Abstract
Objectives:
Although routine dental care is essential for both oral and overall health, in Canada, access to such care is uneven. Those with low or medium income and no workplace dental coverage often face financial barriers in accessing dental care. However, the factors that affect access — income, employer-provided health benefits and public dental care subsidy programs — have changed over the decades. This study examines the net impact of these factors on long-term trends in dental care access among different groups in Canada over the past 5 decades.
Methods
Using data from 1 235 268 respondents to 20 Canadian cross-sectional surveys administered between 1972 and 2017, we estimated the proportion of people who had at least 1 consult with a dental professional over the past 12 months. Prevalence trends by region, age group, education and income level were compared.
Results:
In each age group, the proportion of people consulting a dental professional at least annually gradually increased over the last 5 decades. During the recession of the early 1990s, a temporary drop in use occurred, particularly among younger age groups. We noted significant regional differences in use among individuals in the same age group: rates were highest in Ontario and British Columbia and lowest in Quebec and the Atlantic provinces. Marked differences in use by level of education and income persisted over the 5 decades. Dental care use was significantly higher among those with higher levels of education and higher incomes. The increase in overall rates of dental care use suggest that an increasing fraction of Canadians have higher incomes or are better educated, or both. Nevertheless, about a third of Canadians ≥ 15 years did not receive dental care in 2015.
Conclusions:
Given that dental care is almost wholly privately funded and displays a high degree of income-related inequity, there is an urgent need for policy action to address unequal access to dental care in Canada.
Canadians are among the largest spenders and users of dental care globally, yet many face financial barriers to dental care.1 Such individuals are typically less affluent and lack an employer-sponsored health-benefit plan.1-3 People with access to dental care are more likely to receive basic preventive services, and any oral diseases are more likely to be detected at earlier stages.4 As a result, they are also more likely to maintain good oral health.4 It follows that financial barriers to dental care can result in compromised oral health and health-related quality of life. These barriers also result in lost productivity and higher medical and hospital care costs.1
The relation between income and access to dental care in Canada is well known.1 Less is known about how this relation evolved. Over the last 5 decades, average income levels in Canada have increased markedly. Data from the World Inequality Database indicate that the average, inflation-adjusted income of Canadian adults (≥ 20 years) increased by a factor of 2.25 between 1960 and 2022.5 Rates of senior poverty declined sharply in the 1970s and 1980s.6 This income growth has likely improved the affordability of dental care.
However, over the same period, income inequality increased. Although the share of pre-tax national income held by Canadian adults in the top 10% of income distribution has grown since the late 1980s, the share for those in the bottom half has declined.5 Thus, the marked income gains over the last several decades have not been equally shared. There is also some evidence that the fraction of working-age Canadians with employer-provided dental coverage has declined recently. Specifically, the proportion of Canadians with dental insurance fell by 3% between 2009 and 2018.7 This could be a result of labour market changes: a growing share of those in the labour force provide services as independent contractors and not as employees.8 An additional factor affecting use of dental care was the introduction by provincial governments of limited subsidy programs for youth, seniors and the indigent during the period 1970–2020.1
Little is known about how these changes in income, employment patterns and government subsidies have affected long-term trends in dental care access in Canada. Thus, we sought to provide empirical evidence on this issue by examining trends, over the last 5 decades, in the proportion of Canadians who report having seen or talked to a dental professional at least once in the previous year. This is by no means a comprehensive measure of the use of needed dental care. However, it does reflect the prevalence of at least a minimum level of care — a dental examination — and is measured in most health surveys. We examined trends by income distribution, region of Canada, age group and education level. These trends can show how the income gradient in dental care access in Canada has evolved over time and provide insights into its future direction.
Methods
Study Design and Data Source
We combined 1 235 268 individual observations from 20 cross-sectional surveys of the community-dwelling population of Canada’s 10 provinces that collect information on the use of dental care. These data were obtained from the public use versions of 6 surveys: the 1970–1972 Nutrition Canada National Survey (NCNS); the 1978 Canada Health Survey (CHS); the 1985 and 1991 General Social Survey (GSS); the 1990 Health Promotion Survey (HPS); the 1994, 1996 and 1998 National Population Health Survey (NPHS); and the Canadian Community Health Survey (CCHS), which was conducted periodically from 2001 to 2017. These data were obtained from Odesi, a Canadian social science data repository and online exploration and analysis tool.9
Some of these surveys sampled residents of Canada’s 3 northern territories, Nunavut, the Yukon and Northwest Territories; however, these observations were excluded because of the inconsistent coverage over the years. The surveys targeted individuals living in private dwellings and, thus, excluded residents of long-term care facilities and other institutions. They also did not survey residents of Indian Reserves, full-time members of the Canadian Forces or residents of some remote areas of Quebec. Table 1 shows the sample size for each survey cycle. Most were conducted after 1990; only 2 were conducted in the 1970s and only 1 in the 1980s.
|
Survey |
n |
|---|---|
| Nutrition Canada National Survey, 1972 | 15 074 |
| Canada Health Survey, 1978 | 31 490 |
| General Social Survey, 1985 | 11 200 |
| Health Promotion Survey, 1990 | 13 792 |
| General Social Survey, 1991 | 11 924 |
| National Population Health Survey | |
| 1994 | 16 989 |
| 1996 | 79 172 |
| 1998 | 16 497 |
| Canadian Community Health Survey | |
| 2001 | 121 968 |
| 2003 | 124 124 |
| 2005 | 123 419 |
| 2007 | 121 925 |
| 2009 | 115 230 |
| 2010 | 58 329 |
| 2011 | 6 579 |
| 2012 | 57 649 |
| 2013 | 118 891 |
| 2014 | 59 285 |
| 2015 | 100 864 |
| 2017 | 30 867 |
| Total | 1 235 268 |
These surveys asked participants how many times they had seen or talked to a dentist in the previous year or whether they had seen or talked to a dentist at least once in the previous year. Later versions of the CCHS replaced “dentist” with “dental professional,” which includes dentists, denturists and dental hygienists. We used these data to estimate the proportion of Canadians who reported having consulted a dental professional at least once in the previous year. We estimated this proportion for each survey year and region, stratifying by age group, highest level of education or income level. The 2017 CCHS asked about dental professional consults only for respondents from Ontario. Observations with missing information on dental professional consults or on stratifiers (region, age, education, income) were dropped.
Each of these surveys, except the 1972 NCNS, was conducted by Statistics Canada; the NCNS was conducted by Health Canada. All but the 1972 NCNS and the 1978 CHS were telephone surveys. The NCNS and CHS were administered through a combination of self-completed, written responses to a questionnaire and interviewer-administered surveys conducted at the respondent’s home. The surveys included observation-specific weights that adjusted for household non-response and other factors that made population estimates consistent with known province–age–sex totals. We used these survey weights when estimating the proportion of the residential population that obtained dental care in the previous year.
Each of the surveys indicated the respondent’s province of residence, except for the public use version of the 1978 CHS, which grouped respondents from Alberta, Saskatchewan and Manitoba in the Prairie region. Similarly, respondents from New Brunswick, Nova Scotia, Prince Edward Island and Newfoundland-Labrador were grouped in the Atlantic region. To ensure comparability with the 1978 CHS, for most analyses, we used the CHS regional identifiers (British Columbia, Prairie, Ontario, Quebec and Atlantic regions) for all surveys. We also categorized respondents into 5 age groups — 15–19, 20–24, 25–44, 45–64 and ≥ 65 years — as the source of dental coverage varies across these groups. The youngest age group often obtained dental care coverage from a parent. This was also the case for some in the 20–24 group; others in this age group were reliant on workplace benefits. The prime working age groups were 25–44 and 45–64. Many of those in the remaining group, those ≥ 65 years, were retired and no longer eligible for workplace health benefits.
Respondents were divided into 3 categories that reflect pre-tax household income from all sources. The categories of household income varied across survey years. To standardize, we estimated actual household income by taking the midpoint of each category. For instance, income of $20 000–$29 999 was taken to be $25 000. The income assigned to the open-ended top category (such as ≥ $100 000) was estimated as 25% above the top value (so, $125 000 for the ≥ $100 000 category). Next, we adjusted incomes for inflation using the Statistics Canada annual national all-item consumer price index.10 This adjustment measures incomes in 2002 dollars; $75 000 in 2002 dollars is worth about $100 000 in 2017 dollars. Finally, we divided respondents into 3 groups of real annual household income: < $30 000, $30 000 to $74 999 and ≥ $75 000.
We also placed respondents in 4 categories that reflect their highest level of education: less than high school diploma, high school diploma, some postsecondary education and completed a college diploma or university degree. Educational levels are more reliably measured than income: response rates are higher and are less subject to misreporting. Moreover, education is highly correlated with income. Thus, the dental care–educational attainment gradient provides an alternative way to assess the dental care–household income gradient.
We fitted a median spline curve to the annual estimates. The spline estimate fits a smooth curve through the yearly estimates in a way that captures local trends in dental care use, while smoothing out fluctuations in the estimates obtained from surveys conducted in close succession. All analyses were conducted in Stata v. 17.0 (StataCorp LLC, College Station, Tex.).
Results
We estimated the proportion of people ≥ 15 years in each region who reported having consulted a dental professional at least once in the last year (hereafter referred to as “dental care use”). Several patterns are evident (Figure 1). First, dental care use increased from the late 1970s to late 2010s in all regions, especially Quebec and the Atlantic region. Second, regional differences in dental care use persisted over time. Rates were highest in the relatively affluent provinces, Ontario and British Columbia; Quebec and the Atlantic provinces had the lowest rates. However, the differences across regions appear to be narrowing over time as a result of marked growth in dental care use in Quebec and the Atlantic region. Third, the rates of dental care use declined in all regions during the recession of the early 1990s. Finally, growth rates in all regions appear to be plateauing or slowing. The national average rate of dental care use for those ≥ 15 years in 2015 was 68%.
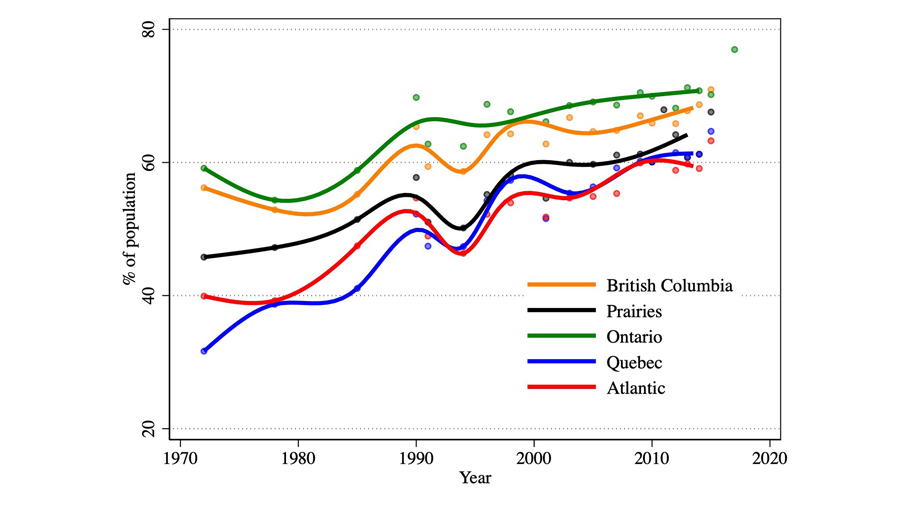
*Median spline curve fit to the region-specific estimates.
Figure 1: Percentage of the population aged ≥ 15 years who consulted a dental professional at least once during the past year by region, 1972–2017.*
We also looked at the proportion of people in various age groups who visited a dentist at least annually (Figure 2). Data from the 2017 CCHS was omitted, as it surveyed Ontario residents only. Dental care use has increased across all age groups from the early 1970s to late 2010s. The largest increases occurred among older adults, those ≥ 65 years. Differences in dental care use between age groups appears to be narrowing over time, although dental care use tended to decrease over the lifecycle, with rates highest for 15–19 year olds and lowest for seniors over the entire period.
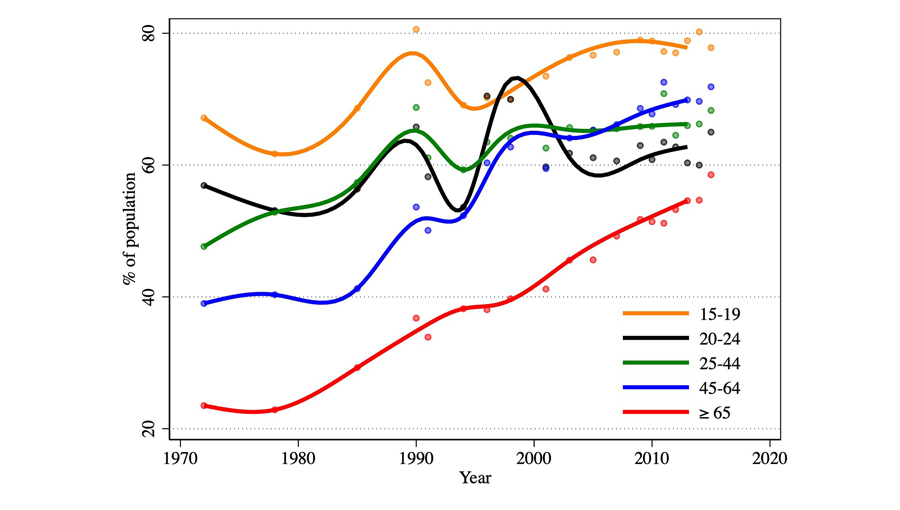
*Median spline curve fit to the age-specific estimates.
Figure 2: Percentage of the population aged ≥ 15 years who consulted a dental professional at least once during the past year by age group, 1972–2015.*
However, the relative rates of dental care use for those 20–24, 25–44 and 45–64 varied over time. In the mid-1970s, rates declined uniformly with age. By the late 2010s, the rankings reversed: those 45–64 years had the highest use, followed by those 25–44 and then those 20–24. Indeed, the rates for the 25–44 years group plateaued over the period 2000 to about 2013, while rates for those 45–64 continued to grow.
The final striking observation is the impact of the economic recession of the early 1990s on dental care use for those under 65 years. The impact is most evident for teens aged 15–19 years. Rates eventually rebounded as the economy recovered. There is also some evidence of a reduction in rates of dental care use among those under 65 during the recession of the early 1980s. The evidence is less clear, however, given the small number of surveys conducted in the 1970s and 1980s.
We explored how the trend in dental care use of different age groups varies across the provinces (Figure 3). As for the national trend, dental care use was highest among young respondents (15–19 years) and lowest among seniors (≥ 65 years) in all provinces. Rates of dental care use among adults ≥ 25 years gradually increased, whereas rates among younger people appear to have plateaued. There were persistent interprovincial variations in use, with the highest rates in Ontario and British Columbia and the lowest in Newfoundland and Quebec. Variation in provincial rates for each age group (with the possible exception of those 20–24 years) appears to have decreased in the latter part of the sample period.
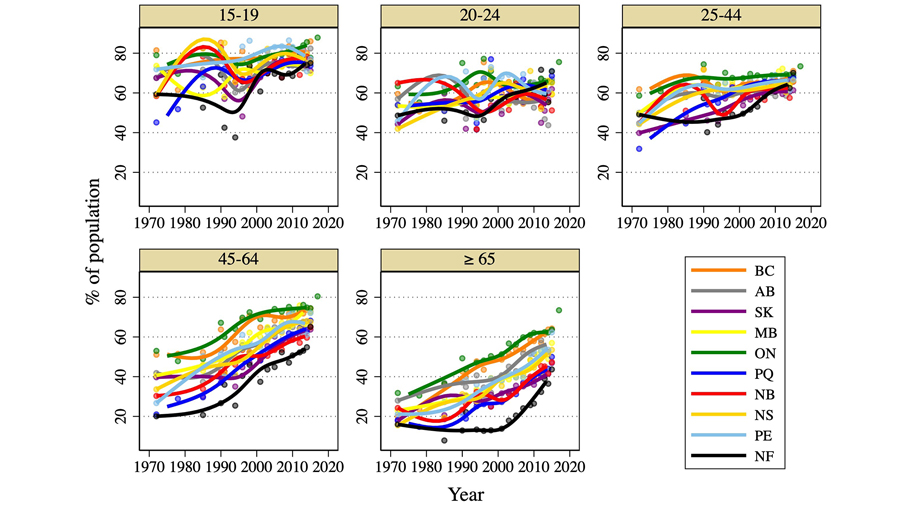
*Median spline curve fit to the province-specific estimates.
Figure 3: Percentage of the population who consulted a dental professional at least once during the past year, by province and age group, 1972–2017.*
Graphs by region highlight the convergence over time of the rates of dental care use by the different age groups (Figure 4). Also, in 3 relatively affluent regions, British Columbia, the Prairies and Ontario, rates of dental care use of those ≥ 65 years is catching up to the rates for younger adults. In Quebec and the Atlantic region, rates of dental care use of those ≥ 65 years remain markedly lower than for adults < 65 years.
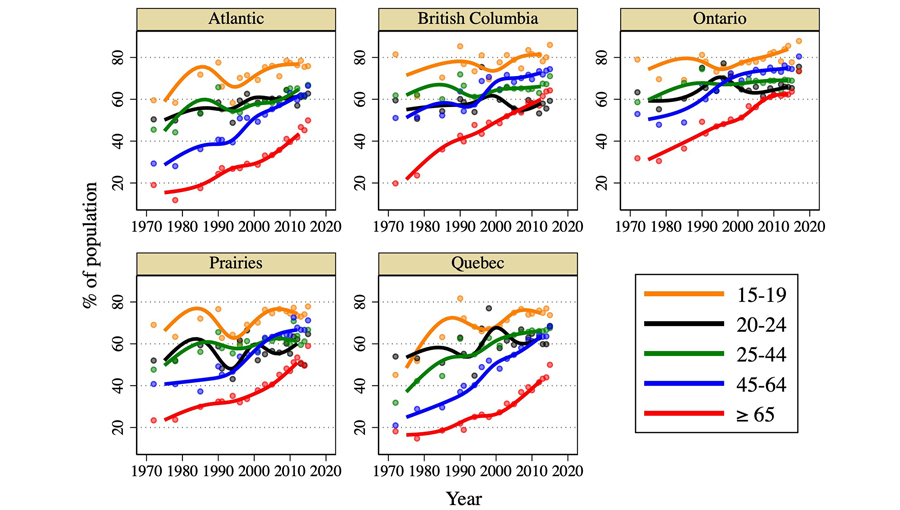
*Median spline curve fit to the age-group specific estimates.
Figure 4: Percentage of the population who consulted a dental professional at least once during the past year, by age group and region of Canada, 1972–2017.*
To estimate trends in dental care use by level of education, we restricted our sample to those ≥ 25 years, given that the highest educational attainment status of those still in school at the time of the survey was not available. Those with higher levels of education had higher rates of dental care use, and these differences persisted over time (Figure 5). Rates of dental care use among those who had not completed high school declined over the 1970s into the mid 1980s, and gradually increased thereafter. However, the rates of dental care use of this group remained below the rates for those with higher levels of education, especially in Quebec and the Atlantic provinces.
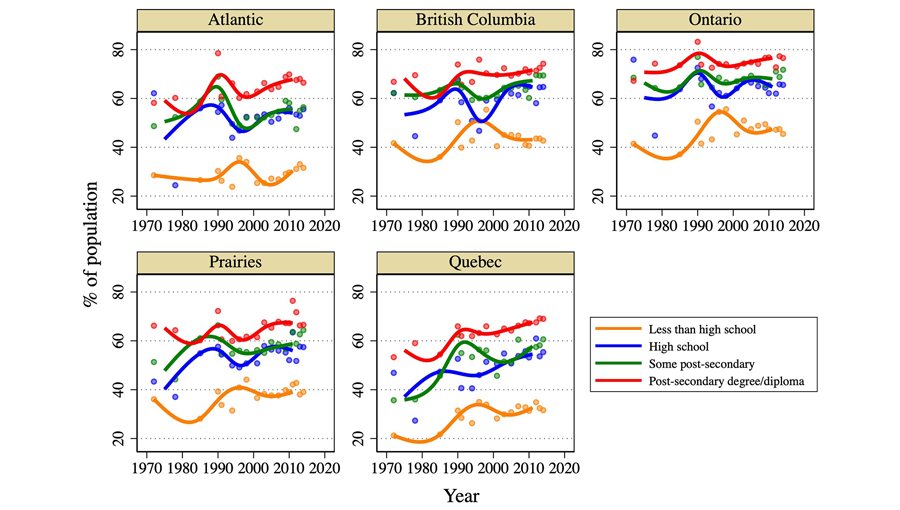
*Median spline curve fit to the education-level specific estimates.
Figure 5: Percentage of the population ≥ 25 years of age who consulted a dental professional at least once during the past year by highest level of education and region of Canada, 1972–2017.*
Trends in dental care use by people ≥ 25 years by level of household income and region showed an increase over time (except during the recession of the early 1990s) for all income groups (Figure 6). However, rates of use were higher with higher household income. Differences in dental care use among income groups use were particularly large in Quebec and the Atlantic region, but the gap appears to be narrowing because of increasing rates of dental care use by the lowest income group.
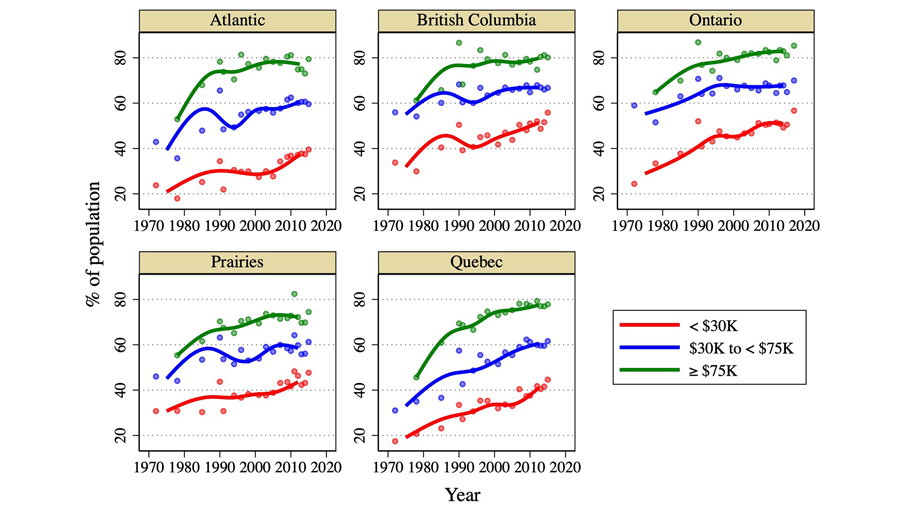
*Median spline curve fit to the education-level specific estimates.
Figure 6: Percentage of the population ≥ 25 years of age who consulted a dental professional at least once during the past year, by real annual household income and region of Canada, 1972–2017.*
Discussion
This study presents evidence of the long-term trends in dental care use in Canada based on repeated cross-sectional population surveys, all but one of which was conducted by Statistics Canada. The results indicate that dental care use — measured as the proportion of Canadians who report having consulted a dental professional at least once in the past year — has increased over the last 5 decades, especially among seniors (≥ 65 years) and older adults (45–64 years). Around this secular increase, we observed temporary reductions in use around the recession of the early 1990s.
Although dental care use has gradually increased, disparities between socioeconomic groups and regions have persisted over time. In each age group, dental care use has been highest among individuals in Ontario and British Columbia, with Quebec and the Atlantic provinces moderately lagging behind. This is consistent with the findings of previous studies that a greater proportion of Ontario and British Columbia residents make annual dental visits.12,13 In both Ontario and British Columbia, the number of dentists per capita is higher than in other Canadian provinces.14 The greater access (with subsequent higher service use) in these provinces may be attributed to their demographic composition or income levels.
Differences in dental care use by level of household income also persisted over time. This no doubt reflects the fact that lower income households are less able to pay for dental care costs and are less likely to have private dental insurance coverage (which is usually a benefit for employees in permanent, full-time jobs).12,13,15 There is some evidence, however, that income-related differences in dental care use in Quebec and the Atlantic regions are decreasing.15 In our data, this appears to be driven by a recent plateauing of dental care use among individuals in the 2 highest income groups and a growth in use among those in the lowest income group. It is unclear whether the increase in use of dental care among lower income households reflects higher levels of income in these groups or perhaps public subsidies for dental care targeted at lower income households.12 Further research may help elucidate the impact of dental care subsidies on rates of dental care use among lower income households.
In each region, more highly educated people also had higher rates of dental care use. This likely operates through 2 mechanisms. First, people with higher levels of education tend to be more aware of the importance of oral and dental hygiene and, hence, more likely to seek dental care.16,17 Second, education also correlates with dental coverage and higher income, both of which relax financial constraints on access to care. There was less growth over time in education-level-specific rates of dental care use. The fact that overall rates of use are increasing, thus, likely reflects an increase in educational attainment of the population. Indeed, the proportion of the population without a high school degree is declining over time, while the proportion with a post-secondary degree has increased.18
Our study period ends in 2017, and of course much has happened since then. The COVID-19 pandemic disrupted the labour market and household incomes,19 and the post-pandemic recovery is ongoing. It is unclear how income-driven inequality in dental access has changed since 2017. Also, the federal government recently announced the launch of the Canadian Dental Care Plan (CDCP), which aims to improve dental care coverage for approximately 9 million uninsured Canadians with a family income < $90 000.20 Initially, only seniors are eligible for the subsidy, but eventually younger people will become eligible. The launch of this program may help narrow the income-dental care use gap. Estimating the impact of the CDCP on trends in dental care access and the provision of needed dental care is a fertile topic for future research.
This study has several limitations. First, self-reported consultation with a dental professional in the previous year is used as a proxy measure for access to dental care. This is by no means a comprehensive measure of use of needed dental care.1 Instead, it typically reflects a minimum level of dental care. Second, as with any survey analysis, some individuals may have difficulty recalling events from the previous 12 months. Third, combining respondents from provinces in the Atlantic and Prairie regions enhances comparability of the estimates over time but, of course, limits our ability to follow the trends in each province of these regions. Fourth, given that relatively few surveys were conducted in the 1970s and 1980s, evidence of trends in dental care access during this period are weaker than in later periods. Finally, the surveys exclude residents of long-term facilities and Indian reserves. Dental care access of both these groups tends to be lower than that for other Canadians.21,22
In conclusion, dental care access in Canada has increased substantially over the years, but about a third of Canadians ≥ 15 still do not obtain even a minimum level of dental care (an annual consult with a dental professional). These people tend to have lower levels of education and lower incomes. Although isolated provincial interventions may have contributed to recent improvements in overall dental care access, broader and coordinated policies are urgently needed to expand dental care access for marginalized groups in Canada.
THE AUTHORS
Corresponding author: Paul Grootendorst, PhD, Leslie Dan Faculty of Pharmacy, University of Toronto, 144 College St., Toronto ON M5S 3M2. Email: paul.grootendorst@utoronto.ca
This research was supported by an operating grant from the Canadian Institutes of Health Research, funding reference number: 112235. We acknowledge Minsup Shim for his research assistance.
This article has been peer reviewed.
References
- Quiñonez C. The politics of dental care in Canada. Toronto: Canadian Scholars’ Press; 2021.
- Allin S, Farmer J, Quiñonez C, Peckham A, Marchildon G, Panteli D, et al. Do health systems cover the mouth? Comparing dental care coverage for older adults in eight jurisdictions. Health Policy. 2020;124(9):998-1007.
- Ramraj C, Sadeghi L, Lawrence HP, Dempster L, Quiñonez C. Is accessing dental care becoming more difficult? Evidence from Canada’s middle-income population. PloS One. 2013;8(2):e57377.
- Oral health in America: advances and challenges. Bethesda, MD: US Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research; 2021. Available: https://www.nidcr.nih.gov/sites/default/files/2021-12/Oral-Health-in-America-Advances-and-Challenges.pdf (accessed 2024 April 1).
- Chancel L, Piketty T, Saez E, Zucman G. World inequality report 2022. World Inequality Lab, wir2022.wid.world; 2022. Available: https://wir2022.wid.world/www-site/uploads/2023/03/D_FINAL_WIL_RIM_RAPPORT_2303.pdf (accessed 2023 Oct. 12).
- Milligan K. The evolution of elderly poverty in Canada. Can Public Policy. 2008;34(4):S79-94. Available: https://www.utpjournals.press/doi/10.3138/cpp.34.4.S79 (accessed 2024 Feb. 7).
- Lange TC. Comprehensive dental care in Canada: the choice between Denticaid and Denticare. Calgary: School of Public Policy Publications, University of Calgary; 2020. Available: https://journalhosting.ucalgary.ca/index.php/sppp/article/view/69676 (accessed 2024 April 1).
- Jeon SH, Liu H, Ostrovsky Y. Measuring the gig economy in Canada using administrative data. Can J Economics. 2021;54(4):1638-66.
- Odesi. Find data. Toronto: Ontario Council of University Libraries; 2023. Available: https://odesi.ca/en (accessed 2024 Jan. 25).
- Table 18-10-0005-01 Consumer price index, annual average, not seasonally adjusted. Ottawa: Statistics Canada; 2023. Available: https://doi.org/10.25318/1810000501-eng (accessed 2023 Oct. 12).
- Grignon M, Hurley J, Wang L, Allin S. Inequity in a market-based health system: evidence from Canada’s dental sector. Health Policy. 2010;98(1):81-90.
- Andkhoie M, Pandovska-Pelivanova E, Emmanuel S, Lateef F, Szafron M, Farag ME. Demand and burden of dental care in Canadian households. Int J Econ Finance. 2014;6(9):73-82. Available: https://ccsenet.org/journal/index.php/ijef/article/download/37316/22017 (accessed 2024 Apr. 3).
- Health workforce in Canada, 2017 to 2021: overview — data tables. Ottawa: Canadian Institute for Health Information; 2022. Available: https://www.cihi.ca/en/health-workforce-in-canada-overview (accessed 2023 June 21).
- Ravaghi V, Farmer J, Quiñonez C. Persistent but narrowing oral health care inequalities in Canada from 2001 through 2016. J Am Dent Assoc. 2020;151(5):349-57.
- Tellez M, Zini A, Estupiñan-Day S. Social determinants and oral health: an update. Curr Oral Health Rep. 2014;1:148-52.
- Vano M, Gennai S, Karapetsa D, Miceli M, Giuca MR, Gabriele M, et al. The influence of educational level and oral hygiene behaviours on DMFT index and CPITN index in an adult Italian population: an epidemiological study. Int J Dent Hyg. 2015;13(2):151-7.
- Friesen J. Census shows high rate of undergraduate and college education among Canadians, but complex trends lie behind it. Globe and Mail. 2022;4 Dec. Available: https://www.theglobeandmail.com/canada/article-census-2021-university-college-graduate/ (accessed 2023 Aug. 8).
- Clarke S, Fields A. Employment growth in Canada and the United States during the recovery from COVID-19. Ottawa: Statistics Canada; 2022. Available: https://www150.statcan.gc.ca/n1/pub/36-28-0001/2022012/article/00001-eng.htm (accessed 2023 Aug. 8).
- Making dental care more affordable in Canada. Ottawa: Health Canada; 2023. Available: https://www.canada.ca/en/health-canada/news/2023/12/making-dental-care-more-affordable-in-canada.html (accessed 2023 Dec. 15).
- Yoon MN, Ickert C, Slaughter SE, Lengyel C, Carrier N, Keller H. Oral health status of long-term care residents in Canada: results of a national cross-sectional study. Gerodontology. 2018;35(4):359-64.
- Report on the findings of the First Nations Oral Health Survey (FNOHS) 2009-2010. Ottawa: First Nations Information Governance Centre; 2012. Available: https://fnigc.ca/wp-content/uploads/2020/09/fn_oral_health_survey_national_report_2010.pdf. (accessed 2023 Nov. 6).



