Abstract
Objective:
Various teething remedies have been widely marketed to caregivers. Unsafe remedies, including teething necklaces and topical anesthetics, have been implicated in adverse events, such as suffocation injuries and death. However, little is known about the extent of their use. Our primary objective was to assess the prevalence of teething remedy use among caregivers. A secondary objective was to determine whether the use of unsafe teething remedies is related to socioeconomic status (SES) or maternal education.
Methods:
Children aged 12–18 months visiting primary care providers for routine checkups were included. Children outside that age group and those with chronic medical conditions were excluded. Caregivers completed a questionnaire about their children’s teething symptoms and remedies used to relieve them. Unsafe remedies were defined on the basis of American Academy of Pediatrics and Canadian Paediatric Society recommendations and included topical anesthetics, teething necklaces and liquid-filled teething rings.
Results:
Of the 130 questionnaires, 123 were complete and included in statistical analysis: 98% of families used teething remedies and 67% were unsafe. Of these families, 27% used amber teething necklaces; 28% used more than 1 unsafe remedy. Apart from topical anesthetic use, no significant correlations were found between overall unsafe remedy use and SES or maternal education.
Conclusion:
Unsafe teething remedies are commonly used despite recommendations against them. Use of unsafe teething remedies transcends SES and education level.
For most infants, the eruption of 20 deciduous teeth occurs between 6 and 30 months of age.1 Teething is commonly associated with many symptoms, such as diarrhea, irritability, rash and rhinorrhea. Currently, most teething symptoms reported in the literature are based on caregivers’ opinions, which are subject to reporter bias.2 However, studies have identified the following as commonly reported teething symptoms: mild fever (< 38.9°C), irritability, loss of appetite, sleep disturbance, local gingival irritation, increased drooling and gum rubbing.3-5
Various remedies are available to caregivers for relieving perceived teething symptoms in infants and toddlers. Some, such as teething necklaces made of amber or hazelwood, are unsafe, yet are widely marketed. Producers of such necklaces claim that they have pain relieving properties.6,7 Teething necklaces pose a safety concern, as they have been implicated in suffocation accidents and even death.8-10 Recent evidence shows that such necklaces are mechanically unsafe for infants and toddlers.11 A 1-time survey conducted through the Canadian Paediatric Surveillance Program (CPSP) showed evidence of adverse events occurring secondary to the use of teething necklaces in Canada.12 Other teething remedies that have been implicated in safety concerns include topical anesthetics that continue to be marketed to relief teething pain. Topical anesthetics can cause methemoglobinemia, which is a serious condition in which the blood’s oxygen-carrying capacity is compromised.13,14 Although solid teething rings can provide symptom relief, liquid-filled rings can break and leaking liquid can become a choking hazard.15 The Canadian Paediatric Society (CPS) and the American Academy of Pediatrics (AAP) share similar concerns and recommend refraining from using unsafe teething remedies, such as teething necklaces, topical anesthetics and liquid-filled teething rings.16-20
The primary aim of this study was to determine the prevalence of use of unsafe teething remedies and factors that may determine caregivers’ choices in this regard. A secondary aim was to identify any correlation between caregivers’ choice of teething remedy and socioeconomic factors, as various child health outcomes are closely correlated with maternal education and socioeconomic status (SES).21,22
Methods
Design and Participants
This was a population-based survey to capture the prevalence of various safe and unsafe teething remedies. Primary care providers (family physicians and community pediatricians) with affiliations to Western University, London, Ontario, Canada, were approached to participate in the study. Questionnaires were administered to caregivers of children visiting these providers for a well-baby check. Safe teething remedies were defined based on the recommendations of CPS and AAP and included teething toys, cold teething rings, frozen fruit and medications (such as acetaminophen and ibuprofen). Unsafe teething remedies included teething necklaces, topical anesthetics and liquid-filled teething rings.16-19
Inclusion criteria were children aged 12–18 months. Most children achieve tooth eruption by 12 months of age and selecting this as a starting age of inclusion would ensure capturing infants with teeth. On the other hand, children > 18 months likely have achieved tooth eruption many months prior and excluding them would minimize symptom recall bias. Exclusion criteria were children aged < 12 months or > 18 months, children with a chronic medical condition (any condition specified by a diagnostic code other than well-baby check at the office visit) and caregivers who previously completed the survey. We aimed for a sample size of at least 100 caregivers based on a medium effect size (R2 = 0.25), population correlation coefficient = 0.20, alpha = 0.05, power = 0.90 and a drop-out rate = 10%.
Protocol and Instrument
The recruitment phase took place over 12 months between February 2016 and February 2017. Caregivers were recruited by office assistants at each of the participating medical offices. They provided paper questionnaires to eligible caregivers who completed them in the waiting room before seeing the primary care provider. The questionnaire was developed de novo based on a literature review and included 14 questions. There were 5 demographic questions regarding age, age at first tooth eruption and current number of teeth visible. Caregivers were also asked to rate the following teething symptoms in terms of nonexistent, mild, moderate or severe: increased fussiness, fever, anorexia, decreased sleep, inflamed gums, increasing drooling, chewing or biting. Given the lack of validated teething symptom questionnaires in the published literature, these symptoms were selected based on previous teething symptom studies.3-5
Caregivers were then asked to identify the teething remedies they used and to state whether they found these remedies not helpful, somewhat helpful or greatly helpful in relieving teething symptoms. Caregivers were also asked if they had visited their primary care provider because of their child’s teething symptoms. Families also selected an annual income range from the following 4 categories: < $25 000, $25 000–$49 999a, $50 000–$100 000 and > $100 000. For maternal education, families were asked to choose some high school, graduated high school, secondary education or postsecondary education.
Statistical Analysis
Caregivers’ responses were summarized as percentages and descriptive statistics (mean, standard deviation [SD]). Two-tailed Pearson correlations and multiple regression analyses were conducted to examine total number of moderate and severe teething symptoms and caregivers’ use of both safe and unsafe teething remedies. Two-tailed Spearman’s rho tests were conducted to examine correlations between SES and teething remedies. Mann-Whitney U tests were used to examine differences in SES between caregivers who did and did not use teething necklaces. Data were analyzed using SPSS v. 24, and p values < 0.05 were considered statistically significant.
Ethics Approval
Approval for conduct of this survey was obtained from Western University’s Health Sciences Research Ethics Board (REB ID #107614).
Results
Four primary care settings (3 community pediatricians’ offices and 1 office shared by a community pediatrician and a family physician) participated in the study. A total of 130 questionnaires were completed in these 4 settings; 7 were excluded because of missing data, resulting in 123 surveys suitable for analysis. The mean age of infants in the study was 14.47 (SD 2.56) months. Their mean age at first tooth eruption was 6.92 (SD 2.00) months. At the time of the study, the infants and toddlers had a mean total of 8.43 (SD 4.00) teeth.
The most common teething symptom was a moderately increased interest in chewing, with over 50% of caregivers reporting it (Figure 1). Overall, 98% of caregivers used a teething remedy, and over half of the participating caregivers reported the use of an unsafe teething remedy (Figure 2). Of these, liquid-containing teething rings were used most (> 45% of caregivers). Teething necklaces came second, with 27% of caregivers reporting use of amber teething necklaces. Over 20% of caregivers used a topical anesthetic, and 28% used more than 1 unsafe remedy.
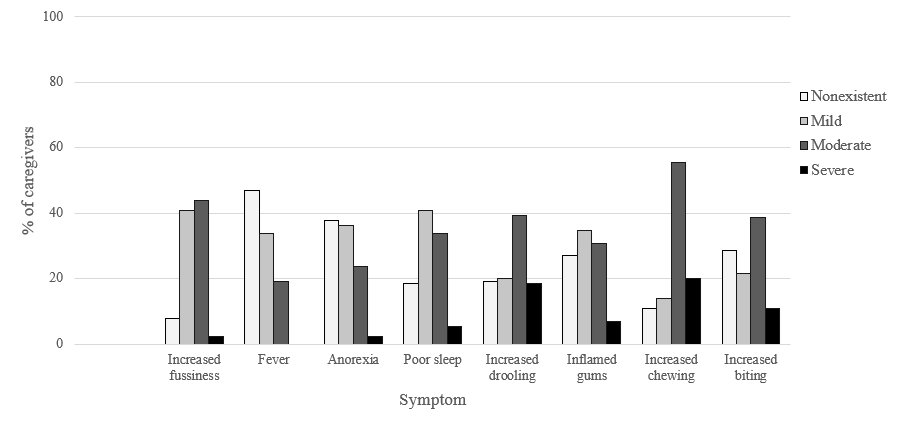
Figure 1: Caregivers’ rating of their infants’ and toddlers’ teething symptoms.
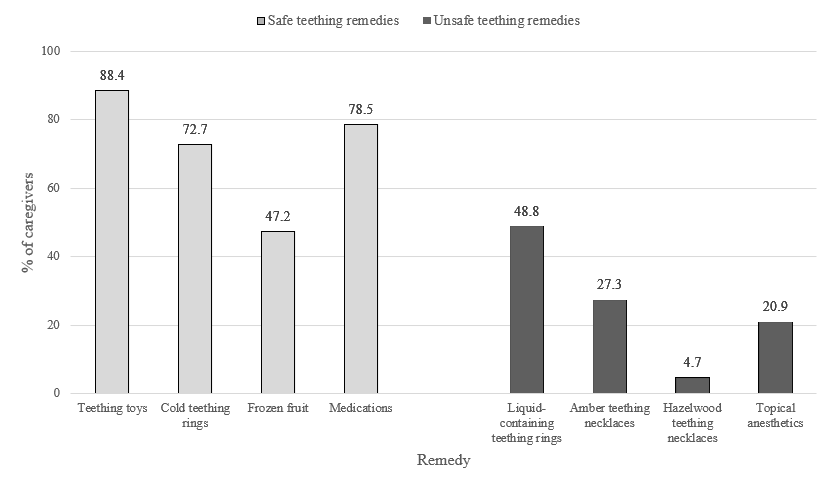
Figure 2: Use of various teething remedies reported by caregivers.
There was a significant relation between number of reported moderate and severe teething symptoms and (a) overall use of teething remedies (r = 0.42, p < 0.001), (b) use of safe teething remedies (r = 0.43, p < 0.001) and (c) use of unsafe teething remedies (r = 0.26, p = 0.004). To further examine these relations, we conducted a multiple regression analysis with number of reported moderate and severe teething symptoms as the outcome and use of safe and unsafe teething remedies included as predictors. Use of safe teething remedies remained significant (p < 0.001), but use of unsafe teething remedies was no longer significant (p = 0.343). Thus, with greater perceived teething symptoms, caregivers were more likely to use teething remedies, with the likelihood of using safe remedies greater than unsafe ones. Only 4% of caregivers visited their primary care provider because of their child’s teething symptoms.
Among the survey population, 14.6% fell into the < $25 000 annual income category, 26.9% in the $25 000–$49 999 category, 29.2% in $50 000–$100 000 category and 25.4% in the > $100 000 category. In this survey, median maternal education was postsecondary education. We did not find a significant correlation between overall unsafe remedy use and SES (Table 1) or maternal education (Table 2). However, a significant negative correlation was identified between SES and the use of topical anesthetics alone (Spearman’s rho = −0.23, p = 0.011). We did not find a difference in SES among families who used teething necklaces compared with those who did not (p ≥ 0.849).
|
Annual income, $ |
No. safe remedies, median (IQR) |
No. unsafe remedies, median (IQR) |
|---|---|---|
|
Note: IQR = interquartile range. |
||
| < 25 000 | 3 (1, 4) | 1 (0, 2) |
| 25 000–49 999 | 3 (2, 4) | 1 (0, 1.25) |
| 50 000–100 000 | 4 (2, 4) | 1 (0, 2) |
| > 100 000 | 3 (3, 4) | 1 (0, 2) |
|
Maternal education level |
No. safe remedies, median (IQR) |
No. unsafe remedies, median (IQR) |
|---|---|---|
|
Note: IQR = interquartile range. |
||
| Some high school | 3 (0.75, 3.25) | 1 (0.75, 2) |
| Completed high school/secondary education | 3 (2.25, 4) | 1 (0, 2) |
| Postsecondary education | 3 (2, 4) | 1 (0, 2) |
Discussion
In infants and toddlers, identifying and characterizing teething symptoms remains challenging given their inability to communicate verbally. The onus is on the caregiver to identify teething-related symptoms, their severity and potential teething remedies. As evident from this study, caregivers who identified their child’s symptoms as moderate to severe were likely to try a teething remedy. Unfortunately, only a small number of caregivers sought their primary care provider’s advice on how to manage teething symptoms, leading to their potential use of hazardous remedies. The use of unsafe teething remedies transcended SES and education level, with the exception that topical anesthetic use was negatively correlated with SES.
Over recent years, teething necklaces have been popularized and widely used. Ours is the first study to examine the prevalence of teething necklace use. About a quarter (27%) of caregivers who visited 1 of the 4 clinics we surveyed used amber teething necklaces; this is an alarming number given the risk associated with them. A nation-wide CPSP survey identified 10 cases of adverse events (some requiring hospitalization) related to teething necklaces and bracelets in a 12-month period.12 Since that survey, the authors have been working with the CPSP to advocate regulation of the use of teething necklaces in young children. Another popular and potentially unsafe remedy identified in our study was liquid-filled teething rings. Although, to our knowledge, there are no published cases, these teething rings carry a theoretical risk of breakage leading to choking or causing frostbite (if frozen).
Limitations of this study include sample selection, which reflects only families who visited the 4 pediatrician offices. Larger-scale studies targeting families with infants and toddlers are needed to determine the true population prevalence of use of unsafe teething remedies. In addition, it remains unclear what influences caregivers’ decisions in choosing a teething remedy. Future research should explore the role of cultural backgrounds and personal beliefs as potential factors impacting caregivers’ use of a teething remedy. After data collection, an error was identified in the survey question about maternal education level: high school education was entered as 2 options (completed high school and secondary education). For statistical analysis, the 2 categories were combined.
Teething pain and symptoms are common in infants and toddlers, leading to caregivers using various remedies to treat the symptoms. Over the last few years, research evidence and case reports have raised safety concerns about products, such as teething necklaces and topical anesthetics. The findings of this survey further support the need for a new approach to parental education about the dangers of some teething remedies; for instance, primary care providers can inform caregivers about these dangers during routine child wellness assessments. In addition, social media have proven to be a powerful tool in educating caregivers, and they can be used as a platform to reach caregivers in terms of providing education about safe teething remedies.23
THE AUTHORS
Corresponding author: Dr. Farah Abdulsatar, 800 Commissioners Rd E, London ON N6A 5W9. Email: farah.abdulsatar@lhsc.on.ca
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose
Acknowledgements: We extend our gratitude to the physicians and staff of South London Children’s Clinic, Springbank Pediatric Services, Rouhani Medical and Masonville Pediatric Clinic for their support.
Funding: This project was funded by the Department of Pediatrics at Western University through a Pediatric Resident Research Grant.
The authors have no declared financial interests in any company manufacturing the types of products mentioned in this article.
This article has been peer reviewed.
References
- Markman L. Teething: facts and fiction. Pediatr Rev. 2009;30(8):e59-64.
- Ashley MP. It’s only teething... a report of the myths and modern approaches to teething. Br Dent J. 2001;191(1):4-8.
- Wake M, Hesketh K. Teething symptoms: cross sectional survey of five groups of child health professionals. BMJ. 2002;325(7368):814.
- Feldens CA, Faraco IMJ, Ottoni AB, Feldens EG, Vítolo MR. Teething symptoms in the first year of life and associated factors: a cohort study. J Clin Pediatr Dent. 2010;34(3):201-6.
- Massignan C, Cardoso M, Porporatti AL, Aydinoz S, Canto GDL, Mezzomo LAM, et al. Signs and symptoms of primary tooth eruption: a meta-analysis. Pediatrics. 2016;137(3):e20153501.
- Hazelaid. All about Hazelwood. Chateauguay, Que.: Hazelaid; 2021 Available: https://hazelaid.com/pages/about-hazelwood (accessed 2021 Oct. 4).
- Baltic amber necklaces for children. Vilniaus, Lithuania: Amber Artisans; 2021. Available: https://www.amberartisans.com/amtene4.html (accessed 2021 Oct. 4).
- Cox C, Petrie N, Hurley KF. Infant strangulation from an amber teething necklace. CJEM. 2017;19(5):400-3.
- Slater M. 'My stomach just dropped with a sickening feeling': mother’s panic at finding her little girl nearly strangled by teething necklace... as officials warn the popular devices are potentially deadly. Daily Mail Australia. 2015;1 Mar. Available: https://www.dailymail.co.uk/news/article-2974043/Mother-s-panic-finding-little-girl-nearly-strangled-teething-necklace-officials-warn-popular-devices-potentially-deadly.html (accessed 2020 Oct. 27).
- Graham RF. Toddler boy dies after ‘choking’ on a necklace during nap time at daycare center that's now under investigation. Daily Mail. 2016;14 Oct. Available: https://www.dailymail.co.uk/news/article-3832605/Toddler-boy-dies-choking-necklace-nap-time-daycare-center-s-investigation.html (accessed 2020 Oct. 27).
- Soudek L, McLaughlin R. Fad over fatality? The hazards of amber teething necklaces. Paediatr Child Health. 2018;23(2):106-10.
- Abdulsatar F, Matsui D, Miller M, Taheri S. Teething necklaces and bracelets pose significant danger to infants and toddlers. Paediatr Child Health. 2019;24(2):132-3.
- Hofer KE, Kaegi S, Weiler S. The acute toxicity profile of a teething gel containing salicylamide in toddlers: an observational poisons centre-based study. Clin Toxicol (Phila). 2019;57(3):220-1.
- Teoh L, Moses GM. Are teething gels safe or even necessary for our children? A review of the safety, efficacy and use of topical lidocaine teething gels. J Paediatr Child Health. 2020;56(4):502-5.
- Healthwise Staff. Teething products. Victoria, British Columbia: HealthLink BC; 2019. Available: https://www.healthlinkbc.ca/pregnancy-parenting/parenting-babies-0-12-months/baby-health/teething-products (accessed 2021 Oct. 4).
- Swanwon WS. How to help teething symptoms without medications. Itasca, Ill.: American Academy of Pediatrics; 2014. Available: https://www.healthychildren.org/English/ages-stages/baby/teething-tooth-care/Pages/How-to-Help-Teething-Symptoms-without-Medications.aspx (accessed 2021 Oct. 4).
- Baby teething pain. Itasca, Ill.: American Academy of Pediatrics; 2018. Available: https://www.healthychildren.org/English/ages-stages/baby/teething-tooth-care/Pages/Teething-Pain.aspx (accessed 2021 Oct. 4).
- Teething necklaces and beads: a caution for parents. Itasca, Ill.: American Academy of Pediatrics; 2018. Available: https://www.healthychildren.org/English/ages-stages/baby/teething-tooth-care/Pages/Amber-Teething-Necklaces.aspx (accessed 2021 Oct. 4).
- Healthy teeth for children. Ottawa: Canadian Paediatric Society; 2021. Available: https://caringforkids.cps.ca/handouts/healthy-living/healthy_teeth_for_children (accessed 2021 Oct. 4).
- Keep your young child safe around the house. Ottawa: Canadian Paediatric Society; 2020. Available: https://caringforkids.cps.ca/handouts/safety-and-injury-prevention/keep_your_young_child_safe (accessed 2021 Oct. 4).
- Hardie JH, Landale NS. Profiles of risk: maternal health, socioeconomic status, and child health. J Marriage Fam. 2013;75(3):651-66.
- Desai S, Alva S. Maternal education and child health: is there a strong causal relationship? Demography. 1998;35(1):71-81.
- Bryan MA, Evans Y, Morishita C, Midamba N, Moreno M. Parental perceptions of the Internet and social media as a source of pediatric health information. Acad Pediatr. 2020;20(1):31-8.



