outpatient settings appears to be how to best address these identified problems. In this regard, it is important to note that, because sterilizers used in general dental practices go through multiple cycles each day, whether BIs are used on a weekly or a daily basis, these protocols remain, at best, a quality control audit for sterilizer efficacy. Whether the switch from a weekly external audit to a daily internal audit could affect compliance issues is not known, but further study appears warranted.
In summary, our data show excellent compliance with the new regulations. Predictably, the daily testing requirement resulted in a comprehensive shift to internal office testing that, unpredictably, was associated with a 15-fold decrease in the rate at which positive tests were reported. However, although the data were not statistically significant, it is possible that the new daily testing protocol has resulted in more offices identifying defective sterilizer function. An unexpected finding was that when positive internal testing did occur, the office had significantly more positive follow-up tests compared with offices monitored by an external laboratory.
THE AUTHORS
Corresponding author: Diane Kunyk, Faculty of Nursing, University of Alberta, 11405 87 Avenue, Edmonton AB T6G 1C9. E-mail: diane.kunyk@ualberta.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, Centers for Disease Control and Prevention. Guidelines for infection control in dental health-care settings — 2003. MMWR Recomm Rep. 2003;52(RR17):1-61. https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5217a1.htm
- ANSI/AAMI ST79-2017. Comprehensive guide to steam sterilization and sterility assurance in health care facilities. Arlington, Va.: Association for the Advancement of Medical Instrumentation; 2017.
- Summary of infection prevention practices in dental settings: basic expectations for safe care. Atlanta, Ga.: Centers for Disease Control and Prevention; 2016. Available: https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf (accessed 2021 June 23).
- Miller CH, Palenik CJ. Infection control and management of hazardous materials for the dental team. 5th ed. St. Louis, M.: Elsevier Mosby; 2014.
- Rutala WA, Weber DJ, Healthcare Infection Control Practices Advisory Committee. Guideline for disinfection and sterilization in healthcare facilities, 2008. Atlanta, Ga.: Centers for Disease Control and Prevention; 2019. Available: https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf (accessed 2021 June 23).
- AORN Recommended Practices Committee. Recommended practices for sterilization in the perioperative practice setting. AORN J. 2006;83(3):700-3, 705-8, 711-6 passim.
- Z314-18 Canadian medical device reprocessing. Section 16: Sterilization methods. Ottawa: Canadian Standards Association Group; 2018. p. 191-2
- Rutala WA, Jones SM, Weber DJ. Comparison of a rapid readout biological indicator for steam sterilization with four conventional biological indicators and five chemical indicators. Infect Control Hosp Epidemiol. 1996;17(7):423-8.
- Standard of practice: infection prevention and control standards and risk management for dentistry. Edmonton: Alberta Dental Association and College; 2010. Available: https://www.dentalhealthalberta.ca/wp-content/uploads/2019/03/Standard-of-Practice-Infection-Prevention-and-Control.pdf (accessed 2021 June 30).
- Cuny E. The use of a process challenge device in dental office gravity displacement tabletop sterilizers. Am J Infect Control. 2015;43(10):1131-3.
- Goodman RA, Solomon SL. Transmission of infectious diseases in outpatient health care settings. JAMA 1991;265(18):2377-81.
- Laheij AMGA, Kistler JO, Belibasakis GN, Välimaa H, de Soet JJ, European Oral Microbiology Workshop 2011. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4.
- Cleveland JL, Gray SK, Harte JA, Robison VA, Moorman AC, Gooch BF. Transmission of blood-borne pathogens in US dental health care settings: 2016 update. J Am Dent Assoc. 2016;147(9):729-38.
- Henderson HJ, Hopps L, Roy KM. Blood borne virus testing of 2250 patients in an unusual, repeated dental patient notification exercise: challenges faced and lessons learnt. Public Health. 2017;151:74-80.
- Redd JT, Baumbach J, Kohn W, Nainan O, Khristova M, Williams I. Patient-to-patient transmission of hepatitis B virus associated with oral surgery. J Infect Dis. 2007;195(9):1311–4.
- Radcliffe RA, Bixler D, Moorman A, Hogan VA, Greenfield VS, Gaviria DM, et al. Hepatitis B virus transmissions associated with a portable dental clinic, West Virginia, 2009. J Am Dent Assoc. 2013;144(10):1110-8.
- Ricci ML, Fontana S, Pinci F, Fiumana E, Pedna MF, Farolfi P, et al. Pneumonia associated with a dental unit waterline. Lancet. 2012;379(9816): 684.
- Lewis DL, Arens M, Appleton SS, Nakashima K, Ryu J, Boe RK, et al. Cross-contamination potential with dental equipment. Lancet. 1992;340(8830):1252-4.
- Lewis DL, Boe RK. Cross-infection risks associated with current procedures for using high-speed dental handpieces. J Clin Microbiol. 1992;30(2):401-6.
- McCarthy GM, Koval JJ, John MA, MacDonald JK. Infection control practices across Canada: do dentists follow recommendations? J Can Dent Assoc. 1999; 65(9):506-11.
- Cleveland JL, Bonito AJ, Corley TJ, Foster M, Barker L, Gordon Brown G, et al. Advancing infection control in dental care settings: factors associated with dentists’ implementation of guidelines from the Centers for Disease Control and Prevention. J Am Dent Assoc. 2012;143(10):1127-38.
- Eklund K, Marianos D. Providing a safe environment for dental care in an era of infectious diseases. J Am Dent Assoc 2013;144(12):1330-2.
Appendix
Appendix A: Survey of dental offices related to implementation of daily BI testing protocol.