Abstract
Purpose:
Early restorative interventions may have important implications in young patients, and the International Caries Classification and Management System strongly recommends non-surgical strategies in the management of dental caries. We aimed to assess management of interproximal and occlusal caries in children and adolescents (≤18 years of age) by Canadian dentists.
Methods:
An electronic survey was created and sent to members of Canadian provincial regulatory dental bodies. The survey included 11 questions on demographic factors and 3 clinical situations on dental caries management.
Results:
The response rate was 4.6% (n = 702). To treat interproximal carious lesions limited to enamel, 442 dentists (63.0%) reported using surgical caries removal on a permanent molar and 502 dentists (71.5%) did the same for a primary tooth. For occlusal carious lesions, the corresponding numbers were 300 dentists (42.7%) for a permanent molar and 269 (38.3%) for a primary molar. Age, year of graduation and province of practice appear to have a significant impact on the restorative threshold.
Conclusions:
According to the latest evidence-based recommendations for caries management, the presence of cavitated enamel should be the main indication to restore, and non-surgical interventions for non-cavitated lesions confined to enamel should be prioritized. Results show that a good proportion of respondents have a lower restorative threshold, particularly for interproximal lesions.
Dental caries is a multifactorial disease resulting from a poor balance between demineralization and remineralization of tooth structure.1 Studies show that caries remain one of the most common infectious diseases worldwide in the 21st century.2 In Canada, although the incidence of dental caries has decreased significantly in the last 40 years, a quarter of children and more than half of adolescents still have at least one carious tooth.3 Clearly, caries in children and adolescents remains a problem in dental practices worldwide, including Canada.
Caries management is an ever-evolving field of research aimed at improving knowledge in various therapeutic approaches. In the last decade, there has been a paradigm shift from early surgical caries management to more conservative, non-restorative approaches based on the remineralization potential of carious lesions confined to the enamel or even those affecting dentin.4 As a result, new guidelines for the diagnosis and management of interproximal and occlusal caries have been created to help dentists, including the well-known International Caries Classification and Management System.5
For any recommended change in treatment modality that require behaviour modification, it is reasonable to determine whether such recommendations are implemented in practice. Surveys are common tools to assess the practice of health care professions. Several studies6-8 have been conducted to evaluate caries management in adults, many using the same survey to determine at which stage of carious lesion evolution dental practitioners decided on surgical removal of tooth structure. Treatment modalities were evaluated as well. Although there are fewer studies evaluating caries management in children and adolescents, a calibrated survey adapted for the pediatric population was recently used in France and Australia.6,9,10 In 1994, a study of the management of carious lesions on a first permanent molar of 12-year-old adolescents was conducted in Ontario.8
The purpose of our study was to assess management of interproximal and occlusal caries in children and adolescents by Canadian dentists, using a validated survey similar to those used in France and Australia, not only to establish a national baseline, but also to compare our findings with those of other countries. The secondary objective was to assess differences in treatment modalities relative to sociodemographic data.
Materials and Methods
Using REDCap, an online protected server, available in English and French, we adopted a survey developed by Michèle Mullet-Bolla and Sophie Doméjean, lead authors of similar studies conducted in France and Australia; this survey has been validated.10 However, a few questions were adapted to better address demographic factors and newer caries management strategies. The main components, such as figures, photographs and radiographs, were not altered so as to conform as much as possible to the original survey for data comparison.
Recruitment Strategy
We contacted all Canadian provincial dental regulatory authorities and/or associations, asking them to send the survey to their members directly or in a newsletter. Thus, no email lists were sent to the research team. Dental regulatory authorities in Quebec, Ontario, Saskatchewan and Nova Scotia accepted the offer and sent the survey to their members. According to the most recent figures from the Canadian Dental Association (CDA) in 2013, there were 21,109 registered dentists in Canada. When we add up just the organizations that accepted our request, that resulted in 14,574 in 2013. With more recent figures from Quebec in 2016, the extrapolated numbers can reach up to about 15,029 for our sample size. To increase our sample size, the Canadian Dental Association also agreed to share the survey on its Online Advice & Searchable Information Service (Oasis) platform.
Survey Design and Variables
Demographic data, collected in questions 1–8, included participants’ year of birth, gender, year of graduation, university of graduation, province of practice and practice environment, type of practice, level of training post-dentistry and frequency of treating children. Questions 9–11 served the main objective of the study: to determine at what stage of a carious lesion Canadian dentists treat caries by surgical removal of tooth structure in primary and permanent dentition. These questions consisted of clinical scenarios combined with radiographic representations and/or images corresponding to caries lesions 1–6, in the International Caries Detection and Assessment System (ICDAS).11 Collected data included choice of lesions where a restoration with caries removal would first be performed for interproximal and occlusal carious lesions on primary and permanent teeth, preparation techniques and restorative materials. Responses were then analyzed in relation to the various sociodemographic factors.
Statistical Analysis
A sample size of at least 402 respondents was needed, to provide a bilateral confidence interval of 0.1 based on a ratio of 0.5 and using the exact calculation method of Clopper-Pearson. Furthermore, at the provincial or regional level, a sample of 104 dentists by province or region would give a confidence interval of 0.2 based on a ratio of 0.5. Data were saved on the secure REDCap server and exported into Excel 365 (Microsoft, Redmond, Wash., USA). SPSS v. 26 was used for statistical analysis using descriptive statistics with Χ2 tests and logistic regression analyses. The level of statistical significance was set at p < 0.05. The Χ2 test and logistic regression analyses were used to test a relationship between the stages at which participants will first remove dental caries and the independent variables, for both occlusal and proximal lesions. Residual traces and influence analysis were performed to highlight any discrepancies in the data that may need attention, to ensure that no errors were captured when the participant completed the survey. To ensure good data export, a minimum of 15 mock surveys was used in both English and French versions and excluded from analysis.
Ethics Approval
Ethics approval was obtained from the Comité d’éthique de la Recherche en Santé of the Université de Montréal.
Results
A total of 702 dentists completed the survey appropriately, yielding a response rate of approximately 4.6%. Participants ranged in age from 23 to 81 years (mean 49 years; Table 1). To obtain more statistically significant results, we grouped the western provinces (British Columbia, Alberta, Saskatchewan and Manitoba) and the eastern provinces (New Brunswick, Nova Scotia, Prince Edward Island and Newfoundland-Labrador). For university of graduation, participants were collapsed into 4 groups: Quebec, Ontario, other Canada and United States/international. Most participants (56.3%) treated children aged 6–15 years ≥ 5 times a week. Younger children (<6 years old) were treated less frequently: 1–4 times a week.
Restorative Threshold
Various stages of interproximal and occlusal carious lesions were illustrated and described to the participants (Figures 1 and 2). They were then asked to choose the earliest stage at which they would intervene with restorative treatment (Figures 1 and 3). For interproximal lesions, 502 (71.5%) participants would intervene in a lesion confined to the enamel in a primary tooth and 442 (63.0%) would do the same for a permanent tooth. For occlusal lesions, most participants would intervene once a lesion has progressed into the dentin for both a primary tooth (432, 61.5%) and a permanent tooth (399, 56.8%).
Restorative Technique and Material
For interproximal lesions, 383 (54.6%) participants favoured the traditional GV Black class II preparation technique for primary dentition, while 281 (40.0%) preferred a box-slot preparation. In the permanent dentition, 406 (57.8%) participants chose the box-slot preparation, and 212 (30.2%) chose the traditional class II preparation. For occlusal lesions, removal of carious tissue only was the most popular option in both primary (565, 80.5%) and permanent dentition (557, 79.3%).
For interproximal lesions on a primary tooth, dentists preferred to restore with resin-bonded composite (275, 39.2%), amalgam (240, 34.2%) and resin-modified glass-ionomer (75, 10.7%). On a permanent tooth, resin-bonded composite was greatly favoured (584, 83.2%) compared with amalgam (58, 8.3%). For occlusal lesions, resin-bonded composite was again preferred over amalgam for a primary tooth (332, 47.3% vs. 207, 29.5%) and a permanent tooth (590, 84.0% vs. 40, 5.7%).
We found a significant difference in the use of amalgam for primary teeth in Quebec compared with other provinces (p < 0.001). In Quebec, for interproximal caries on a primary tooth, 78.6% (151/192) of responding dentists chose amalgam as a restorative material. In Ontario, only 12.6% (53/422) of dentists chose amalgam, compared with 55.2% (233) who preferred resin-bonded composite. Amalgam was also the first choice for dentists in both eastern and western provinces, but with lower percentages than Quebec, 44.0% (11) and 38.7% (24), respectively.
Caries Detection and Management on an Occlusal Surface
Both photographic and radiographic representations of tooth 85 (Figures 4a and 4b) were presented to participants, who were asked to classify the occlusal lesion (no lesion, confined to enamel, extending into dentin). They were then asked to determine how they would treat it and which material they would use if they were to restore, no matter their treatment choice (Table 2).
Demographic Factors Influencing Restorative Thresholds
We used Χ2 analysis to assess the influence of demographic factors on the restorative thresholds for interproximal and occlusal carious lesions in primary and permanent dentitions. We used multiple logistic regression analyses to assess all factors, but only the statistically significant findings are reported in Table 3. Odds ratios (with 95% confidence intervals) were used to show whether participants were more likely to delay restoration until the lesion had extended into dentin versus treating lesions confined to the enamel.
|
Demographic factor |
No. dentists (%) |
Demographic factor |
No. dentists (%) |
|---|---|---|---|
| Gender | Location of practice | ||
| Male | 372 (53.0) | Quebec | 192 (27.4) |
| Female | 330 (47.0) | Ontario | 422 (60.2) |
| Age group, years | Western provinces | 62 (8.8) | |
| ≤ 35 | 149 (21.2) | Eastern provinces | 25 (3.6) |
| 36–45 | 149 (21.2) | University of graduation | |
| 46–55 | 159 (22.6) | Quebec | 215 (30.7) |
| > 55 | 239 (34.0) | Ontario | 275 (39.2) |
| Missing | 6 (0.9) | Other Canada | 92 (13.1) |
| Year of graduation | USA and international | 119 (17.0) | |
| 1989 and earlier | 239 (34.0) | Practice environment | |
| 1990–1999 | 155 (22.1) | Urban | 542 (77.2) |
| 2000–2009 | 127 (18.1) | Rural or remote | 142 (20.2) |
| 2010 and after | 181 (25.8) | Missing | 18 (2.6) |
|
Assessment |
Response rate, % (no.) |
|---|---|
|
Note: GIC = glass ionomer cement. |
|
| Carious status (n = 702) | |
| No carious lesion | 6.3 (44) |
| Lesion confined to enamel | 46.7 (328) |
| Lesion extending into dentin | 39.3 (276) |
| Uncertain | 7.7 (54) |
| Treatment (n = 699) | |
| None/follow-up | 11.1 (78) |
| Topical fluoride treatment (varnish, gel) | 13.2 (93) |
| Silver diamine fluoride | 10.1 (71) |
| Fissure sealing | 5.4 (38) |
| Prepare and restore carious part(s) only | 44.1 (310) |
| Prepare and restore whole fissures | 15.5 (109) |
| Material used if restoration (n = 670) | |
| Amalgam | 24.2 (170) |
| Composite | 46.4 (326) |
| Conventional GIC | 3.4 (24) |
| Resin modified GIC | 12.7 (89) |
| Combination of GIC and composite | 3.3 (23) |
| Compomer | 4.4 (31) |
| Other | 1.0 (7) |
|
Independent factor |
OR (95% CI) |
p |
|---|---|---|
|
Note: CI = confidence interval, OR = odds ratio. OR > 1 = more likely to treat lesions in dentin, OR < 1 = less likely to treat lesions in dentin. |
||
| Interproximal lesions on a primary tooth | ||
| Province | ||
| East vs. Quebec | 0.238 (0.66–0.858) | 0.028 |
| Age, years | ||
| 36–45 vs. ≤ 35 | 1.907 (1.113–3.267) | 0.019 |
| > 55 vs. ≤ 35 | 2.003 (1.219–3.293) | 0.006 |
| Frequency of treating children aged 6–15 years | ||
| Never vs. ≥ 5 times/week | 10.302 (1.913–55.475) | 0.007 |
| Interproximal lesions on a permanent tooth | ||
| Age, years | ||
| 36–45 vs. ≤ 35 | 0.605 (0.377–0.971) | 0.037 |
| > 55 vs. ≤ 35 | 0.617 (0.388–0.983) | 0.042 |
| Gender | ||
| Female vs. male | 1.842 ((1.306–2.599) | < 0.001 |
| Occlusal lesions on a primary tooth | ||
| University of graduation | ||
| Ontario vs. Quebec | 0.657 (0.449–0.962) | 0.031 |
| Other Canada vs. Quebec | 0.516 (0.311–0.854) | 0.01 |
| International | 0.436 (0.274–0.693) | < 0.001 |
| Province | ||
| Ontario vs. Quebec | 0.608 (0.421–0.878) | 0.008 |
| East vs. Quebec | 0.232 (0.097–0.555) | 0.001 |
| Occlusal lesions on a permanent tooth | ||
| Year of graduation | ||
| 1989 and before vs. after 2010 | 0.610 (0.398–0.936) | 0.024 |
| 1990–1999 vs. after 2010 | 0.572 (0.363–0.901) | 0.016 |
| Frequency of treating children aged 6–15 years | ||
| Rarely vs. ≥ 5 times/week | 2.054 (1.039–4.060) | 0.038 |
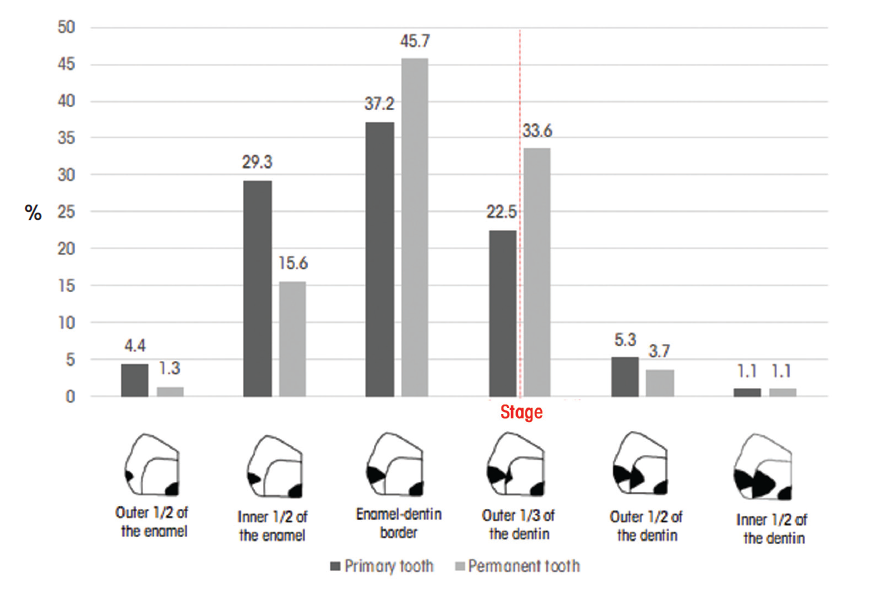
Figure 1: Stage at which participants (%) chose to intervene with restorative treatment of interproximal caries in primary and permanent dentition.
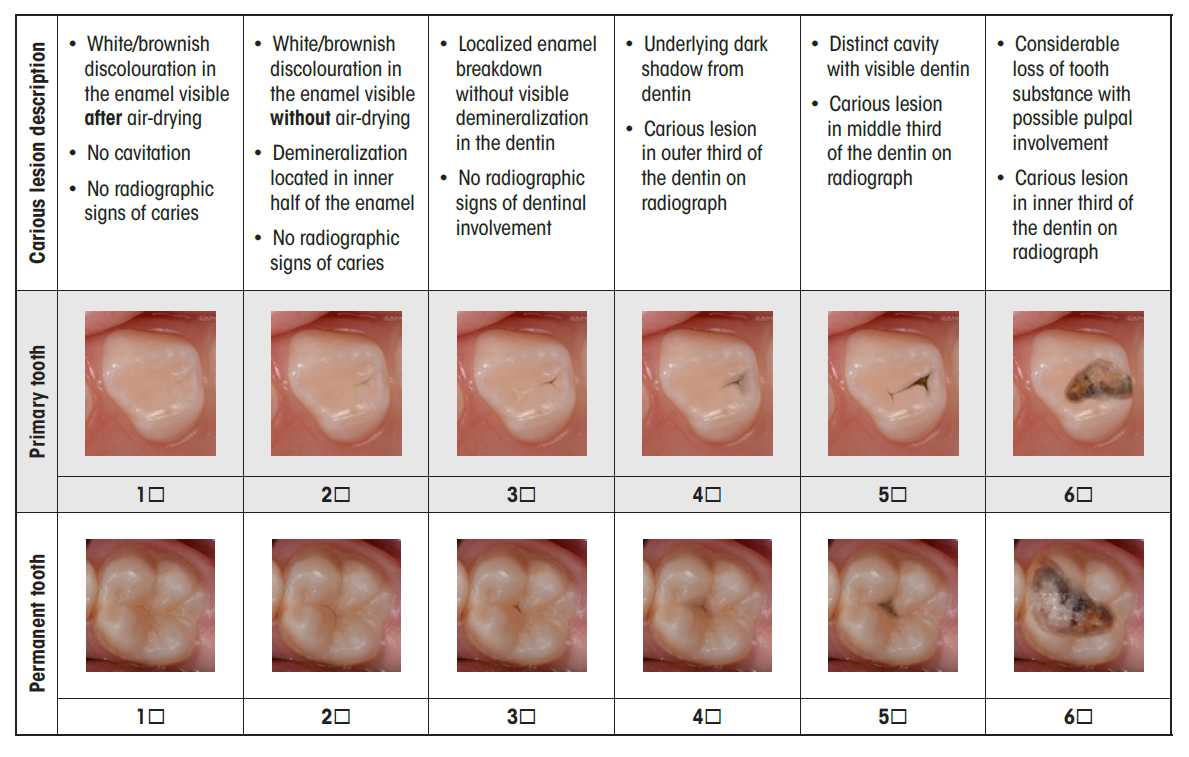
Figure 2: Images and text descriptions provided to participants asked to report their restorative threshold for occlusal caries.
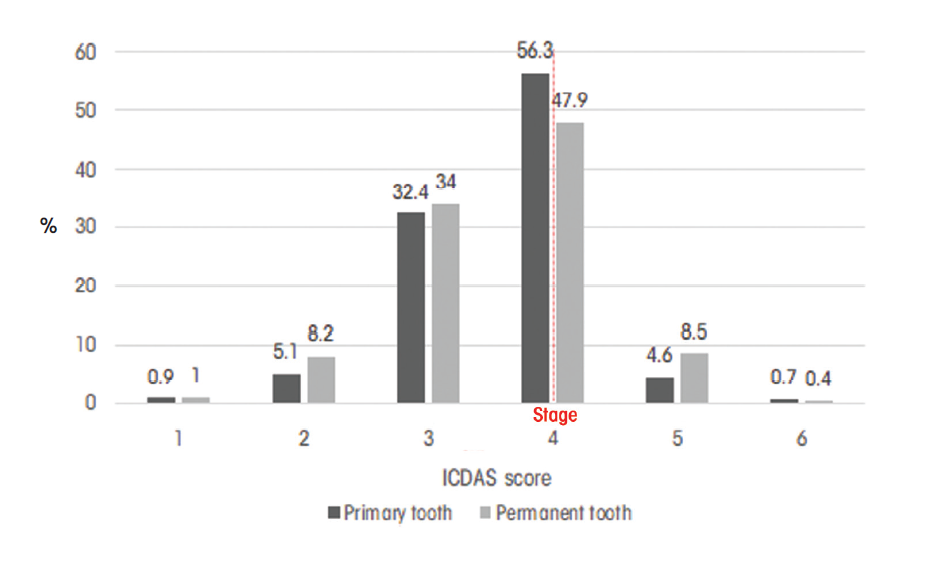
Figure 3: Stage at which participants (%) chose to intervene with restorative treatment of occlusal caries in primary and permanent dentition.

Figure 4a: Photograph of tooth 85. |

Figure 4b: Radiographic image of tooth 85. |
Discussion
The aim of this study was to obtain the first data set in Canada on the management of carious lesions affecting primary and permanent teeth in children and adolescents and to compare data based on social demographic factors. The response rate for this research was low (4.6%) compared with other studies using electronic surveys. For example, a recent study in Australia using the same survey had a response rate of 8%.10 A better response rate might have been obtained by also mailing the survey.9 However, this was not feasible because of limited funding. Men and women were almost equally represented (53.0% vs. 47.0%, respectively) in our study. The response rate was highest among dentists > 55 years of age, closely followed by those in the other age categories in similar proportions (Table 1). A higher response rate from dentists practising in Ontario and Quebec was obtained because only a few other provincial regulatory authorities agreed to send the survey to their members. Furthermore, of the 21 109 dentists practising in Canada in 2013, 8912 were in Ontario and 4720 in Quebec.12
Results of this study show that most dentists tend to treat interproximal carious lesions surgically and restore lesions confined to the enamel: 70.9% for a primary tooth and 62.6% for a permanent tooth. According to the latest recommendations, the presence of cavitated enamel is the main indication to restore.13 Non-cavitated carious lesions can be treated with non-surgical and conservative methods, such as oral hygiene control, pit and fissure sealants and various forms of fluoride.14 For interproximal caries, it is difficult to correlate the presence of radiolucent lesions with the presence of clinical cavitation. A study by Pitts and Rimmers15 showed cavitation in only 40.6% of permanent teeth with a radiolucency extending to the outer half of the dentin. In primary teeth, only 28.3% of teeth had a cavitation with a radiolucency extending to that level. For radiolucencies in the enamel, cavitations were present in 10.6% of permanent teeth and 2.9% of primary teeth.
Participants were more conservative when managing carious lesions on occlusal surfaces than on interproximal surfaces. An indication for surgical treatment of an occlusal carious lesion is the presence of a dentin shadow under the enamel (ICDAS code 4) or the presence of a cavitation (ICDAS codes 5 and 6).5 Most participants first intervened surgically for a lesion with an ICDAS code of 4 (Figure 3). However, many dentists had an aggressive approach and reported surgically treating a molar with no carious dentin involvement: 38.4% on a primary tooth and 43.2% on a permanent tooth.
According to our multiple logistic regression analyses, dentists aged 36–45 years old and those > 55 years old were twice as likely to delay restoration until the lesion had extended into the dentin for interproximal caries on a primary tooth, compared with dentists aged ≤ 35 years. On the other hand, for permanent teeth, dentists 36–45 years old were less likely to delay restoration until the lesion had extended into dentin for interproximal caries than those who were ≤ 35 years old. Some reports in the literature demonstrate that younger dentists are less conservative,8,10 while others show that they are more conservative when treating dental caries.7,16 For interproximal and occlusal lesions, dentists in Quebec were more conservative than dentists in Ontario or eastern provinces.
In terms of university of graduation, dentists from Quebec universities were less aggressive. A recent Canadian study on core cariology curriculum among the 10 accredited Canadian dental schools showed that all schools included teaching of non-surgical methods for treating dental caries. It concluded that harmonization of didactic and clinical teaching was necessary in all dental schools.17 This finding may explain the differences found between the different universities.17,18
Our results highlight the fact that there are barriers to the adoption of new recommendations on non-surgical techniques for dental caries. First, the teaching of caries prevention and restoration has been found to be inconsistent between departments in medical schools. Most clinicians supervising students are part-time employees, and it has been shown19 that they often lack consistency. Problems have occurred with respect to student assessment systems in clinics. Students often receive more points for carrying out a restoration, or they have requirements to fufill.19 Thus, young dentists may continue habits learned in clinical practice at dental school, sometimes in opposition to what they learned didactically.
Other barriers have been identified in private practice. Dentists may be reluctant to accept change, sticking to old dogma. Practices can be overloaded and dentists may find that integration of new approaches takes too much time. Inadequate continuing education or the lack of encouragement to participate in continuing education in cariology may be another barrier. Patients may have certain expectations, lack openness to new therapeutic approaches and fail to comply with new approaches. Finally, barriers can be caused by the health care system or insurance coverage. Most insurance coverage reimburses surgical treatments, but rarely supports prevention or new methods.20
Our results suggest that Canadian dentists choose a surgical approach earlier than Australian dentists. In Keys' 2019 research,10 most respondents (55.5% for permanent dentition and 42.7% for primary dentition) surgically treated an interproximal carious lesion that had reached the internal third of the dentin. For occlusal lesions, Australian dentists were also more conservative: 62% first intervened surgically for an ICDAS code 4 lesion on a primary tooth and 53.8% on a permanent tooth.10 Other studies on permanent teeth also suggest that Canadian dentists are more aggressive in their treatment of dental caries.1,9,16,21 In one study, 60% of Ontarian dentists would have treated an interproximal lesion confined to the enamel of a permanent tooth in a 12 year old. For an occlusal carious lesion, they would do the same 62% of the time. Results are similar to those of our study, revealing that trends have not changed much in 25 years, even though knowledge in cariology has advanced tremendously.8
In our study, choice of techniques and materials varied according to the type of dentition and the province of practice. In primary dentition, the technique of choice was the traditional GV Black class II preparation. In permanent dentition, the more conservative box-slot preparation was favoured. It is encouraging to see that the new recommendations for minimally invasive preparations, such as the box-slot, were respected by most Canadian dentists for permanent teeth. These results are consistent with the widespread use of resin-bonded composites in permanent teeth, which can be placed in more conservative cavity preparations thanks to their bonding properties.22 The advantages of retaining more tooth structure include maintenance of pulp vitality, placement of more durable dental restorations and, ultimately, long-term retention of the tooth in the mouth.14 The more prevalent use of amalgam for primary molars in Quebec compared with Ontario can be explained by the dental coverage program offered by the Quebec government. This program only covers amalgam restorations for posterior teeth in children < 10 years of age. In Ontario, no such restrictions exist. This seems to indicate that despite the availability of more conservative material, Quebec dentists still use amalgam for the most part, given the coverage for their patients.
One limitation of this study is the low participation rate (4.6%), even with a 1-month reminder from the Quebec Order of Dentists to Quebec dentists. Results must be interpreted with caution given the selection bias and the possible low representation of the study population. However, this study provides the first data on the management of interproximal and occlusal caries in primary and permanent dentition in children and adolescents in Canada. A second limitation is the low representation of dentists from western and eastern Canada, with Quebec and Ontario dentists forming the large majority of our sample (87.6%). Another limitation is the fact that survey answers may differ from the actual practices of dentists. To prevent bias, there was no indication of what would be a “good” or “bad” answer in the survey; the questions were neutral and without judgement. The last limitation was the treatment options offered to survey participants. For example, when asked about the management of occlusal caries, choices of fluoride or pit and fissure sealant were available, but not a combination of these. This was deliberate, as we wanted to remain as faithful as possible to the original survey. The only change that was made in the clinical questions was the addition of silver diamine fluoride as a treatment option to reflect contemporary recommendations.23
Conclusion
In summary, Canadian dentists appear to treat interproximal carious lesions more prematurely than recommended by current principles. There is a body of evidence supporting the removal of carious tissue and the placement of a restoration only in the presence of non-cleansable cavitated lesions. However, as only about 10% of interproximal lesions limited to the enamel will present a cavitation,15 it can be concluded that within the limitations of this study, a proportion of Canadian dentists have not integrated the latest evidence-based guidelines, resulting in less conservative practices when compared to other countries, such as Australia.10 Adoption of changes in the management of interproximal caries seems to be slower than that for occlusal caries. This study confirms the presence of barriers to the adoption of new recommendations, in this case, of non-surgical techniques for caries management. Continuing education on conservative, non-surgical interventions is available and should be encouraged by dental regulatory authorities and associations to facilitate diffusion of knowledge.
THE AUTHORS
Corresponding author: Duy-Dat Vu, Faculté de Médecine Dentaire, Université de Montréal, C.P. 6128, succ. Centre-Ville, Montréal, QC H3C 3J7. Email: duy.dat.vu@umontreal.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- Innes NPT, Schwendicke F. Restorative thresholds for carious lesions: systematic review and meta-analysis. J Dent Res. 2017;96(5):501-8.
- Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94(5):650-8.
- The state of oral health in Canada. Ottawa: Canadian Dental Association; 2017. Available: https://www.cda-adc.ca/stateoforalhealth/ (accessed 2021 Dec. 2).
- Innes NPT, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on terminology. Adv Dent Res. 2016;28(2):49-57.
- Pitts NB, Ismail AI, Martignon S, Ekstrand K, Douglas GVA, Longbottom C, et al. ICCMS guide for practitioners and educators. London, UK: ICDAS Foundation; 2014. Available: https://www.iccms-web.com/uploads/asset/59284654c0a6f822230100.pdf (accessed 2021 Dec. 2).
- Doméjean S, Léger S, Maltrait M, Espelid I, Tveit AB, Tubert-Jeannin S. Changes in occlusal caries lesion management in France from 2002 to 2012: a persistent gap between evidence and clinical practice. Caries Res. 2015;49(4):408-16.
- Rechmann P, Doméjean S, Rechmann BM, Kinsel R, Featherstone JDB. Approximal and occlusal carious lesions: restorative treatment decisions by California dentists. J Am Dent Assoc. 2016;147(5):328-38.
- el-Mowafy OM, Lewis DW. Restorative decision making by Ontario dentists. J Can Dent Assoc. 1994;60(4):305-10,13-6.
- Halawany HS, Salama F, Jacob V, Abraham NB, Moharib TNB, Alazmah AS, et al. A survey of pediatric dentists’ caries-related treatment decisions and restorative modalities — a web-based survey. Saudi Dent J. 2017;29(2):66-73.
- Keys T, Burrow MF, Rajan S, Rompre P, Doméjean S, Muller-Bolla M, et al. Carious lesion management in children and adolescents by Australian dentists. Aust Dent J. 2019;64(3):282-92.
- Pitts N. “ICDAS” — an international system for caries detection and assessment being developed to facilitate caries epidemiology, research and appropriate clinical management. Community Dent Health. 2004;21(3):193-8.
- Dentistes autorisés à exercer au Canada en 2013, par province. Ottawa: Canadian Dental Association; 2013. Available: https://www.cda-adc.ca/fr/services/fact_sheets/dentistincanada.asp (accessed 2021 Dec. 2).
- Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007;35(3):170-8.
- Schwendicke F, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res. 2016;28(2):58-67.
- Pitts NB, Rimmer PA. An in vivo comparison of radiographic and directly assessed clinical caries status of posterior approximal surfaces in primary and permanent teeth. Caries Res. 1992;26(2):146-52.
- Chana P, Orlans MC, O’Toole S, Doméjean S, Movahedi S, Banerjee A. Restorative intervention thresholds and treatment decisions of general dental practitioners in London. Br Dent J. 2019;227(8):727-32.
- Tikhonova S, Girard F, Fontana M. Cariology education in Canadian dental schools: where are we? where do we need to go? J Dent Educ. 2018;82(1):39-46.
- Tikhonova S, Jessani A, Girard F, Macdonald ME, De Souza G, Tam L, et al. The Canadian core cariology curriculum: outcomes of a national symposium. J Dent Educ. 2020:84(11):1245-53.
- Fontana M, Zero D. Bridging the gap in caries management between research and practice through education: the Indiana University experience. J Dent Educ. 2007;71(5):579-91.
- McGlone P, Watt R, Sheiham A. Evidence-based dentistry: an overview of the challenges in changing professional practice. Br Dent J. 2001;190(12):636-9.
- Espelid I, Tveit AB, Mejàre I, Sundberg H, Hallonsten AL. Restorative treatment decisions on occlusal caries in Scandinavia. Acta Odontol Scand. 2001;59(1):21-7.
- The reference manual of pediatric dentistry: definitions, oral health policies, recommendations, endorsements, resources. Chicago: American Academy of Pediatric Dentistry; 2019.
- Slayton RL, Urquhart O, Araujo MWB, Fontana M, Guzmán-Armstrong S, Nascimento MM, et al. Evidence-based clinical practice guideline on nonrestorative treatments for carious lesions: a report from the American Dental Association. J Am Dent Assoc. 2018;149(10):837-49.e19.





