Abstract
Objective:
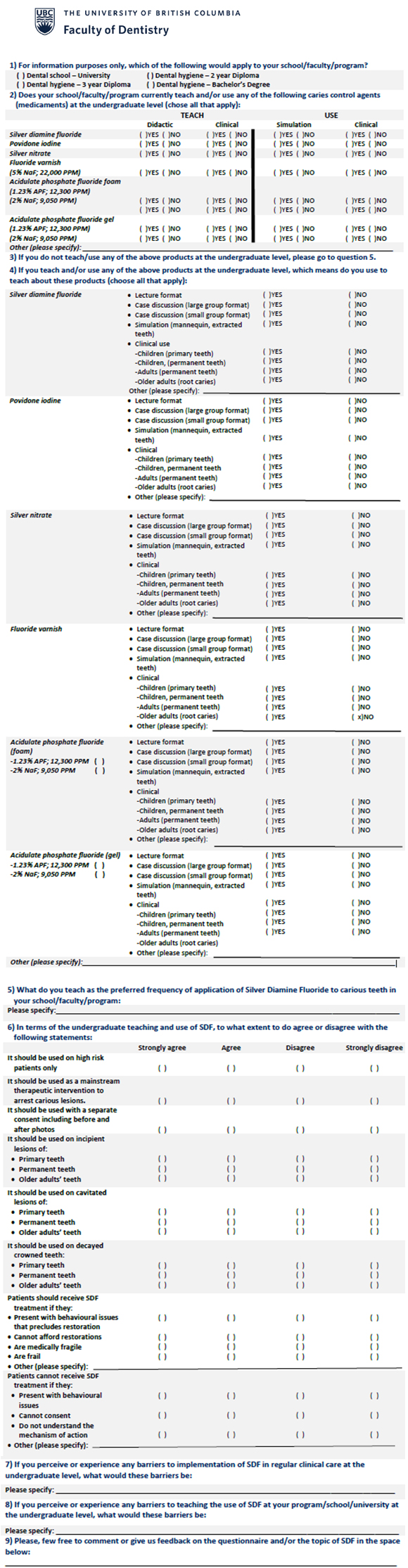
To investigate pedagogical approaches and perceived barriers to teaching about caries-control medications, particularly silver diamine fluoride (SDF), in Canadian undergraduate dental and dental hygiene programs. Methods: In summer 2018, a 9-item questionnaire was distributed to all 10 dental schools and 32 dental hygiene programs in Canada. It enquired about the types of caries-control medications used, teaching methods and perceived barriers to instruction on managing active caries with SDF.
Methods
In summer 2018, a 9-item questionnaire was distributed to all 10 dental schools and 32 dental hygiene programs in Canada. It enquired about the types of caries-control medications used, teaching methods and perceived barriers to instruction on managing active caries with SDF.
Results:
The response rate was 80% (n = 8) from dental schools and 72% (n = 23) from dental hygiene programs. All curricula included information about conventional caries-control medications: fluoride, silver nitrate and povidone iodine. In all programs, instruction regarding SDF was predominantly didactic: 93% of programs presented lectures on SDF and 30% of programs included clinical teaching and use of SDF in primary dentition only. The lack of consensus on clinical protocols outlining the number and frequency of SDF applications to arrest caries was cited by 43% of the programs as a barrier to clinical teaching.
Conclusions:
There is some variation across Canada in pedagogical approaches to caries-control medications and the inclusion of SDF in curricula. Poorly defined clinical protocols were reported as the main barrier to didactic and clinical use of SDF in undergraduate dental education programs.
Oral health has long been recognized as a basic human right.1 However, in Canada, oral health is excluded from the federally funded health care system and access is challenging for those who are economically disadvantaged.2-5 Complex surgical and restorative dental treatment of teeth affected by caries may be too costly for many. Instead, active carious lesions may be managed by promoting remineralization of affected enamel and dentin via non-surgical methods, including topical application of fluoride, silver nitrate and povidone iodine. In February 2017, silver diamine fluoride (SDF) was approved for use by Health Canada.4 SDF is a colourless solution of silver (25%), ammonia (8%), fluoride (5.5%) and water (62%) that has been demonstrated to arrest dental caries effectively. To date, most literature discusses its use in the primary dentition,4,6-12 with very few studies including adults and older adults with root caries.13,14
The current extent to which SDF has been integrated into routine clinical care in Canada is unknown. Recent reports have focused on its incorporation into the caries management curricula of United States dental schools.15,16 These studies suggest considerable variation, both in terms of the extent to which SDF is taught in undergraduate15 and graduate dental programs16 and of acceptable clinical protocols for its use.17,18 The amount of clinical and didactic instruction focused on SDF and other caries-control medications in Canadian dental programs is largely unknown.19 Educational institutions have traditionally been resistant to change when shifting from restorative and prosthetic procedures to more conservative, non-surgical and minimally invasive caries management methods.20,21
The objectives of this study were to investigate the teaching practices and perceived barriers to instruction on caries-control medications, particularly SDF, in Canadian dental and dental hygiene educational programs.
Methods
A non-systematic, yet comprehensive, literature search was initiated using the keywords “caries control” AND “silver diamine fluoride”, AND “education” on PubMED/Medline. The search was limited to full-text studies on humans published in English, Portuguese or Spanish (languages that the authors could understand) between 1970 and August 2018. A supplementary search for conference proceedings and graduate theses was undertaken using ProQuest and the same keywords. MS identified publications, screened them and excluded those failing to meet the search criteria based on the study objectives. Two pairs of independent researchers (MAB and CMCA; MS and IA) scrutinized the title, abstract and text of the selected publications and included those of relevance to the study. The researchers then met to discuss discrepancies until consensus was reached on which studies to include. Although the literature was searched comprehensively, this manuscript does not present a regular systematic review and meta-analysis for quality assessment given that there was no patient, intervention, comparison and outcome (PICO) question.
In all, 26 full-text articles were included based on their relevance to the study objectives, i.e., describing teaching pedagogies or methods pertaining to caries-control medications and instructions on SDF use. Of these, 12 reported on both didactic and clinical pedagogical approaches to the use of caries-control medications, including SDF. Some studies reviewed SDF instruction at the undergraduate level,22 while others focused on the graduate level.16 Two studies presented the clinical protocols used to apply SDF.17,22 Most studies mentioning SDF (22) were from the United States, 2 were from Canada,19,20 1 was from Australia and New Zealand23 and 1 was from Brazil.24 Based on these 26 studies, the use of caries-control medications is taught primarily via didactic methods, as a stand-alone subject or within a more robust course, usually restorative or operative dentistry or cariology. These methods include varying combinations of lectures, case presentations, problem-based learning, case studies, videos and undergraduate/graduate curricula. A few studies present a combination of didactic teaching on the application of SDF in a simulation environment (e.g., extracted teeth) or in a clinical care context involving patients, albeit mostly children.
Based on what we learned from the literature review pertaining to pedagogical approaches to teaching about caries-control medications, we developed a 9-item questionnaire in English only (Appendix), adapted from a 2016 study by Nelson et al.16 The questionnaire included identifying which medications were covered in the curricula and whether didactic instruction took place in lecture, seminar or simulation formats or together with clinical application of these substances. We also asked participants to describe any perceived barriers to teaching minimally invasive management of active lesion strategies using these caries-control medications, seeking information on SDF use in particular.
The questionnaire was pilot tested by 5 faculty members and graduate students to ensure clarity and comprehensiveness before it was sent to all 10 dental schools and 32 dental hygiene programs in Canada via an email attachment in the summer of 2018. We identified potential respondents by examining the websites of these programs; in addition, the questionnaire was sent to deans/directors and department heads with a request to forward it to an appropriate faculty member when no names were identified from their websites. After 2 weeks, a reminder email was sent to those programs and schools that had not responded. A third and final request was sent 4 weeks after the initial email.
Respondents could either complete the questionnaire as an MS Word document (Microsoft Corp., Redmond, Washington, USA) and email it back or print it out and fax it back. Only 1 response was collected for each institution; those with both undergraduate dental and dental hygiene programs counted as a single response. Descriptive analyses were completed to show the percentages and distribution of the responses.
Results
The response rate from Canadian dental schools was 80% (8 out of 10) and from Canadian dental hygiene programs 72% (23 out of 32). All schools and programs reported including the topic caries-control medications. The agents most commonly reported were fluoride varnish (92.3%), acidulated phosphate fluoride foam (88.5%), silver nitrate (26.9%) and povidone iodine (23.1%) with an even distribution between the schools and programs (Table 1). In terms of SDF, 1 dental school and 3 dental hygiene programs reported not addressing its use at all, either didactically or clinically in a formal course or module at the time the questionnaires were returned. Among dental schools and dental hygiene programs that taught the use of SDF, didactic formats varied widely and included lectures, case discussions, videos and problem-based learning (Table 1). Five of the dental schools reported teaching clinical use of SDF for children, while 2 also taught its clinical use in adults. Of the dental hygiene programs, 14 taught the clinical use of SDF for children, while only 1 did so for adult patients.
|
|
Teach, no. (%) |
Use, no. (%) |
||
|---|---|---|---|---|
|
Please note that the numbers may overlap because the same school/program may teach and/or use more than one product via different means (e.g., use in simulation and in clinic). |
||||
| Didactic | Clinical | Simulation | Clinical* | |
| Silver diamine fluoride | 23 (74.2) | 16 (51.6) | 11 (35.5) | 11 (35.5) |
| Povidone iodine | 6 (19.4) | 0 (0) | 0 (0) | 0 (0) |
| Silver nitrate | 7 (22.5) | 1 (3.2) | 1 (3.0) | 0 (0) |
| Fluoride varnish† | 24 (77.4) | 24 (77.4) | 10 (32.2) | 24 (74.4) |
| Acidulate phosphate fluoride foam‡ | 23 (74.2) | 7 (22.5) | 2 (6.5) | 5 (16.1) |
| Acidulate phosphate fluoride gel‡ | 25 (80.6) | 4 (13.0) | 9 (29.0) | 16 (51.6) |
The most commonly reported barriers to teaching about the use of SDF included lack of consensus on clinical guidelines in terms of the number and frequency of SDF applications needed to arrest caries (4 dental schools; 9 dental hygiene programs) and lack of training and experience using SDF (4 dental schools; 5 dental hygiene programs). Other barriers included lack of curriculum time, unclear patient benefits, heavy staining of caries by SDF, unclear reimbursement processes and lack of interest. Three respondents described lack of institution support — or a champion — for incorporating teaching of SDF across their curricula. About half of respondents from both the dental schools (n = 5) and the dental hygiene programs (n = 15) agreed or strongly agreed with the use of SDF as a mainstream therapy for all patients with active caries lesions, not just for high-risk individuals or children.
Discussion
This study reviewed the available literature on pedagogical approaches to caries-control medications, particularly SDF and then surveyed Canadian dental and dental hygiene programs on their teaching practices regarding caries control and perceived barriers to incorporating SDF into their curricula. The questionnaire had a return rate similar to other studies on the same topic, above 70%,15,16 which is much higher than the estimated 10% response rate for mailed out surveys.26
Other studies have also shown that the topic of caries-control medications has primarily been taught using didactic methods, ranging from lectures to videos and case studies, as we found herein; fewer studies have reported the clinical use of SDF when describing pedagogies, despite overwhelming evidence of safe, efficacious use of SDF as a minimally invasive topical agent to arrest active carious lesions.13,14 As highlighted by Fontana and colleagues,21 there is critical momentum to include non-surgical caries management in didactic and clinical approaches so that the traditional restorative and prosthetic methods can be contested,20 and risk-based caries management and personalized prevention may be more readily adopted.25
With the exception of fluoride varnish, our results showed that other medications were used at a higher rate than reported in the study that used the questionnaire on which ours was based16; however, that study involved a graduate program in pediatric dentistry. It found that 48.6% of programs used acidulated fluoride foam, 9.5% used silver nitrate and 1.3% used povidone iodine. These discrepancies might be because Nelson’s study16 focused on graduate programs only, and more specifically on clinical use of SDF, which was equally low in our study, in terms of didactic teaching (Table 1).
Both dental and dental hygiene programs reported that clinical use of SDF was predominantly focused on children (70%), which correlates with currently available literature. A lack of consensus on the frequency of application was listed as the main barrier to inclusion of SDF in teaching clinics. Other studies have also noted the lack of a widely accepted, evidence-based protocol for SDF as another barrier preventing its use clinically. This lack of evidence remains a major hurdle to the full adoption of this non-surgical dental caries treatment.21,23 Surprisingly, the black-staining side effect27 was not reported as a major barrier to clinical use, contrary to other studies.28,29 This might be because dark staining is frequently reported as influencing the acceptability of this treatment by patients,26 but does not necessarily influence how oral health care providers view its application.28,30
In addition, some respondents mentioned the lack of a champion to advocate the teaching of SDF as a barrier, particularly when there is a lack of institutional support. Champions have indeed been instrumental in the implementation of evidence-based dentistry31 and in prompting daily oral health care practice in long-term care homes.32,33 Similar to United States dental schools mentioned in a study by Ngoc and colleagues,15 most Canadian institutions varied in teaching involving SDF, while consistently focusing on its use to arrest coronal dental decay in primary teeth only. Weintraub et al.18 recently concluded that the existence of an easy-to-use protocol is a strong determinant of SDF uptake in clinical settings. In health care systems where basic dentistry remains unaffordable for many, as in Canada, the use of SDF as a mainstream procedure may fall within a dental public health mandate, leading to the need for robust undergraduate pedagogies aimed at sensitizing future dentists to a career focused on dental public health.34
The idea of promoting the widespread use of SDF is supported by the fact that most respondents (66%) from both dental schools and dental hygiene programs agreed or strongly agreed with its use as a mainstream therapy for all patients, regardless of age or socioeconomic status. As more studies emerge, SDF might indeed show evidence of arresting and preventing root and coronal caries in adults and older adults, as long as patients are well informed about the risks and benefits.35
The strengths of this study are related to its relatively high response rate. The limitations of the review method used to develop the questionnaire include the languages used to select the literature, which might have excluded studies in languages other than English, Spanish and Portuguese. The limitations of the questionnaire include its design and lengthy questions, response bias and potential recall bias among respondents. It also includes the potential for socially desirable responses, as respondents from the schools and programs might have felt pressured to participate in instances where they knew the researchers. Another limitation was the fact that the questionnaire was available only in English, and only 2 French-language institutions replied. In addition, some dental and dental hygiene programs are based at the same university and might have returned more than 1 questionnaire but were only counted as a single submission. As widely accepted and standardized evidence-based guidelines for the use of SDF and its evaluation must be further agreed on, follow-up studies should explore the extent to which dental professionals use SDF in their practices. Further studies should discuss the need to better align operative dentistry education with preventive dentistry education and should consider the inclusion of ways to teach proper SDF use for internationally trained dentists holding a licence to practise in Canada.
Conclusions
Dental education worldwide appears to have included the topic of caries-control medications, either as a stand-alone component of the curricula or as a topic within other disciplines, with some including the teaching of SDF use. Most Canadian dental and dental hygiene schools include caries-control medications in their curricula; however, the use of SDF is taught both didactically and clinically in fewer schools. Unclear guidelines are the main barrier preventing comprehensive teaching and use of SDF clinically. Widely accepted and standardized evidence-based guidelines for the use of SDF must be agreed on.
THE AUTHORS
Acknowledgements: The authors are thankful to all the Canadian dental schools and dental hygiene programs that participated in the survey. Financial support was received from Mitacs Canada to IA, and the National Council for Scientific and Technological Development and the Foundation for Research and Scientific and Technological Development of Maranhão to CMCA and to CCCR. A version of this manuscript was presented as a poster at the 98th International Association of Dental Research in Vancouver, Canada, on 21 June 2019, and at the Canadian Dental Association/Dentsply Sirona Student Clinician Research competition in Saskatoon, Canada, on 9 September 2019.
Corresponding author: Dr. Mario A. Brondani, Department of Community Dentistry and Prosthodontics and Dental Geriatrics, Faculty of Dentistry, University of British Columbia, 2199 Wesbrook Mall, Vancouver BC V6T 1Z3. Email: brondani@dentistry.ubc.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- van Palenstein Helderman W, Benzian H. Implementation of a basic package of oral care: towards a reorientation of dental NGOs and their volunteers. Int Dent J. 2006;56(1):44-8.
- Report on the findings of the oral health component of the Canadian Health Measures Survey 2007–2009. Ottawa: Health Canada; 2010. Available from: http://publications.gc.ca/site/eng/369649/publication.html
- Benjamin RM. Oral health: the silent epidemic. Public Health Rep. 2010:125(2):158-9.
- Yeung SST, Argáez C. Silver diamine fluoride for the prevention and arresting of dental caries or hypersensitivity: a review of clinical effectiveness, cost-effectiveness and guidelines. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2017. Available from: https://www.cadth.ca/sites/default/files/pdf/htis/2017/RC0903%20Silver%20Diamine%20Final.pdf
- The state of oral health in Canada. Ottawa: Canadian Dental Association; 2017. Available from: https://www.cda-adc.ca/stateoforalhealth/_files/TheStateofOralHealthinCanada.pdf
- Gao SS, Zhang S, Mei ML, Lo ECM, Chu CH. Caries remineralisation and arresting effect in children by professionally applied fluoride treatment — a systematic review. BMC Oral Health. 2016;16:12.
- Zhao IS, Gao SS, Hiraishi N, Burrow MF, Duangthip D, Mei ML, et al. Mechanisms of silver diamine fluoride on arresting caries: a literature review. Int Dent J. 2018;68(2):67-76.
- Horst JA. Silver fluoride as a treatment for dental caries. Adv Dent Res. 2018;29(1):135-40.
- Milgrom P, Horst JA, Ludwig S, Rothen M, Chaffee BW, Lyalina S, et al. Topical silver diamine fluoride for dental caries arrest in preschool children: a randomized controlled trial and microbiological analysis of caries associated microbes and resistance gene expression. J Dent. 2018;68:72-8.
- Gao SS, Zhao IS, Hiraishi N, Duangthip D, Mei ML, Lo ECM, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res. 2016;1(3):201-10.
- Monse B, Heinrich-Weltzien R, Mulder J, Holmgren C, van Palenstein Helderman WH. Caries preventive efficacy of silver diammine fluoride (SDF) and ART sealants in a school-based daily fluoride toothbrushing program in the Philippines. BMC Oral Health. 2012;12:52.
- Fung MHT, Duangthip D, Wong MCM, Lo ECM, Chu CH. Arresting dentine caries with different concentration and periodicity of silver diamine fluoride. JDR Clin Trans Res. 2016;1(2):143-52.
- Hendre AD, Taylor GW, Chávez EM, Hyde S. A systematic review of silver diamine fluoride: effectiveness and application in older adults. Gerodontology. 2017;34(4):411-9.
- McReynolds D, Duane B. Systematic review finds that silver diamine fluoride is effective for both root caries prevention and arrest in older adults. Evid Based Dent. 2018;19(2):46-7.
- Ngoc CN, Mehta R, Donovan TE, Ferreira Zandona AG. Teaching silver diamine fluoride in U.S. dental schools’ predoctoral curricula. J Dent Educ. 2018;82(12):1305-9.
- Nelson T, Scott JM, Crystal YO, Berg JH, Milgrom P. Silver diamine fluoride in pediatric dentistry training programs: survey of graduate program directors. Pediatr Dent. 2016;38(3):212-7.
- Burgette JM, Weintraub JA, Birken SA, Lewis TA, White BA. Development of a silver diamine fluoride protocol in safety net dental settings. J Dent Child (Chic). 2019;86(1):32-9.
- Weintraub JA, Birken SA, Burgette JM, Lewis TA, White BA. Use of the consolidated framework for implementation research to assess determinants of silver diamine fluoride implementation in safety net dental clinics. J Public Health Dent. 2019;79(4)298-306.
- Tikhonova S, Aggarwal N, Girard F. Cariology education in Canadian dental schools: interinstitutional symposium. J Can Dent Assoc. 2019;84:j9.
- Brown JP. A new curriculum framework for clinical prevention and population health, with a review of clinical caries prevention teaching in U.S. and Canadian dental schools. J Dent Educ. 2007;71(5):572-8.
- Fontana M, Guzmán-Armstrong S, Schenkel AB, Allen KL, Featherstone J, Goolsby S, et al. Development of a core curriculum framework in cariology for U.S. dental schools. J Dent Educ. 2016;80(6):705-20.
- Horst JA, Ellenikiotis H, Milgrom PL. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications and consent. J Calif Dent Assoc. 2016;44(1):16-28.
- Raphael SL, Foster Page LA, Hopcraft MS, Dennison PJ, Widmer RP, Evans RW. A survey of cariology teaching in Australia and New Zealand. BMC Med Educ. 2018;18(1):75.
- Ferreira-Nóbilo NdeP, Rosário de Sousa MdaL, Cury JA. Cariology in curriculum of Brazilian dental schools. Braz Dent J. 2014;25(4):265-70.
- Riley 3rd JL, Gordan VV, Ajmo CT, Bockman H, Jackson MB, Gilbert GH, et al. Dentists’ use of caries risk assessment and individualized caries prevention for their adult patients: findings from the Dental Practice-Based Research Network. Community Dent Oral Epidemiol. 2011;39(6):564-73.
- Fan W, Yan Z. Factors affecting response rates of the web survey: a systematic review. Comput Hum Behav. 2010;26(2):132-9.
- Patel J, Anthonappa RP, King NM. Evaluation of the staining potential of silver diamine fluoride: in vitro. Int J Paediatr Dent. 2018;28(5):514-22.
- Crystal YO, Janal MN, Hamilton DS, Niederman R. Parental perceptions and acceptance of silver diamine fluoride staining. J Am Dent Assoc. 2017;148(7):510-518.e4.
- Bagher SM, Sabbagh HJ, AlJohani SM, Alharbi G, Aldajani M, Elkhodary H. Parental acceptance of the utilization of silver diamine fluoride on their child’s primary and permanent teeth. Patient Prefer Adherence. 2019;13:829-35.
- Chhokar SK, Laughter L, Rowe DJ. Perceptions of registered dental hygienists in alternative practice regarding silver diamine fluoride. J Dent Hyg. 2017;91(4):53-60.
- Frantsve-Hawley J, Newman MG, Meyer DM. Proceedings of the Evidence-based Dentistry Champion Conference. Introduction. J Evid Based Dent Pract. 2008;8(3):113-4.
- Amerine C, Boyd L, Bowen DM, Neill K, Johnson T, Peterson T. Oral health champions in long-term care facilities-a pilot study. Spec Care Dentist. 2014;34(4):164-70.
- MacEntee MI, Thorne S, Kazanjian A. Conflicting priorities: oral health in long-term care. Spec Care Dentist. 1999;19(4):164-72.
- Brondani MA, Pattanaporn K, Aleksejuniene J. How can dental public health competencies be addressed at the undergraduate level? J Public Health Dent. 2015;75(1):49-57.
- Seifo N, Cassie H, Radford JR, Innes NPT. Silver diamine fluoride for managing carious lesions: an umbrella review. BMC Oral Health. 2019;19(1):145.
Appendix:
Questionnaire to explore teaching and use of caries-control medications in Canadian dental schools and dental hygiene programs.*