Abstract
Introduction:
Evidence-based practice (EBP) is an expectation of medical professionals and is positively received in the dental community. Investigations of evidence-based dentistry (EBD) have discussed its use in broad terms and daily clinical practice, but there is only limited information about its use and barriers with respect to particular dental specialities.
Methods:
A cross-sectional questionnaire was developed to survey implementation and obstacles to EBP; EBD specific to periodontics; and preferences for types of dissemination of evidence. The target population was active general dentists in Nova Scotia (n = 446). An email link to the questionnaire was distributed to dentists, and reminders were sent 4 and 10 days later.
Results:
The response rate was limited (16.6%). Most respondents were comfortable evaluating the growing body of research, although many reported use of low-level evidence, including that from other health professionals or expert opinion. A common barrier to use was insufficient time. Respondents who found strong evidence for certain periodontal procedures were more likely to refer these procedures, which included tissue regeneration and periodontics related to endodontics. On-site lecture-based dissemination was preferred by most respondents.
Conclusion:
General evidence-based concepts and use were similar to EBD results reported elsewhere, although external validity is limited by our low response rate and narrow target population. Specific data related to periodontics may be useful in directing a modified questionnaire to a broader target population. Respondents who are truly interested in EBD and responded to our questionnaire may ultimately benefit the most from our results, where further educational opportunities can be tailored to overcome the identified barriers and aid in more effective translation of evidence-based periodontal decisions in a general dental practice.
Introduction
The principles of evidence-based practice (EBP) reflect the core ethical values and conduct expected of dental professionals. Specifically, EBP is the integration of the clinician’s expertise, patient values and judicious use of current best evidence to guide clinical decision-making.1 This definition has been adopted by professional organizations such as the Canadian and American Dental Associations, and evidence-based dentistry (EBD) is a competency required of all graduating dentists.2,3 Attitude and intent toward EBP are generally positive, with self-reported use by general dentists at 32–88%; however, it is still underused to a large degree.4-9
Most dental programs have incorporated EBD into curricula; however, even with tools to critically appraise and apply knowledge from the literature, practitioners face a number of internal and external barriers to implementation.10-14 Many recent graduates report insufficient time to keep up with current research.6 Other clinician-centred barriers include reliance on personal experience, lack of knowledge to select the most appropriate articles and critically appraise the evidence and a perceived lack of applicability of research outcomes to their practice and patients.15,16 External barriers may be attributed to government health care factors focusing on cost efficiency and reimbursement and the influence of the dental industry on research projects and patient expectations.16 For example, as information is becoming increasingly more accessible and advertising infiltrates social media, patients may demand certain treatment modalities for which there may be limited evidence. Furthermore, the sheer volume of research material and access to the evidence is yet another external pressure contributing to the already difficult task of implementing an evidence-based clinical approach.13,17 As a result, general practitioners often rely on clinical expertise or information from colleagues, rather than sourcing and critically analyzing the constantly growing and potentially conflicting body of literature.6,14
There are many sources of primary research and research syntheses, such as systematic reviews and practice guidelines.12 However, for those not familiar with analyzing evidence, these sources may also be difficult to interpret and apply. A number of resources are accessible to guide a practitioner through the process of finding, evaluating and applying evidence from the literature,10,18-20 including the American Dental Association’s EBD Champion Program.21,22 In today’s digital world, several online initiatives are also available to facilitate the translation of research evidence into practice situations,13,23 including Canadian-developed ebhnow.com.24
A multifaceted, active learning approach is most likely to facilitate application of knowledge from clinical research.10,21,25 Involving practitioners in research through participatory means (practice-based research) may also be a solution to some of the barriers outlined above.15,17 This model creates data relevant to their practice and patients and potentially shortens the process from conception to adoption of research. Sampling a specific population of general dentists and tailoring continuing education to reflect their reported barriers may also be an effective method to simplify the EBD concept. The purpose of our research was to assess the extent of use, implementation and barriers to an EBP approach among a population of general dental practitioners in Nova Scotia, Canada, as it relates to the field of periodontics.
Materials and Methods
Questionnaire
A cross-sectional questionnaire was developed to assess implementation and obstacles to EBP; EBD specific to periodontics; and preferences for types of dissemination of evidence. The survey consisted of 27 questions formatted on Opinio (ObjectPlanet, Inc., Oslo, Norway); it was tested for face and content validity26 with a sample of 5 clinical and academic periodontists at Dalhousie University, Halifax, Canada.
The EBD implementation and obstacles section of the questionnaire was adapted from 2 sources: a survey distributed at the American Dental Association’s EBD Champion conference in 2008 by Spallek et al.9 and that of Straub-Morarend et al.6 A specific section related to periodontics, aimed at adding to the growing body of EBD evidence, included a range of topics that paralleled parameters of care and position papers available on the American Academy of Periodontics website.27
Questions included multiple choice (requiring single and multiple answers), matrix of choices, open-ended textboxes and comment/essay boxes. For questions that assessed frequency, a Likert-type scale with 5 categories was used: always, sometimes, occasionally, rarely, never. Open-ended “other” textboxes were available for most multiple-choice questions under the given choices.
Sample
A sample size calculation28 (using a 95% confidence level, with a margin of error of 5%) from a recruitment population of 446 licensed general dentists registered in Nova Scotia, resulted in a target sample size of 207. Recruitment was by emailed invitation distributed by the Nova Scotia Dental Association (NSDA) through its regular newsletter, Dispatch. Reminder emails were sent 4 and 10 days later, and access to the survey was closed following day 14. Responses were anonymous, as data were not linked with email or IP addresses. Consent was indicated by completing the survey. Participants could withdraw at any point throughout the survey. No reimbursements were given for participation.
Statistical Analyses
Statistical analysis was performed using SPSS v. 24. Descriptive statistics were used to summarize the data. χ2 tests were used to compare respondents’ referral behaviours based on their use of evidence and respondents’ depth of article-read based on their graduation cohort. Spearman correlation was used to assess the relationship between respondents’ number of courses attended and their reported use of EBD. A p value < 0.05 was considered statistically significant.
Ethics Approval
The Health Sciences Research Ethics Board at Dalhousie University granted ethics approval for the project (REB#2017-4254).
Results
Demographics
Of the 446 dentists invited by email, 74 completed the questionnaire, giving a final cumulative response rate of 16.6% (74/446). The number of respondents for each question varied, as participants were free to skip any questions they did not want to answer. The largest cohort by age was 25–34 (36.5%), with a similar number (36.1%) graduating in 2010 or later (Table 1).
|
|
Respondents |
|
|---|---|---|
| No. | % | |
| Age, years (n = 74) | ||
| 25–34 | 27 | 36.5 |
| 35–44 | 15 | 20.3 |
| 45–54 | 17 | 23.0 |
| 55–64 | 13 | 17.6 |
| 65+ | 2 | 2.7 |
| Gender (n = 74) | ||
| Male | 32 | 43.2 |
| Female | 38 | 51.4 |
| Not disclosed | 4 | 5.4 |
| Year of graduation (n = 72) | ||
| Before 1980 | 2 | 2.8 |
| 1980–1989 | 15 | 20.8 |
| 1990–1999 | 11 | 15.3 |
| 2000–2009 | 18 | 25.0 |
| 2010 or later | 26 | 36.1 |
| Practice profile (n = 73) | ||
| Solo practice | 19 | 26.0 |
| Community clinic/public health | 4 | 5.5 |
| Academia | 4 | 5.5 |
| Group practice | 48 | 65.8 |
| Associate or practice owner (n = 74) | ||
| Associate | 33 | 44.6 |
| Owner | 34 | 45.9 |
| Other | 7 | 9.5 |
Barriers to Applying Evidence
Most respondents were “somewhat comfortable” (56.2%) or “comfortable” (30.1%) when evaluating research studies for scientific validity, and most reported using evidence from clinical research in daily practice “occasionally” (24.7%) or “often” (52.1%). When asked about searching for an answer to a clinical question, 86.1% reported they were able to find the answer, although 41.7% questioned the validity or level of evidence.
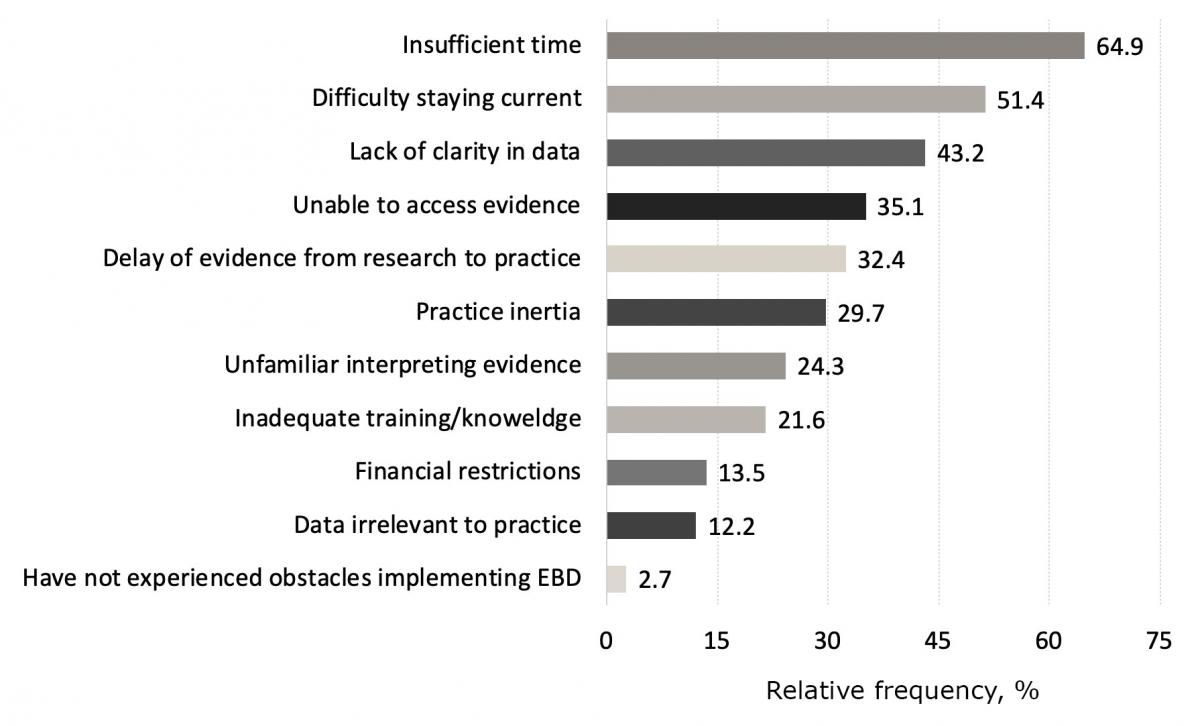
Barriers to EBD use included “insufficient time” (64.9%), “difficulty staying current” (51.1%) and “lack of clarity in research” (43.2%) (Fig. 1). Although 74.6% of respondents had access to online resources, 66.0% reported that they do not regularly use evidence-based resources.
Sources used in determining diagnosis and planning treatment included “experience and past knowledge” (94.5%), “another health professional” (82.2%) and “expert opinion” (63.0%). Synopses of research evidence (42.5%), research syntheses such as systematic reviews (31.51%) and original research studies (26.0%) were reported far less often (Table 2).
|
|
Relative frequency, % (no.) |
||||||
|---|---|---|---|---|---|---|---|
| Likelihood of accessing resources for a procedure not currently delivered (n = 73) |
Very likely | Somewhat likely | Unlikely | Very unlikely | N/A | Total | |
| Past experience | 47.7 (31) | 38.5 (25) | 4.6 (3) | 6.2 (4) | 3.1 (2) | 100 (65) | |
| Other health professionals | 59.2 (42) | 36.6 (26) | 1.4 (1) | 2.8 (2) | 0.0 (0) | 100 (71) | |
| Expert opinion | 49.3 (33) | 38.8 (26) | 6.0 (4) | 4.5 (3) | 1.5 (1) | 100 (67) | |
| Original research studies | 19.4 (12) | 33.9 (21) | 27.4 (17) | 19.4 (12) | 0.0 (0) | 100 (62) | |
| Clinical treatment guidelines | 52.2 (36) | 36.2 (25) | 7.3 (5) | 4.4 (3) | 0.0 (0) | 100 (69) | |
| Research syntheses | 23.4 (15) | 34.4 (22) | 28.1 (18) | 14.1 (9) | 0.0 (0) | 100 (64) | |
| Synopses of research evidence | 22.2 (14) | 42.9 (27) | 22.2 (14) | 12.7 (8) | 0.0 (0) | 100 (63) | |
| Manufacturer’s websites | 19.1 (12) | 41.3 (26) | 22.2 (14) | 17.5 (11) | 0.0 (0) | 100 (63) | |
| Textbooks | 27.9 (17) | 27.9 (17) | 18.0 (11) | 26.2 (16) | 0.0 (0) | 100 (61) | |
| Would not seek further information | 0.0 (0) | 2.2 (1) | 15.6 (7) | 60.0 (27) | 22.2 (10) | 100 (45) | |
| Other | 4.6 (1) | 0.0 (0) | 4.6 (1) | 0.0 (0) | 90.0 (20) | 100 (22) | |
| “I read the following dental/biomedical journals” (n = 73) |
Always | Often | Occasionally | Rarely | Never | N/A | Total |
| Journal of the Canadian Dental Association (JCDA.ca) | 29.6 (21) | 35.2 (25) | 22.5 (16) | 9.9 (7) | 1.4 (1) | 1.4 (1) | 100 (71) |
| Journal of Dental Research | 1.7 (1) | 18.3 (11) | 26.7 (16) | 23.3 (14) | 30.0 (18) | 0.0 (0) | 100 (60) |
| Journal of the American Dental Association | 8.2 (5) | 11.5 (7) | 31.2 (19) | 26.2 (16) | 21.3 (13) | 1.6 (1) | 100 (61) |
| Other | 16.0 (4) | 20.0 (5) | 12.0 (3) | 4.0 (1) | 28.0 (7) | 20.0 (5) | 100 (25) |
| Number of continuing education events attended in the past 12 months (n = 73) | 1–2 | 2–5 | 6–10 | >10 | N/A | Total | |
| Online courses | 34.3 (23) | 14.9 (10) | 9.0 (6) | 9.0 (6) | 32.8 (22) | 100 (67) | |
| On-site courses | 25.4 (18) | 43.7 (31) | 22.5 (16) | 7.0 (5) | 1.4 (1) | 100 (71) | |
| Journal clubs | 11.1 (6) | 1.9 (1) | 0.0 (0) | 0.0 (0) | 87.0 (47) | 100 (54) | |
| Study groups | 32.2 (19) | 15.3 (9) | 10.2 (6) | 3.4 (2) | 39.0 (23) | 100 (59) | |
| Other | 0.0 (0) | 10.5 (2) | 5.3 (1) | 10.5 (2) | 73.7 (14) | 100 (19) | |
The Journal of the Canadian Dental Association (JCDA.ca) was the most commonly read resource (97.2% of respondents), while the Journal of Dental Research and the Journal of the American Dental Association were read by 58.3% and 65.3% of respondents (Table 2).
When reading a scientific article, respondents focused mainly on conclusions (56.7%) or abstract only (42.0%), with 25.7% reading the article in its entirety. Graduates before 2000 were much more likely to read the abstract only (52.2%) than graduates since 2000 (26.9%) (χ2 = 4.32, df = 1, p = 0.032).
EBD Specific to Periodontics
In the past year, 63.5% of respondents attended continuing education (CE) related to periodontics, with 57.5% attending a course associated with surgical implantology and 44.7% for treatment planning and management of periodontal disease.
Periodontal surgical therapy was provided by 26.0% of all respondents. Among these responses, the most common in-office procedures were crown lengthening (84.2%), soft tissue grafting (47.4%) and surgical implantology (36.8%).
Most respondents (95.9%) referred at least 1 type of procedure to a periodontist. Soft tissue grafting was the most commonly referred procedure, while hard tissue grafting, tissue regeneration, crown lengthening and surgical implantology were frequently referred by 2 thirds of our respondents (Fig. 2). Over 2 thirds agreed that they found strong evidence to justify referrals for these same procedures (Fig. 3).
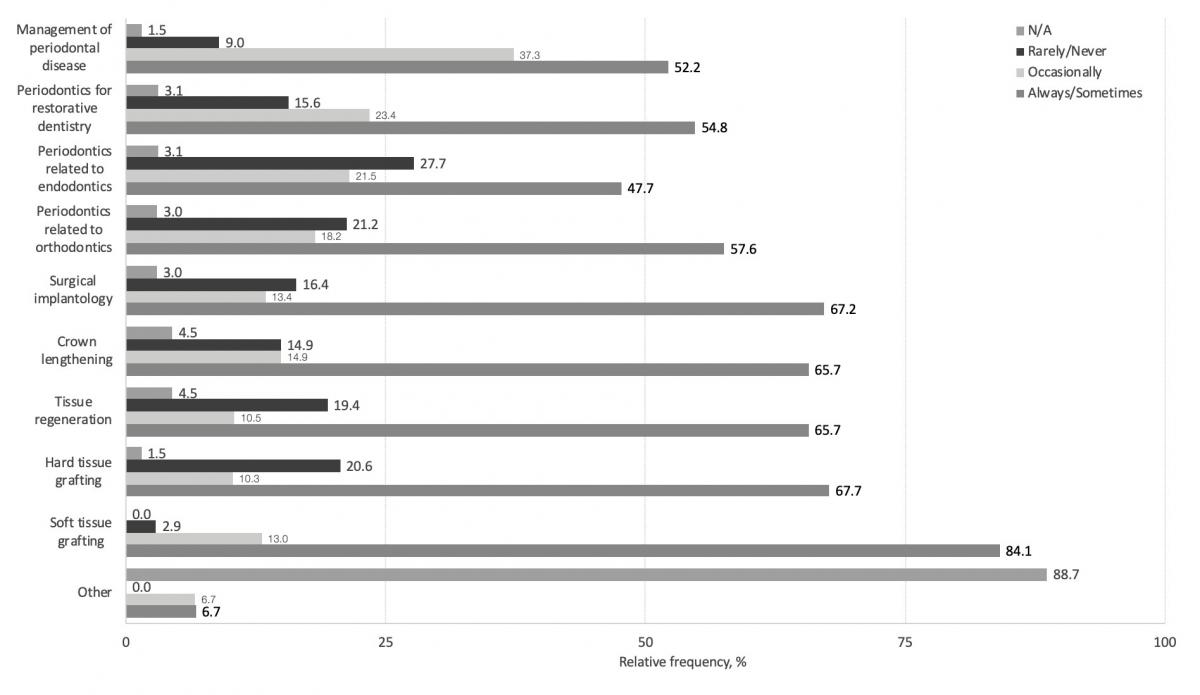
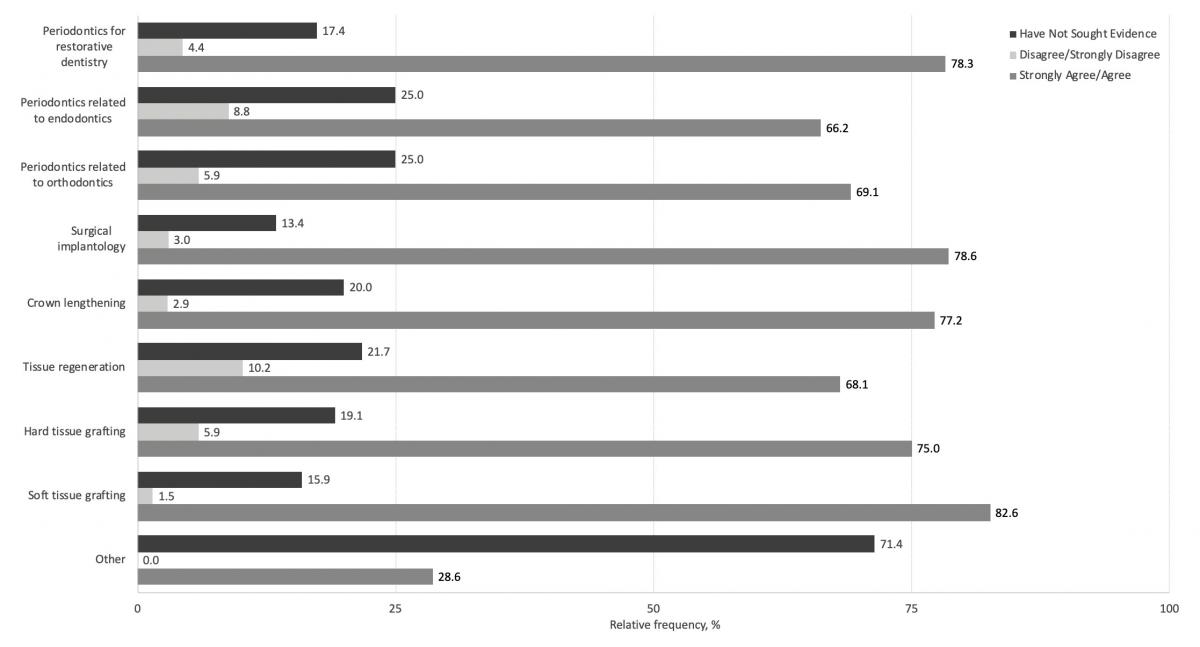
A comparison of procedures referred (Fig. 2) with level of agreement with evidence (Fig. 3) showed that respondents who reported being able to find strong evidence for certain procedures were more likely to refer these same procedures. These procedures included tissue regeneration (88.6% vs. 11.4%, χ2 = 11.44, df = 1, p = 0.001) and periodontics related to endodontics (85.0% vs. 15.0%, χ2 = 14.13, df = 1, p = 0.001); no significant differences were found for the other procedures.
With respect to CE opportunities, most respondents were interested in learning about periodontics related to restorative dentistry (62.5%). Other popular topics included treatment planning and management of periodontal disease (58.3%) and the relationship between systemic disease and periodontal disease (58.3%), followed by soft tissue grafting (48.6%) and surgical implantology (45.8%). No significant associations were found between the frequency of procedures referred and desired CE topics.
Methods of Dissemination of Evidence
The preferential delivery medium was on-site, lecture-based (84.9%), with 95% attending at least 1–2 events in the past 12 months. Online courses were attended by 67.2%, while study groups and journal clubs attracted 61.0% and 13.0%, respectively. There was no significant correlation between respondents use of EBD and the number of on-site courses attended (rs = 0.1, n = 71, p = 0.406).
Discussion
Our questionnaire was developed to determine barriers to using evidence-based periodontics in a target population of 446 general dentists, practising in Nova Scotia, Canada. The final response rate of 16.6% is at the lower end of the range of responses achieved in similar electronically distributed EBD questionnaires (16–41%).9,14,29 For privacy reasons, our survey was designed to collect anonymous responses; targeting non-responders was not possible, and no incentives were given to complete the questionnaire. In addition, the resources at the NSDA were unable to provide a mixed-mode distribution approach, which could have included other methods of questionnaire dissemination, such as distributing hard copies by traditional mail and/or sending recorded reminders by telephone. This approach of using multiple modes of dissemination may have been more effective.30 With a low participation rate, a non-response bias is likely. As a result, our findings may not be generalized to all dentists in Nova Scotia; however, we believe respondents to this survey may be more inclined to attend continuing education courses involving EBD. To our knowledge, this is the first collection of EBD data related to a specific dental specialty and may be useful in directing a modified questionnaire to a broader target population.
Our respondents reported that they “often” (52.1%) or “always” (15.1%) use evidence from clinical research in daily practice. This corresponds to habits of dentists in the European Regional Organization zone (32.1%),4 but is lower than those reported elsewhere.4,6,14 Although it is encouraging that such a large percentage of dentists report using an evidence-based approach in their daily practice, there is some difficulty in estimating the true frequency, as one may misinterpret familiarity with the concept of EBD as understanding.4,6 This point is illustrated by the majority of our sample using “other health professionals” or “expert opinion” when determining appropriate diagnosis and treatment, similar to other surveys where respondents favoured “other health professionals and colleagues” above “electronic library databases.”5,6 A higher level of evidence sources, such as systematic reviews and research synopses,19 was reported by fewer than half of our participants. In addition, most respondents reported that they have access to online evidence-based materials, but many do not regularly use these resources.
The most frequently reported barriers to EBD implementation reported in our questionnaire were in line with previous studies, with “insufficient time” being the primary obstacle.5,6,9,14 Although we did not find an association between age or graduation year and lack of time for implementation, we found that those who graduated before 2000 were much more likely to read the abstract section only. Other commonly reported barriers were those not under the clinician’s control.31 For example, the overwhelming amount of new evidence may create difficulties in staying current and may cloud data interpretation when conflicting results appear. Future CE should strive to summarize relevant evidence and target known topics of interest. For our sample, this included periodontics and restorative dentistry, treatment planning and management of periodontal disease and the relationship between systemic disease and periodontal disease.
A limited number of our respondents performed periodontal surgical therapy in their office, while nearly all referred at least 1 form of periodontal surgery to a periodontist. In terms of how comfortable respondents felt using an EBD approach to evaluate a patient for referral or treatment, a significant number indicated so for tissue regeneration and periodontics and endodontics. Other procedures not showing significance may be areas where general dentists feel exceptionally weak in searching for or evaluating the evidence and subsequently referring; this can be targeted for future knowledge translation.
Recent data further highlight the importance of a multifaceted and interactive approach.32 Kinesthetic learning or on-site, hands-on courses are likely to be well received. Use of technology, specifically social media distribution methods, allows for approachable and rapid dissemination of EBD.32,33 This is an area of unlimited potential, with the ability to connect practitioners in different regions at their convenience, while eliminating timely and costly in-person meetings and organizational logistics. Although our respondents favoured on-site learning over online courses, social media and online knowledge translation tools are in the early stages and should be explored in future EBD research.
Conclusions
It is clear that integration of patient needs, clinician’s experience and evidence is important to respondents, as nearly all reported some level of comfort in using an evidence-based approach on a daily basis. Regardless of whether this is true EBD understanding of what an EBP is, the overwhelmingly positive response indicates that this population might be open to tailored interventions.13 Although our small sample size was a major limitation, the data related to periodontics may be useful in directing a modified questionnaire to a broader target population. Those who are truly interested in EBD and responding to our questionnaire may ultimately benefit the most from our results. Creating a community of learners or a small group of EBD champions using these data may be the way forward.
THE AUTHORS
Correspondence to: Dr. Nader Hamdan, Dalhousie University, Faculty of Dentistry, 5981 University Ave., PO Box 15000, Halifax NS B3H 4R2. Email: nader.hamdan@dal.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- Sackett DL, Rosenberg WM, Gray JA, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312(7023):71-2.
- Accreditation standards for dental education programs (rev.). Chicago: Commission on Dental Accreditation; 2016.
- ACFD educational framework for the development of competency in dental programs. Winnipeg: Association of Canadian Faculties of Dentistry; 2016. Available from: https://acfd.ca/wp-content/uploads/ACFD-Educational-Framework-for-the-Development-of-Competency-in-Dental-Programs_2016.pdf
- Haron IM, Sabti MY, Omar R. Awareness, knowledge and practice of evidence‐based dentistry amongst dentists in Kuwait. Eur J Dent Educ. 2012;16(1):e47-52.
- Iqbal A, Glenny A-M. General dental practitioners’ knowledge of and attitudes towards evidence based practice. Br Dent J. 2002;193(10):587-91; discussion 583.
- Straub-Morarend CL, Marshall TA, Holmes DC, Finkelstein MW. Toward defining dentists’ evidence-based practice: influence of decade of dental school graduation and scope of practice on implementation and perceived obstacles. J Dent Educ. 2013;77(2):137-45.
- McColl A, Smith H, White P, Field J. General practitioners’ perceptions of the route to evidence based medicine: a questionnaire survey. BMJ. 1998;316(7128):361-5.
- Sabounchi SS, Nouri M, Erfani N, Houshmand B, Khoshnevisan M. Knowledge and attitude of dental faculty members towards evidence‐based dentistry in Iran. Eur J Dent Educ. 2013;17(3):127-37.
- Spallek H, Song M, Polk DE, Bekhuis T, Frantsve-Hawley J, Aravamudhan K. Barriers to implementing evidence-based clinical guidelines: a survey of early adopters. J Evid Based Dent Pract. 2010;10(4):195-206.
- Thomas A, Saroyan A, Dauphinee WD. Evidence-based practice: a review of theoretical assumptions and effectiveness of teaching and assessment interventions in health professions. Adv Health Sci Educ Theory Pract. 2011;16(2):253-76.
- Forrest JL. Treatment plan for integrating evidence-based decision making into dental education. J Evid Based Dent Pract. 2006;6(1):72-8.
- Boaz A, Baeza J, Fraser A, European Implementation Score Collaborative Group. Effective implementation of research into practice: an overview of systematic reviews of the health literature. BMC Res Notes. 2011;4:212.
- Grimshaw JM, Eccles MP, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50.
- Yamalik N, Nemli SK, Carrilho E, Dianiskova S, Melo P, Lella A, et al. Implementation of evidence‐based dentistry into practice: analysis of awareness, perceptions and attitudes of dentists in the World Dental Federation–European Regional Organization Zone. Int Dent J. 2015;65(3):127-45.
- Hopper L, Morris L, Tickle M. How primary care dentists perceive and are influenced by research. Community Dent Oral Epidemiol. 2011;39(2):97-104.
- Hannes K, Norré D, Goedhuys J, Naert I, Aertgeerts B. Obstacles to implementing evidence-based dentistry: a focus group-based study. J Dent Educ. 2008;72(6):736-44.
- Green LW. Making research relevant: if it is an evidence-based practice, where’s the practice-based evidence? Fam Pract. 2008;25(Suppl 1):i20-4.
- Somaraj V, Shenoy RP, Panchmal GS, Jodalli P, Sonde L. Evidence based dental practice: a review. J Appl Dental Med Sci. 2015;1(3):112-22.
- Sutherland SE. Evidence-based dentistry: Part I. Getting started. J Can Dent Assoc. 2001;67(4):204-6.
- Faggion Jr CM. The development of evidence-based guidelines in dentistry. J Dent Educ. 2013;77(2):124-36.
- Gillette J, Matthews JD, Frantsve-Hawley J, Weyant RJ. The benefits of evidence-based dentistry for the private dental office. Dent Clin North Am. 2009;53(1):33-45.
- Van Scoyoc SK. How to be a champion. J Evid Based Dent Pract. 2009;9(3):151-3.
- Afrashtehfar KI, Assery MK. From dental science to clinical practice: knowledge translation and evidence-based dentistry principles. Saudi Dent J. 2017;29(3):83-92.
- Catalogue. Montréal : Ebhnow.com; 2017. Available from: http://ebhnow.com/wp/applications/
- Schoonheim‐Klein M, Wesselink PR, Vervoorn JM. A community of learners in the evidence‐based dental clinic. Eur J Dent Educ. 2012;16(1):e174-9.
- Streiner DL, Norman GR, Cairney J. Health measurement scales: a practical guide to their development and use (5th ed.). Oxford, UK: Oxford University Press; 2015.
- AAP clinical and scientific papers. Chicago: American Academy of Periodontology; 2018. Available from: https://aap.onlinelibrary.wiley.com/doi/toc/10.1002/19433670.aap-clin-sci-papers
- Lerman, J. Study design in clinical research: sample size estimation and power analysis. Can J Anaesth 1996 Feb;43(2):184-91.
- Abdelkarim A, Sullivan D. Perspectives of dental students and faculty about evidence-based dental practice. J Evid Based Dent Pract. 2014;14(4):165-73.
- Patel AB, Matthews DC, Ghiabi E. Practice profile of periodontists in Canada: a national survey. J Can Dent Assoc. 2016;82:g5.
- Kao RT. The challenges of transferring evidence-based dentistry into practice. J Evid Based Dent Pract. 2006;6(1):125-8.
- Papakostopoulou M, Hurst D. Disseminating research evidence: what matters to general dental practitioners? Br Dent J. 2018;225(5):413-7.
- Puljak L. Using social media for knowledge translation, promotion of evidence‐based medicine and high‐quality information on health. J Evid Based Medicine. 2016;9(1):4-7.




