Abstract
Objective: To gain a better understanding of the extent to which rectangular collimation is being used in private practice and the barriers to adoption by practitioners.
Methods: Licensed dentists in private practice were asked to answer a survey composed of 17 multiple-choice questions and 1 open-ended question regarding demographics, radiation safety, image receptor type, intraoral imaging techniques and use of rectangular collimation.
Results: Among all participants (n = 82), 86.6% used digital systems (n = 71) and 13.4% conventional film (n = 11). Most (74.0%, n = 60) were aware of the benefits of using rectangular collimation, with 5.5% reporting not knowing of the existence of this device (n = 3). Only 12.9% of the dentists reported using rectangular collimation routinely (n = 10). The youngest and oldest age groups had the lowest compliance rates, 5.6% and 0%, respectively.
Conclusion: Although 74.0%, (n = 60) of private practitioners were aware of the benefits of using rectangular collimation to reduce radiation dose, only 12.2% (n = 10) used it routinely for intraoral imaging. Barriers to implementing rectangular collimation in private practice settings included challenges in training support staff and fear of an increase in the occurrence of technical errors that would result in re-exposure of patients.
According to the United Nations Scientific Committee on the Effects of Atomic Radiation, 480 million diagnostic dental examinations are performed worldwide annually.1 Intraoral radiographs are the most common dental radiographs performed, with numbers approaching 100 million in the United States,2 63 million in Europe3 and 14 million in Canada.4 Although radiation exposure during conventional intraoral imaging, particularly in comparison with medical imaging, is very low, because several intraoral images are performed in dental practice, the collective dose to the population as a whole is clinically important. The ultimate goal of an intraoral radiograph is to provide diagnostic value, while adhering to the “as low as reasonably achievable” (ALARA) principle to minimize radiation exposure. Rectangular collimation (Figure 1) restricts the size and shape of the beam from round to rectangular to correspond more closely with the size of rectangular receptors and increases the quality of the image by reducing scatter. The routine adoption of rectangular collimation for taking intraoral images would reduce the ionizing radiation dose to the population and the individual.2,5,6 A recent systematic review reinforced the evidence that rectangular collimation reduces radiation dose by at least 40% when compared to round collimation.7

The use of rectangular collimation is supported by the American Dental Association (ADA)2 and highly suggested by the National Council on Radiation Protection.8 A 2001 survey involving 65 dental schools across North America found that 47% used rectangular collimation with 52% using round collimation exclusively.9 A study from the United Kingdom (UK) reported a use rate of 37% among general practitioners and 40% among endodontists.10 However, use in dental private practice remains low.
This research project aimed to gain a better understanding of the extent to which rectangular collimation is being used in private practice in Edmonton, Alberta, and the barriers to its adoption by practitioners. The specific research questions were as follows. Are private practitioners aware of the benefits of rectangular collimation? Are private practitioners using a rectangular collimator for routine intraoral imaging? What are the barriers to the implementation of rectangular collimation in private practice settings?
Methods
Eligibility Criteria
All licensed dentists practising in Edmonton (n = 1009) were invited to complete a survey. Consent to participate was included in an information sheet (Appendix 1). No inducements (financial or otherwise) were offered to participants. Surveys completed by dentists who were not licensed in Alberta were ineligible.
The survey consisted of a questionnaire, with 17 multiple-choice questions adapted and modified from a previously published survey (Lee and Ludlow 2013).11 One open-ended question asking participants to describe challenges preventing use of a rectangular collimator in their practice was also included. Questions related to participant demographics, consent from patients for imaging, response to patient questions regarding dose, intraoral technique and image receptor type used, rectangular collimation awareness and use and barriers to use. Photos and illustrations were included in the survey to facilitate visualization of the techniques and equipment described in it. The complete version of the questionnaire is available in Appendix 2.
Participation was through a web-based survey system (SurveyMonkey Inc., Palo Alto, Calif., USA) and was accessible on portable computers or via a participant’s device by scanning a QR code (2-dimensional barcode) or by opening a link to the web-based survey. Dentist respondents had access to the research team by email or telephone; however, no one on the research team was contacted. The participants preferred to clarify their concerns verbally before they started to answer.
Statistical Analysis
Collected data were categorized according to gender, age, general or specialist practitioner and years of practice. Mean values, frequencies and standard deviations were calculated. The normality of distributions was tested for all variables. A Χ2 test of independence was performed to examine the relation between awareness of rectangular collimation benefits and gender. Considering the number of survey respondents (n = 82) and the city’s population of dentists (n = 1009) the confidence interval (CI) is 8.74% when the confidence level is set at 90%. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS v. 22.0).
Ethics Approval
The study was conducted in full accordance with the Helsinki Protocol. Approvals for the protocol and consent processes were obtained from the Research Ethics Board at the University of Alberta, Edmonton, under study Pro00079995 and a cross-sectional study design was planned.
Results
The first response to our survey (n = 64) was considered low; thus, strategies were adopted to increase the number of participants and compliance among private practitioners. Active private practitioners attending continuing education events and faculty who also maintain active private practices were also recruited. In total, 85 surveys were collected from March to November 2018; 3 were excluded from analysis, as they were incomplete. The final number of surveys analyzed was 82, representing an 8.1% response rate.
The respondents included 52 (63.4%) men and 30 (36.6%) female. In terms of age groups, 36 (43.9%) of participants were 24–35 years old; 20 (24.4%) were 36–47 years old, 14 (17.1%) were 48–58 years old and 12 (14.6%) were ≥ 59 years old. Most of the dentists, 40 (48.7%) had been in practice < 10 years, while 18 (22.0%) had more than 30 years of experience. Of the 82 responses, 69 (84.1%) were from general practitioners and 11 (13.4%) from specialists and 2 respondents preferred not to declare. Type of specialty was not reported by respondents, but no oral and maxillofacial radiologists were invited to complete the survey.
All respondents used intraoral radiographs routinely: 71 (86.6%) using digital systems and 11 (13.4%) using conventional film. Of digital users, 63 (88.2%) declared using solid-state detectors (sensors) and 8 (11.8%) photostimulable phosphor technology (PSP plates). Most dentists 81 (98.7%) routinely used a receptor holder and 67 (82.1%) regularly used an aiming ring to align the tube head. When taking periapical radiographs, 65 (79.5%) used the paralleling technique routinely and 16 (20.5%) the bisecting angle technique
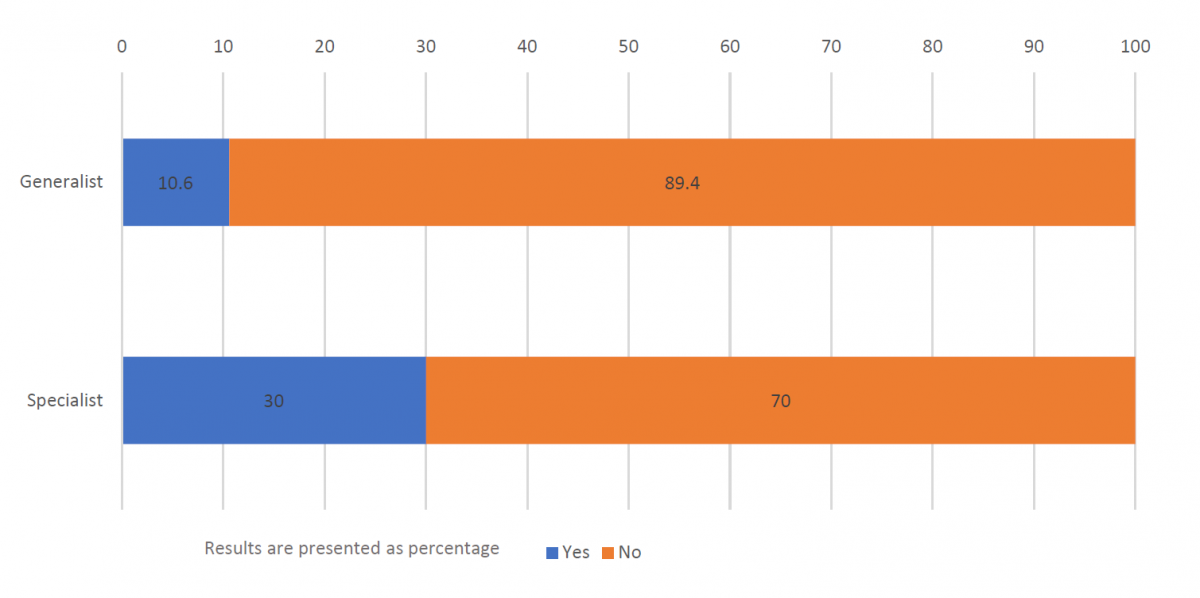
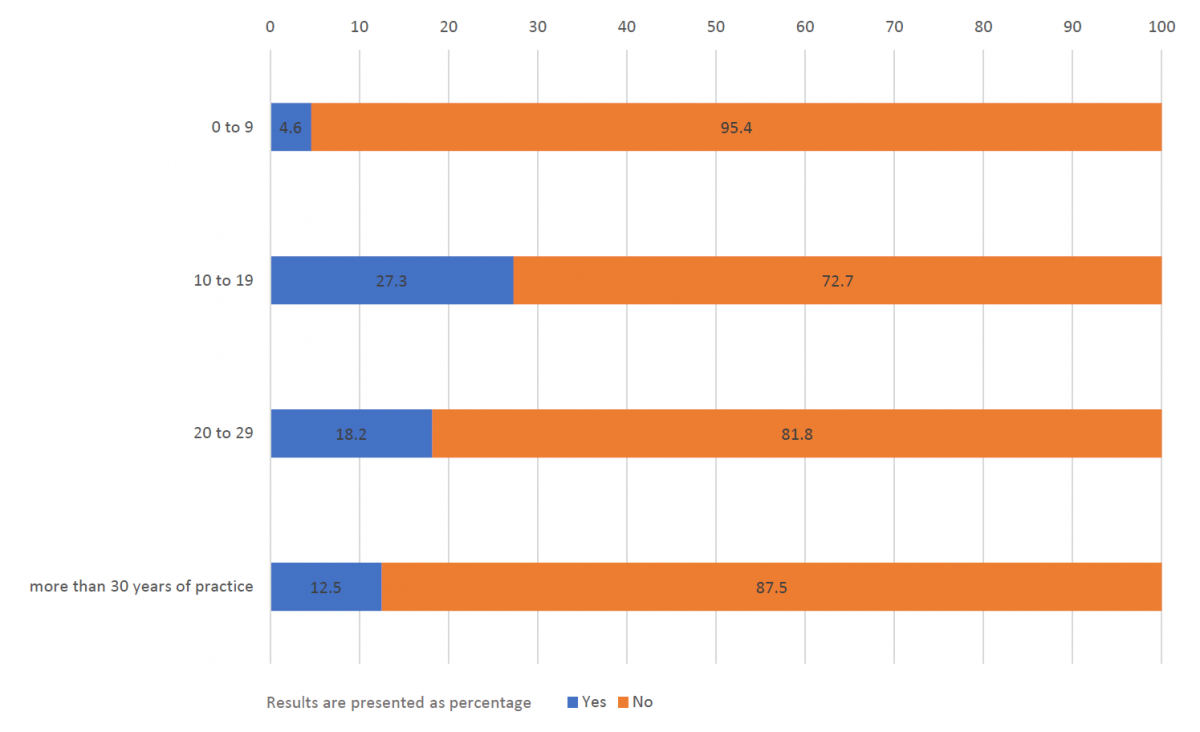
Regarding rectangular collimation, 60 (74.0%) of respondents were aware of the benefits but only 10 (12.2%) regularly used rectangular collimation to perform intraoral imaging. Three respondents reported not knowing about the existence of rectangular collimating devices. Figure 2a shows greater use of rectangular collimation by specialist practitioners (30.0%) compared with generalists (10.6%). The rate of adoption of rectangular collimation by recently graduated dentists (up to 9 years in practice) was very low (4.6%) compared with that of dentists with 10–19 years of clinical experience (27.3%; Figure 2b). The same trend was noted with respect to dentists’ age. The youngest and the oldest age groups presented the lowest rates of use: 5.6% and 0%, respectively. The relation between awareness of rectangular collimation benefits and gender was significant, with women more likely than men to be aware of the benefits of using rectangular collimation, p = 0.003.
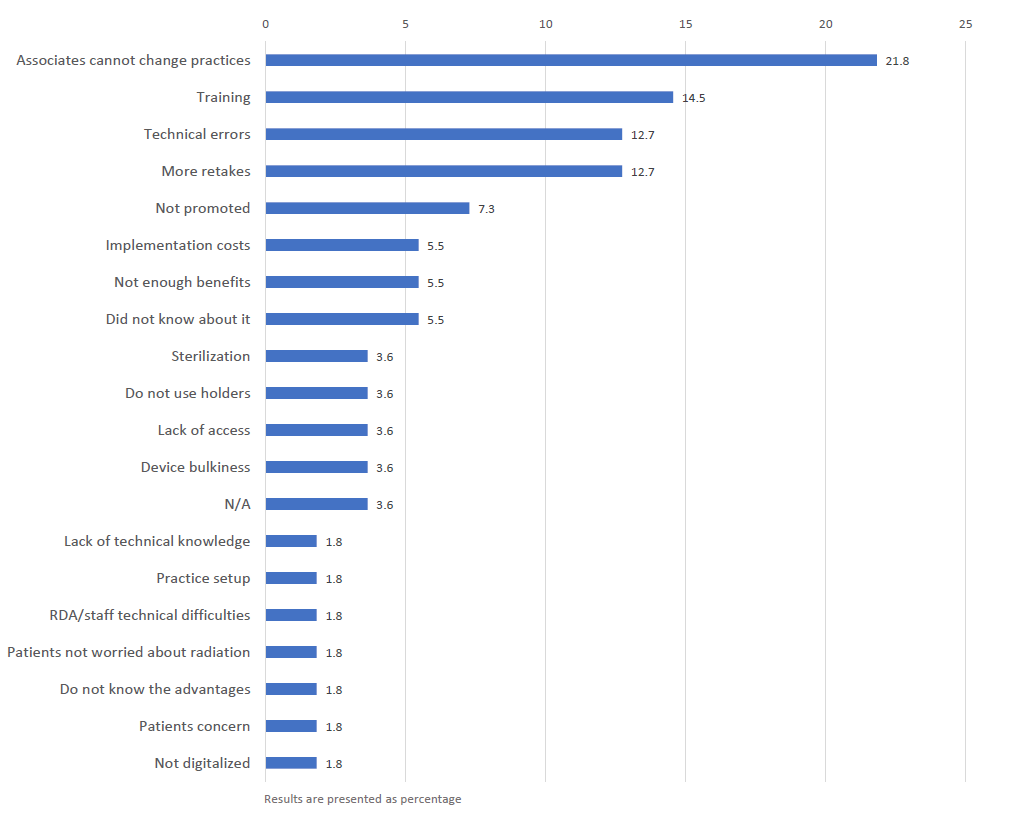
In answering the open-ended question, participants (n = 55) described why they did not use rectangular collimation (Figure 3). The main reasons were lack of or challenges with staff training (14.5%), fear of technical challenges related to rectangular collimation use (12.7%) and fear of increased retakes (12.7%). Lack of technical knowledge by dentists on how to use rectangular collimation, a clinical environment that does not promote its use and concern that patients might become more concerned about radiation dose were also mentioned. A common response (21.8%) from dentists working as associates in a dental practice was that they had limited control and decision-making capacity regarding use and purchase of equipment, including radiography equipment.
Patient concerns about radiation safety were usually addressed by the dentists 39 (48.1%), rather than their dental assistant 14 (17.3%), with a frequency of once a month most common (68.4%). Specialists reported receiving more questions than generalists regarding radiation safety: 27.3% “always” and 45.5% “occasionally” had to address these questions. One generalist never discussed the topic with their patients (1.2%), while most 81 (89.9%) encountered questions from patients regarding the radiation dose from dental radiographs. When explaining radiation safety, 30.9% of the respondents compared dose level with radiation exposure during day-to-day activities. Patient consent specifically for performing radiographs was always obtained by 70.0% of the dentists, with 10.0% never acquiring specific consent.
Discussion
Although the use of 3-dimensional imaging is increasing, 95% of the images obtained in dental settings continue to be 2-dimensional intraoral radiographs.12 The basic principles of radiation exposure continue to be justification, optimization and dose limitation.12,13 The ADA and the International Commission on Radiological Protection recommend the use of rectangular collimation as a “best practice” for reducing patient radiation dose because it restricts the beam to the rectangular dimension of the receptor.2,8,14,15 For example, a full mouth series performed with a charge-coupled device sensor using rectangular collimation reduces the effective dose from 85 μSv to an estimated 17 μSv.15
Our study results show that, although most of the dentists surveyed (74%) were aware of the dose-reduction benefits of rectangular collimation, only 12.9% routinely used it. These findings are similar to the Lee and Ludlow study11 of Korean dentists in 2013, which reported a 14.6% rectangular collimation utilization rate. In contrast to the Korean study, in which 30% of the practitioners were never asked about radiation hazards, only 2.5% of our study participants reported never receiving questions about radiation safety from patients. A Canadian study from 1994 reported a rectangular collimation use rate of 8%16; a study from the UK showed an increase in the use of rectangular collimation by generalists from 34% in 2005 to 63% in 201210,17; and an increase of 6% was reported in Belgium in 200518 and 15% in Switzerland in 2004.19 These differences in adoption rate among countries may be a result of disparities in radiation protection policies and standards and the extent to which these standards are monitored and enforced by regulatory agencies. Education, familiarity and, subsequently, comfort and expertise with rectangular collimator use may also affect adoption. Dentists who participate in continuing education are more likely to use rectangular collimators,7,20,21 and if an oral radiologist is available, the likelihood of collimator use increases, because of their knowledge and attention to radiation safety measures.20
As more dental schools and teaching colleges are now demonstrating rectangular collimation in preclinical radiology teaching labs and using it for patient care, recent graduates may be more likely to be aware of its benefits and to have had more hands-on experience using collimation than previous graduates.9 However, our study showed that even though most respondents, especially women, recognized the benefits, the implementation rate of both male and female practitioners was low. Dentists working as associates reported limited influence or control over what radiology equipment was used or purchased in their offices. This suggests that for implementation to proceed, raising awareness and gaining the support of those with purchasing authority must occur. Resistance to change and reluctance to modify established dental practices may also hinder implementation, as for other evidence-based practices in dentistry.9,22
Barriers to use, either perceived or experienced by the participants, included concerns over technique errors. Cone cuts result from poor alignment of the beam indicating device or a failure to ensure that the receptor is centered within the aiming ring. A previous study reported that a common complaint about rectangular collimation is the occurrence of cone cuts on radiographic images, which can reduce their diagnostic yield.23 In agreement, 25% of our participants mentioned “positioning difficulty” and/or “technical challenges” as barriers to using rectangular collimation. A 2011 study found that the use of collimators with appropriate film-holding apparatus did not affect the diagnostic yield of bitewing radiographs enough to necessitate a significant increase in the number of retake images.24 Receptor-holding devices have been shown to reduce alignment errors with circular collimators from approximately 21% to 3% and vertical distortion from 88% to 52%.24 Although cone cuts can be more prevalent with rectangular collimation, they do not lead to a diagnostically unacceptable image.24,25 In a comparative study, Thornley et al.23 found that even though use of rectangular collimation increased retake imaging by 7%, rectangular collimators were still valuable in reducing radiation exposure.
Patience, skill/training and attention to detail can reduce cone cuts and retake rates to levels similar to those achieved without collimator use.7 In our study, the challenge of training support staff to use rectangular collimation was described as a barrier. Technique errors related to rectangular collimation have been shown to occur less frequently with more experienced operators.26 While support staff are becoming familiar with equipment and techniques, radiographic examinations may take longer to perform, thus, affecting the speed of image acquisition and patient flow. In this study, it was encouraging to note that beam-aiming rings, essential for accurate collimator alignment, were already being used by most participants. This suggests that many private practices may already own and use other components necessary for successful implementation of rectangular collimators.
Any survey-based research has limitations. Our initial response rate was very low and, hence, we recruited practitioners and faculty who had been attending general dentistry continuing education events to achieve a meaningful confidence interval. This could have introduced bias, as practitioners who attend continuing education events are more likely to use rectangular collimation.7,20,21 The issues we faced during the project were not only related to dentists’ compliance in answering a 10-minute questionnaire, but also the fact that some participants may have been hesitant to comment on radiation protection measures. These factors may have compromised our response rate by limiting the number of participants who chose to attempt the survey. We must also consider the limitations related to the yes-or-no type of survey question, as it is not possible to ascertain the true knowledge of the respondents. A question asking whether a participant had ever tried using rectangular collimation in a practice setting would have been helpful to detect rejection following a negative experience. This would have been helpful to determine whether reported barriers were perceived or actually experienced.
Current evidence implies that instruction through continuing education is the best way to educate dentists in evidence-based dentistry and to change their practice and behaviour.27 Increasing adoption of rectangular collimation in private practice settings requires the education and training of not just dentists, but the whole dental team. Although radiation safety standards and policies emphasize rectangular collimation use as a best practice,4,8,12,13 until the standard is required, inspected and enforced, compliance is likely to remain limited. Another approach is to ensure that all dentistry, dental hygiene and dental assistant training programs mention the dose-reduction benefits of rectangular collimators in their course content and routinely use the technique in preclinical and clinical settings. Finally, for dentists and staff no longer in school, providing more continuing education opportunities (including hands-on training) to help inform and transition the whole dental team is recommended.
Conclusion
In this study, 74% of private practitioners were aware of the benefits of using rectangular collimation to reduce radiation dose, with 12.9% using rectangular collimation routinely for intraoral imaging. Barriers to implementing rectangular collimation in private practice settings included challenges in training support staff and the fear of an increase in the occurrence of technical errors that would result in re-exposure of patients.
THE AUTHORS
Acknowledgement: We thank the dentist-respondents, who kindly took time to answer the survey. We also thank Suraj Chavda for collaboration as a summer research dental undergraduate student, the Centre of Teaching and Learning, University of Alberta, and Francisco Vargas-Madriz for assistance in conducting the survey and data analysis.
Correspondence to: Dr. Anthea Senior, School of Dentistry, Faculty of Medicine and Dentistry, University of Alberta, 5 521, Edmonton Clinic Health Academy, 11405 — 87 Ave NW, Edmonton AB T6C 1C9. Email: senior@ualberta.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- United Nations Scientific Committee on the Effects of Atomic Radiation. UNSCEAR 2008 report to the General Assembly with scientific annexes, volume I: Sources and effects of ionizing radiation. Annex A: medical radiation exposures. New York: United Nations; 2010. Available at: unscear.org/docs/publications/2008/UNSCEAR_2008_Annex-A-CORR.pdf
- American Dental Association, Council on Scientific Affairs. Dental radiographic examinations: recommendations for patient selection and limiting radiation exposure. Washington: U.S. Department of Health and Human Services; 2012 [accessed 2018 Oct. 2]. Available at: http://www.ada.org/~/media/ADA/Member%20Center/FIles/Dental_Radiographic_Examinations_2012.ashx
- Horner K, Rushton V, Walker A, Tsiklakis K, Hirschmann PN, van der Stelt PF, et al. European Guidelines on Radiation Protection in Dental Radiology—The Safe Use of Radiographs in Dental Practice. The Publications Office of the European Union; Luxembourg: 2004. Available at: https://ec.europa.eu/energy/sites/ener/files/documents/136.pdf
- Regulations amending the radiation emitting devices regulations (dental X-ray equipment). Canada Gazette Part I 2016:150(25):18 June [accessed: 2018 Feb. 2]. Available at: http://www.gazette.gc.ca/rp-pr/p1/2016/2016-06-18/html/reg3-eng.php
- Magill D, Ngo NJH, Felice MA, Mupparapu M. Kerma area product (KAP) and scatter measurements for intraoral X-ray machines using three different types of round collimation compared with rectangular beam limiter. Dentomaxillofac Radiol. 2019;48(2):20180183.
- Falk A, Lindhe JE, Rohlin M, Nilsson M. Effects of collimator size of a dental X-ray unit on image contrast. Dentomaxillofac Radiol. 1999;28(5):261-6.
- Shetty A, Almeida FT, Ganatra S, Senior A, Pacheco-Pereira C. Evidence on radiation dose reduction using rectangular collimation: a systematic review. Int Dent J. 2019;69(2):84-97.
- NCRP report no. 145: Radiation protection in dentistry. Bethesda: National Council on Radiation Protection and Measurement; 2003.
- Geist JR, Katz JO. Radiation dose-reduction techniques in North American dental schools. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(4):496-505.
- Orafi I, Rushton VE. A questionnaire study to derive information on the working environment, clinical training, use of ancillary staff and optimization of patient radiation dose within UK dental practice. Int Endod J. 2012;45(8):763-72.
- Lee BD, Ludlow JB. Attitude of the Korean dentists towards radiation safety and selection criteria. Imaging Sci Dent. 2013;43(3):179-84.
- Radiation protection in dentistry: recommended safety procedures for the use of dental x-ray equipment. Safety code 30. Ottawa: Environmental Health Directorate, Health Canada; 1999. Available at: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/ewh-semt/alt_formats/hecs-sesc/pdf/pubs/radiation/99ehd-dhm177/99ehd-dhm177-eng.pdf
- NCRP report no. 177: Radiation protection in dentistry and oral and maxillofacial imaging. Bethesda: National Council on Radiation Protection and Measurement; 2019. Available at: https://ncrponline.org/shop/reports/report-no-177
- Hoogeveen RC, Martens EP, van der Stelt PF, Berkhout WE. Assessment of random error in phantom dosimetry with the use of error simulation in statistical software. Biomed Res Int. 2015:596858.
- Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculations. J Am Dent Assoc. 2008;139(9):1237-43.
- Bohay RN, Kogon SL, Stephens RG. A survey of radiographic techniques and equipment used by a sample of general dental practitioners. Oral Surg Oral Med Oral Pathol. 1994;78(6):806-10.
- Trevor MM, Davies C, Trevor M, Grange S. 2005. Radiation protection practices and related continuing professional education in dental radiography: A survey of practitioners in the North-east of England. Radiography 2005;11(4):255-61.
- Gijbels F, Debaveye D, Vanderstappen M, Jacobs R. Digital radiographic equipment in the Belgian dental office. Radiat Prot Dosimetry. 2005;117(1-3):309-12.
- Aroua A, Buchillier-Decka I, Dula K, Nedjadi Y, Perrier M, Vader JP, et al. Radiation exposure in dental radiology: a 1998 nationwide survey in Switzerland. Dentomaxillofac Radiol. 2004;33(4):211-9.
- Svenson B, Söderfeldt B, Gröndahl HG. Attitudes of Swedish dentists to the choice of dental X-ray film and collimator for oral radiology. Dentomaxillofac Radiol. 1996;25(3):157-61.
- Shahab S, Kavosi A, Nazarinia H, Mehralizadeh S, Mohammadpour M, Emami M. Compliance of Iranian dentists with safety standards of oral radiology. Dentomaxillofac Radiol. 2012;41(2):159-64.
- Geist JR, Katz JO. The use of radiation dose-reduction techniques in the practices of dental faculty members. J Dent Educ. 2002;66(6):697-702.
- Thornley PH, Stewardson DA, Rout PGJ, Burke FJT. Rectangular collimation and radiographic efficacy in eight general dental practices in the West Midlands. Prim Dent Care. 2004;11(3):81-6.
- Parrott LA, Ng SY. A comparison between bitewing radiographs taken with rectangular and circular collimators in UK military dental practices: a retrospective study. Dentomaxillofac Radiol. 2011;40(2):102-9.
- Zhang W, Abramovitch K, Thames W, Leon ILK, Colosi DC, Goren AD. Comparison of the efficacy and technical accuracy of different rectangular collimators for intraoral radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(1):e22-8.
- Johnson KB, Mauriello SM, Ludlow JB, Platin E. Technical performance of universal and enhanced intraoral imaging rectangular collimators. J Dent Hyg. 2015;89(4):238-46.
- Yamalik N, Nemli SK, Carrilho E, Dianiskova S, Melo P, Lella A, et al. Implementation of evidence-based dentistry into practice: analysis of awareness, perceptions and attitudes of dentists in the World Dental Federation-European Regional Organization zone. Int Dent J. 2015;65(3):127-45.
Appendix 1: Study Information Sheet
Project: Rectangular collimator use — a translation to private practice
HERO study # Pro00079995
Principal Investigators: Dr. Anthea Senior and Dr. Camila Pachêco-Pereira
Background
You are invited to participate in a research study as part of a research project assessing dentists in private practice. You are integral to this study as you will be providing your perspective on the use of a rectangular collimator while taking intraoral images. This study will help inform our research team on this specific radiation safety measure and the implementation in a private practice setting. Additionally, the findings of this study may be presented and published as part of our scholarly research in dental education. Before you decide if you wish to take part, you need to understand why the research is being done and what it will involve for you.
Purpose
It has been long understood that rectangular collimation has the potential to significantly reduce unnecessary radiation exposure and improve diagnostic quality on intraoral radiographs. A systematic review from our team has already addressed this issue with an evidence-based focus merging two essential concepts; radiation dose reduction and radiation safety. It showed evidence suggesting that rectangular collimation significantly reduces radiation dose by 40% to 92%.
We have incorporated rectangular collimation into our learning environment to provide more opportunity to practice and translate its use to dental clinics in Edmonton.
This study aims to obtain a better understanding of the reasons why rectangular collimation is not being used in private practice settings for intraoral imaging.
Participating in this study will involve
This study involves the completion of an online survey at Survey Monkey website. All that is required of you is to complete and submit the online blinded survey. If you choose to participate you do not have to answer every question if you choose not to. Since we will use Survey Monkey, you should know that while we will keep the information you give us confidential, in the United States under US privacy laws, the government has the right to access all information held in electronic databases.
Consent to Participate: Your consent is implied by completing and submitting the survey.
Possible Benefits
Although you will not see a direct benefit, your involvement in this study will inform the compliance on the use of rectangular collimation in private practices and may subsequently affect future radiation safety regulations. You will be impacting future offerings of training for students and dental care providers on how to implement the device in private practice when taking intraoral radiographs.
Possible Risks: There are no foreseeable risks involved in this study.
Confidentiality
These surveys are anonymous, as such there will be no personal information captured during your engagement with the research.
Voluntary Participation
Your participation in this study is voluntary. You are free to withdraw from the research study at any time during the data collection process (that is, up to the point you hit submit on your survey). There is no obligation on your part to continue and there is no penalty for withdrawing.
The plan for this study has been reviewed by a Research Ethics Board at the University of Alberta. If you have questions about your rights or how research should be conducted, you can call (780) 492-2615. This office is independent of the researchers.
If you have concerns about your rights as a study participant, you may contact the
| Research Principal Investigators | |
|---|---|
| Anthea Senior | Telephone: (780) 492-0464 |
| School of Dentistry | Email: senior@ualberta.ca |
| University of Alberta | |
| Camila Pacheco-Pereira | Telephone: (780) 248-1737 |
| School of Dentistry | Email: camila.pereira@ualberta.ca |
| University of Alberta | |
Thank you for your participation! Your input is extremely valuable and appreciated!
Appendix 2: The Questionnaire
*Denotes questions from the original survey by Lee and Ludlow 2013.11
- Demographics
Gender: Male or female
Select age range (years): 24–35; 36–47; 48–59; older than 59
Years in private practice: 0–5; 6–10; 11–20; 21–30; 31 and above
Dentist: Generalist or specialist - Communication with patients
- How often do you encounter patient questions about radiation safety?*
Always
Occasionally. If yes than select one: once per day, once per month, once per year.
Never discussed radiation risks with patients - How do you explain radiation risk/benefits to your patients?
Verbally – the staff explains
Verbally – the dentist explains
Written guidelines created by the practice
Comparison with day-by-day activities
Never explained - How often do you explain radiation risk/benefit to patients and acquire patient consent before taking radiographs?*
Sufficient
Sometimes
As requested by patients
None
- How often do you encounter patient questions about radiation safety?*
- Image receptor
- When taking intraoral images which receptor type do you use?*
Film
Digital. If this option is checked, select one: sensor or digital photostimulable phosphor (PSP) plates - What technique do you use for bitewings?
Tabs
Paralleling technique (using holder or not) - What technique do you use for periapicals?
Paralleling
Bisecting angle - How is the receptor held in the patient’s mouth during intraoral X-ray exposure?*
Patient’s finger
Parents finger
Staffs finger
Receptor holder (e.g., tabs, XCP, Snap-R-Ray) - Do you regularly use an aiming ring to help with aligning the tube head? (examples of aiming rings were provided)
Yes or no

- When taking intraoral images which receptor type do you use?*
- Rectangular collimation
- Do you regularly use a rectangular collimator during intraoral radiographic examinations? (examples of different types of collimators below)*
Yes or no


- Are you aware of the benefits of using rectangular collimation?
Yes or no - What challenges are preventing the implementation of using a rectangular collimator in your practice? (open question)
- Do you regularly use a rectangular collimator during intraoral radiographic examinations? (examples of different types of collimators below)*
We appreciate your participation!




