Abstract
Introduction:
Occupational characteristics of dental care — including closed environment, proximity to staff and patients and the use of aerosol-generating procedures — put workers at high risk of COVID-19 exposure and transmission. We describe the frequency of workplace situations that potentially increase the risk of exposure to COVID-19 in dental care compared with other occupations including health care.
Methods
We conducted a cross-sectional study using sociodemographic and occupational data from the 2016 Canadian census linked to workplace characteristics from the Occupational Information Network (O*NET) dataset. We assessed frequency of workplace indicators using an intensity score from 0 (low) to 100 (high) from O*NET on exposure to infection or disease, physical proximity to others, indoor controlled environments, standard protective equipment and specialized protective equipment.
Results:
In 2016, 87 815 Canadians worked in the 5 dentistry occupations of interest: dentists; denturists; dental hygienists and dental therapists; dental technologists, technicians and laboratory assistants; and dental assistants. These occupations were routinely ranked in the top 10 of all occupations examined in terms of exposure to workplace indicators that increase the risk of exposure to COVID-19. Dental hygienists and dental therapists, dental assistants, dentists and denturists, rank as the top 4 occupations, in that order, with the highest exposure to disease or infection and physical proximity to others combined.
Conclusions:
Compared with other occupations, dental care workers are at a higher risk of occupational exposure to COVID-19. These results support the development of workplace guidance to reduce the risk of COVID-19 transmission and enhance the well-being of the dental care workforce.
Occupational risk assessment is a method “for estimating health risks from exposure to various levels of a workplace hazard.”1 As workplace transmission was observed early in the COVID 19 pandemic,2 characterizing the role of the workplace in COVID-19 exposure and transmission became an important public health consideration. Agencies, including the World Health Organization,3 the Canadian Centre for Occupational Health and Safety4 and the Centers for Disease Control and Prevention (CDC),5 emphasize the importance of understanding the risk of exposure to and transmission of COVID-19 associated with varying occupations and implementing workplace safety or mitigation strategies accordingly.
Current evidence indicates that COVID-19 spreads primarily among people who come into close contact (≤ 2 m); transmission is via respiratory droplets generated when an infected person coughs, sneezes or talks.5 There is increasing evidence that transmission also occurs through aerosols and less evidence that surface transmission is a major route.6 Health care workers are considered to be at a higher risk of exposure to infectious diseases compared with other occupations. Their increased COVID-19 risk results from the provision of treatment, performing “essential” and other routine services for patients with COVID-19 and regular communication with staff and the public in a typical work day.7 In Canada, as of 23 July 2020, 19% (21 842) of all COVID-19 cases were among health care workers.8 A CDC data from 13 locations in the United States between 1 March and 31 May 2020 showed that health care workers accounted for 6% of adults admitted to hospital with COVID-19.9
Dental care workers face unique challenges in mitigating COVID-19 transmission when delivering care as they work in closed environments in close proximity to staff and patients and they conduct aerosol-generating procedures.10,11 COVID-19 outbreaks have been reported in dental offices in Canada,12-17 although none included provider-to-patient or patient-to-provider transmission. However, any time an outbreak is reported, it creates panic among dental workers, regulators and associations, and queries related to the nature and extent of the outbreak arise. This raises an important question: what is the risk of occupational exposure to COVID-19 in the dental care workforce compared with other occupations including health care?
Understanding the occupational characteristics that increase the risk of COVID-19 exposure and transmission would support the development of upstream prevention measures for the profession, both at the workplace (e.g., developing workplace policies, training dental staff about infection prevention) and regulatory levels (e.g., paid sick leave, compensation for exposure to hazard during a pandemic).7
Methods
Study Design and Sample Population
We conducted a cross-sectional study of employed people aged 15 and over who completed the long-form 2016 Canadian Census of Population. The long-form 2016 Census was completed by 25% of Canadian households and includes detailed information related to demographic, social and economic characteristics.18
For this study, Statistics Canada provided customized aggregate-level tables of data from the 2016 Canadian census, which included 18 497 145 labour force participants.18 The 2016 census classified occupation using the hierarchical National Occupational Classification (NOC) 2016 system. We identified occupations using the NOC 2016 4-digit unit group codes, representing the most specific occupational description available (n = 500).
Occupational characteristics of interest were provided by the publicly available Occupational Information Network (O*NET) database (v. 24.3; updated May 2020) developed by the United States Department of Labor/Employment and Training Administration.19 O*NET is a comprehensive database20 that includes characteristics (e.g., skills, knowledge and abilities) on 974 Standard Occupational Classification (SOC) occupations in the United States.21
Linking the 2016 Census to O*NET
Occupational characteristics from O*NET were mapped to occupations in the 2016 census using a publicly available “crosswalk” between occupational classifications systems from the United States (SOC)21 and Canada (NOC 2016), described elsewhere.22 This data linkage combines a rich set of population-representative occupation and sociodemographic data in Canada with comprehensive data on workplace indicators that increase risk of exposure to and transmission of COVID-19.
Complete O*NET information was available for 485 of 500 NOC 2016 4-digit occupations.
Occupational Characteristics
O*NET gathers information on occupational indicators through self-reported Likert-scale ratings in questionnaires administered to about 25 people in each SOC occupation.23 For each indicator, occupation-specific continuous weighted-average intensity scores, ranging from 0 to 100, are calculated.23
Recently, O*NET indicators have been used to describe occupational characteristics related to COVID-19 risk in the United States and the United Kingdom.24-27 Based on the existing literature and established COVID-19 risk factors, such as close physical contact, aerosol transmission in indoor settings and accessibility of personal protective equipment (PPE),10,11,24-28 5 O*NET indicators were selected for this study. For each of these, the specific questions asked and derived continuous weighted-average intensity scores were as follows.
Frequency by which workers are exposed to diseases or infections: Based on the question “How often does this job require exposure to disease/infections?” intensity scores were: 0 = never exposed, 25 = once a year, 50 = once a month, 75 = once a week, 100 = every day.
Physical proximity to other workers in a typical workday: Based on the question “How physically close to other people are you when you perform your current job?” intensity scores were: 0 = do not work near people, 25 = work with others, but not closely, 50 = slightly close, e.g., shared office, 75 = moderately close, e.g., arm’s length, 100 = very close, e.g., near touching.
Indoors, environmentally controlled: Based on the question “How often does this job require working indoors in environmentally controlled conditions?” intensity scores were: 0 = never, 25 = once a year, 50 = once a month, 75 = once a week, 100 = every day.
Wear common protective or safety equipment: Based on the question “How much does this job require wearing common protective or safety equipment?” intensity scores were: 0 = never, 25 = once a year, 50 = once a month, 75 = once a week, 100 = every day.
Wear specialized protective or safety equipment: Based on the question “How much does this job require wearing specialized protective or safety equipment, such as breathing apparatus, safety harness, full protection suits or radiation protection?” intensity scores were: 0 = never, 25 = once a year, 50 = once a month, 75 = once a week, 100 = every day.
In addition, ability to work from home (yes/no) was assessed given its potential for reducing an occupation’s risk of COVID-19 infection transmission. Ability to work from home was derived for SOC occupations from Dingel & Nieman’s white paper,29 by applying cut-offs to ordinal responses for 17 O*NET indicators related to work context and activities.
Dental Occupations
Dental care workers were defined as those working in the following NOC 2016 4-digit occupations: 3113 dentists; 3221 denturists; 3222 dental hygienists and dental therapists; 3223 dental technologists, technicians and laboratory assistants; and 3411 dental assistants. In total, 87 815 individuals worked in dentistry occupations of interest.
Sociodemographic Characteristics
Characteristics for each dentistry NOC 2016 4-digit occupation included median employment income (2015 Canadian dollars [CAD]) and aggregate counts for the total number of workers and across sociodemographic information, including age (15–24, 25–34, 35–44, 45–54, 55–64, 65+ years); sex (male/female); immigrant status (non-immigrant, immigrant, non-permanent residents); household income adequacy quintiles; and visible minority status as proxy for race/ethnicity (Visible minority total, South Asian, East Asian, Black, Southeast Asian, Middle Eastern, Latin American, Visible minority included elsewhere, Multiple visible minorities, Non-visible minority).
Statistical Analysis
Demographic characteristics of the 5 dental occupations (n = 87 815) were assessed descriptively using univariate analysis. For each O*NET indicator, we identified the top 10 occupations (n = 485) based on their respective scores. The O*NET scores of all dental occupations, irrespective of representing the top 10 occupations for the O*NET indicator, were assessed and presented. A cross-tabulation for the 2 most relevant indicators — exposure to infection/disease and physical proximity to others — was conducted to calculate an average score to assess which occupations are at the highest risk of exposure to COVID-19 because of the nature of the occupation.
Results
Occupational exposure and sociodemographic information about the 5 dental occupations are presented in Table 1. In 2016, of the 87 815 Canadians who worked in the 5 dentistry occupations of interest, most identified as dental assistants (n = 34 160), dental hygienists/therapists (n = 26 645) and dentists (n = 18 930). Compared with other dentistry occupations, a higher proportion of workers age ≥ 65 years were found among dentists (10%) and denturists (11%). Women were overrepresented in dental hygienist/therapist (98%) and dental assistant occupations (99%), but underrepresented in the other dentistry occupations, e.g., dentists (39%). The representation of immigrants in dental occupations varied from 16% among dental hygienists/therapists to 52% among dental technologists, technicians and laboratory assistants. Moreover, the proportion of people in dental occupations who were in the lowest household income quintile varied from 4% of dentists to 21% of dental technologists, technicians and laboratory assistants. Based on 2015 figures, dentists had the highest median income of the 5 occupations. Visible minority groups were prominent among dental technologists, technicians and laboratory assistants (37%) as well as dentists (35%). Workers who identified as East Asian, South Asian, Southeast Asian, and Middle Eastern were the most prominent visible minority groups in all dentistry occupations.
|
Characteristic |
Dentists |
Denturists |
Dental hygienists/dental therapists |
Dental technologists, technicians and laboratory assistants |
Dental assistants |
|---|---|---|---|---|---|
|
Note: Counts, proportions and income information are from the 2016 Canadian census. The Brookfield crosswalk23 was used to map O*NET indicators to National Occupational Classification codes used in the 2016 census. |
|||||
| Female, % | 39 | 35 | 98 | 44 | 99 |
| ≥ 65 years, % | 10 | 11 | 1 | 6 | 1 |
| Immigrant or non-permanent resident, % | 39 | 21 | 17 | 54 | 26 |
| Lowest household income quintile, % | 4 | 13 | 8 | 21 | 17 |
| Visible minority, % South Asian, % East Asian, % Black, % Southeast Asian, % Middle Eastern, % Latin American, % Other or multiple visible minority, % |
35 9 13 1 4 7 1 1 |
15 1 6 1 4 2 1 1 |
16 4 3 2 3 2 1 1 |
37 2 19 1 8 3 3 1 |
22 4 4 2 6 2 2 1 |
| Median income, 2015 CAD | 98 582 | 46 722 | 49 305 | 42 113 | 34 420 |
| O*Net indicators Able to work from home Physical proximity Exposed to disease or infections Indoors environmentally controlled Wear specialized protective equipment Wear common protective equipment |
No 99 94 94 52 91 |
No 99 94 94 52 91 |
No 100 100 97 14 100 |
No 52 72 97 16 93 |
No 99 96 92 38 100 |
None of the 5 dental occupations allow the ability to work from home. Apart from dental technologists, technicians and laboratory assistants, dentistry occupations ranked high for all O*NET indicators except for “Wear specialized protective or safety equipment.” Dental technologists, technicians and laboratory assistants ranked high for 2 indicators: “Wear common protective or safety equipment” and “Indoors, environmentally controlled.”
O*NET scores for the top 10 occupations in terms of risk of exposure to COVID-19 at work for each relevant indicator are presented in Table 2.
|
O*NET indicator |
O*NET score |
|---|---|
|
Note: Where >10 occupations had similar scores, all occupations are listed. |
|
| Frequency with which workers are exposed to diseases or infections 3112 General practitioners and family physicians 3222 Dental hygienists and dental therapists 3214 Respiratory therapists, clinical perfusionists and cardiopulmonary technologists 3411 Dental assistants 3113 Dentists 3221 Denturists 3233 Licensed practical nurses 3215 Medical radiation technologists 3114 Veterinarians 3234 Paramedical occupations |
100 100 98 96 94 94 94 92 89 89 |
| Physical proximity to other workers in a typical workday 3142 Physiotherapists 3222 Dental hygienists and dental therapists 3113 Dentists 3221 Denturists 3411 Dental assistants 5134 Dancers 3217 Cardiology technologists and electrophysiological diagnostic technologists, n.e.c. 3234 Paramedical occupations 3122 Chiropractors 6522 Pursers and flight attendants |
100 100 99 99 99 98 97 97 96 96 |
| Indoors, environmentally controlled 1511 Mail, postal and related workers 3131 Pharmacists 4112 Lawyers and Quebec notaries 4166 Education policy researchers, consultants and program officers 6222 Retail and wholesale buyers 6311 Food service supervisors 6331 Butchers, meat cutters and fishmongers - retail and wholesale 9462 Industrial butchers and meat cutters, poultry preparers and related workers 2252 Industrial designers 3122 Chiropractors 4111 Judges 5224 Broadcast technicians |
100 100 100 100 100 100 100 100 99 99 99 99 |
| Wear common protective or safety equipment 3222 Dental hygienists and dental therapists 3411 Dental assistants 6621 Service station attendants 7232 Tool and die makers 7252 Steamfitters, pipefitters and sprinkler system installers 7253 Gas fitters 7312 Heavy-duty equipment mechanics 7318 Elevator constructors and mechanics 7531 Railway yard and track maintenance workers 7532 Water transport deck and engine room crew 7621 Public works and maintenance labourers 7622 Railway and motor transport labourers 8411 Underground mine service and support workers 8412 Oil and gas well drilling and related workers and services operators 8614 Mine labourers 8615 Oil and gas drilling, servicing and related labourers 9231 Central control and process operators, mineral and metal processing 9411 Machine operators, mineral and metal processing 9412 Foundry workers 9421 Chemical plant machine operators 9431 Sawmill machine operators |
100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 100 |
| Wear specialized protective or safety equipment 7322 Motor vehicle body repairers 7244 Electrical power line and cable workers 7293 Insulators 8232 Oil and gas well drillers, servicers, testers and related workers 8412 Oil and gas well drilling and related workers and services operators 9231 Central control and process operators, mineral and metal processing 9411 Machine operators, mineral and metal processing 3215 Medical radiation technologists 4312 Firefighters 7236 Ironworkers |
91 86 83 81 76 76 76 75 74 74 |
Frequency with which workers are exposed to diseases or infections: O*NET scores for the 10 most exposed occupations ranged from 89 to 100; these were all in health care including 4 dental occupations. The only dental occupation not in the top 10 was dental technologists, technicians and laboratory assistants, which scored 72. These scores are interpreted to mean that dental hygienists/therapists, dental assistants, dentists and denturists are all exposed to disease or infection almost every day, whereas dental technologists, technicians and laboratory assistants are exposed at least once a week.
Physical proximity to other workers in a typical workday: Of the top 10 occupations that require working in close physical proximity to others, 8 were in health care, including 4 dental occupations. O*NET scores were 96–100 for the top 10; dental technologists, technicians and laboratory assistants, who were not in the top 10, scored 52. Therefore, dentists, dental hygienists/therapists, dental assistants and denturists nearly touch other individuals during their routine work, and dental technologists, technicians and laboratory assistants work only slightly close to others as they share office space.
Indoors, environmentally controlled: The top 10 occupations who work indoors in a controlled environment include only 2 in health care (pharmacists and chiropractors) and none in a dental occupation. The O*NET scores for these occupations were 99–100; dental occupations scored 97 for dental hygienists/therapists and for dental technologists, technicians and laboratory assistants; 94 for dentists and denturists; and 92 for dental assistants. From the frequency perspective, the O*NET scores indicate that dental occupations work in environmentally controlled indoors almost all (if not all) days.
Wear common protective or safety equipment: Because 21 occupations reported wearing common protective equipment at all times in the workplace, an O*NET score of 100, all have been included in the table. Dental hygienists/therapists and dental assistants were the only 2 dental occupations among them. Dental technologists, technicians and laboratory assistants scored 93, and dentists and denturists both scored 91. These scores indicate that dental technologists, technicians and laboratory assistants, dentists and denturists wear common protective or safety equipment at almost all (if not all) times.
Wear specialized protective or safety equipment: Among the top 10 occupations, the only health care workers who wear specialized protective safety equipment are medical radiation technologists. O*NET scores for the top 10 ranged from 74 to 91. The 5 dental occupations scored 52 for dentists and denturists, 38 for dental assistants, 16 for dental technologists, technicians and laboratory assistants and 14 for dental hygienists/therapists. This means that dentists and denturists wear specialized protective equipment almost once a month, dental assistants a few times in a year and dental technologists, technicians and laboratory assistants and dental hygienists/therapists very rarely.
A bubble plot of all occupations (Figure 1) shows average O*NET scores for the 2 most prominent indicators: exposure to disease or infection and physical proximity to others in a typical workday. Of the 10 occupations with high scores for both indicators (upper right of the graph), all are in the health care sector, and dental hygienists/therapists (100), dental assistants (97.5), dentists (96.5) and denturists (96.5) rank as the top 4.
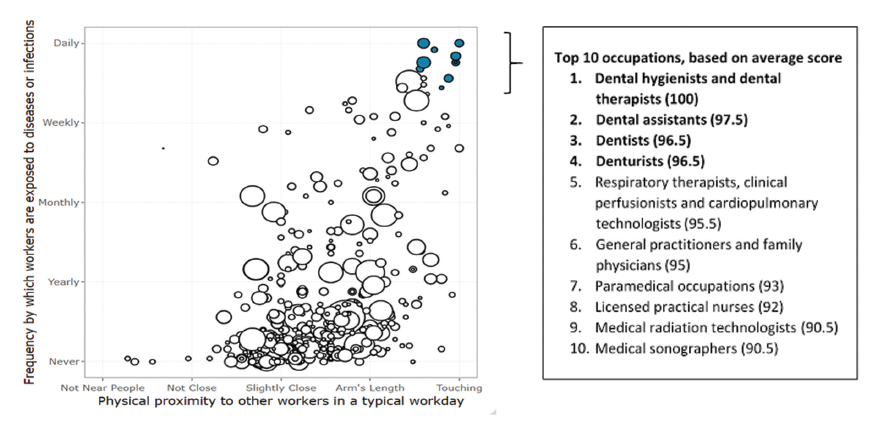
Figure 1: Average Occupational Information Network scores for National Occupational Classification (NOC) 2016 occupations (n = 485) by physical proximity to others in a typical workday versus frequency with which workers are exposed to diseases or infections. The size of each “bubble” reflects the number of individuals working in that occupation (2016 census). Filled bubbles highlight occupations with the highest average score, and these are listed in descending order above.
Discussion and Conclusion
This is the first study to attempt to assess the occupational characteristics that increase risk of exposure and transmission of COVID-19 in the dental care workforce compared with other occupations including health care. Based on O*NET indicators, our study suggests that dental care workers have potentially high occupational risk of such exposure and transmission. In particular, this risk relates to working in close physical proximity to others and a high frequency of exposure to disease or infection. Dental care workers had similar occupational risk of exposure to COVID-19 as some other health care occupations and, on average, higher risk compared with non-health care occupations in Canada.
Although no patient-to-provider or provider-to-patient infection transmission cases have been reported in dental settings in Canada, it is important to acknowledge the potential for underreporting of patient acquisition of COVID-19 infection in dental offices; because symptoms may present only 2–14 days later, patients could have multiple exposures during that time making it difficult to identify specific sources. As such, the high O*NET scores observed among dental care workers for indicators, such as working in close proximity to others and exposure to infection/disease are, in a way, validated through multiple dental office outbreaks reported in the media, which were mainly among staff.12-17 Overall, our purpose is not to scare the dental community but rather provide data to allow better understanding of workplace characteristics that can increase risk of infection transmission. Attention has focused on how to prevent infection transmission during aerosol generating procedures, but only limited information is available on how staff communicate during off hours or in a staff room. This study will support dental professionals in targeting COVID-19 infection transmission prevention in their offices more comprehensively.
In general, dental care workers do take utmost precautions during dental care delivery to prevent infection. This is evident from our findings that dental workers report using standard protection almost every day to at all times. None of the dental professions was in the top 10 occupations for wearing specialized protective equipment; this is understandable, as specialized protective gear is not required when providing standard care. Currently, specialized protective equipment in dental care occupations is only recommended under special circumstances, for example, when providing care to a patient with a highly infectious disease, such as COVID-19. Throughout the COVID-19 pandemic, the use of non-routine protective equipment, such as N95 respirators, American Society for Testing and Materials level 3 face masks, face shields, safety goggles and protective gowns, has been recommended, based on point-of-care risk assessment, while providing dental care.11 Familiarity with specialized protective equipment may have reduced COVID-19 outbreaks in dental care settings despite the increased occupational risk of exposure to COVID-19.
Throughout the COVID-19 pandemic, the importance of heating, ventilation and air conditioning (HVAC) systems in dental care settings has been boldly underscored. Efficient HVAC systems in a dental operatory are directly linked to the time required to remove aerosol from the area after a procedure. With understanding that dental professionals are at the highest risk of exposure to COVID-19, not only because of conducting aerosol-generating procedures, but also because of other factors identified in this study (i.e., high exposure to disease or infections and working in close proximity to others), it becomes all the more important that they always work in controlled environments. However, results show that dental workers do work in a controlled environment almost every day; thus, inbuilt HVAC systems may not be sufficient to provide the desired indoor environment, especially in older constructions, and supplementary means, such as portable filters, might have to be employed.30
We found that dental technologists, technicians and laboratory assistants do not share the same high level of risk exposure as other dental workers. This may be because technicians work in laboratory settings and, therefore, have no physical contact with patients, have fewer interactions with other staff and are not exposed to infection directly. That said, a systematic review of cross-infection control in dental laboratories highlighted flaws in cross-infection control procedures and disinfection strategies and recommended improved training in disinfection in such settings.31
Another factor that is crucial in terms of controlling infection transmission is “presenteeism,” where employees are present at work despite having a sickness that justifies their absence and, as a result, are working under suboptimal conditions, which can be harmful to themselves and others.32 Our results show that no workers in the 5 dental occupations have the ability to work from home. Health care workers, including those in dentistry, are essential skilled workers. The limited availability of substitute workers is exacerbated during COVID-19; therefore, one may expect more presenteeism and, thus, more transmission of infection. This observation calls for cost-effective workplace interventions to reduce dental care worker presenteeism while maintaining a sustainable workforce.33
Some limitations identified in this work include acknowledgement that risk of exposure to COVID-19 at work measured through O*NET scores is based on typical job characteristics and activities within occupations, not a measure of association based on COVID-19 cases or COVID-19 transmission. Also, workplace exposure indicators were assessed before the COVID-19 pandemic and do not account for changes in workplace policies and/or infection mitigating strategies instituted during the pandemic, e.g., additional environmental controls, specialized personal protective equipment, maintaining physical distance.
In addition, the O*NET database is designed and maintained in the United States. Although, it is a common assumption that job characteristics, such as skills, knowledge and abilities, are generalizable to the Canadian workforce, practices such as frequency of wearing common protective or safety equipment might differ. A similar survey among Canadian dental workers would be useful for making more certain assessments. In addition, the O*NET scores are based on self-reported data, which can be subject to response bias. Misclassification of occupations can also occur for those who are engaged in more than 1 occupation, but we assume that such numbers would be very low.
This analysis has several strengths. It was the first to specifically quantify the intensity of occupational characteristics that potentially increase the risk of exposure and transmission of COVID-19 in dental care workers and objectively compare them with other occupations. These indicators fill an important information gap regarding the lack of COVID-19 data by occupation in Ontario. The study includes the latest census data from Statistics Canada, which provide reliable and comprehensive population-based Canadian information on specific occupations. In terms of assessing occupational risk indicators, O*NET scores were used, which cover working conditions that are derived from survey responses from large, representative samples of workers.
Overall, the results of this study suggest that dental care workers are at a higher risk of exposure to COVID-19 at work than those in other occupations. In addition, the study also identifies opportunities where dental care workers have the potential to improve their work practices to further mitigate the risk of infectious disease transmission. The results of this study will be helpful to administrators and regulators in developing workplace guidance to not only reduce infection transmission but also ensure well-being of the dental care workforce.
THE AUTHORS
Corresponding author: Dr. Sonica Singhal, Public Health Dentist, Health Promotion, Chronic Disease, and Injury Prevention Dept., Public Health Ontario, 480 University Avenue, Toronto, ON M5G 1X8. Email: sonica.singhal@mail.utoronto.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- Occupational risk assessment. Washington, DC: National Institute for Occupational Safety and Health; 2017. Available: https://www.cdc.gov/niosh/topics/riskassessment/default.html (accessed 2021 Apr. 21).
- Koh D. Occupational risks for COVID-19 infection. Occu Med (Lond). 2020;70(1):3-5.
- Coronavirus disease (COVID-19): health and safety in the workplace. Geneva: World Health Organization; 2020. Available: https://www.who.int/news-room/q-a-detail/coronavirus-disease-covid-19-health-and-safety-in-the-workplace (accessed 2020 Dec. 15).
- Reducing COVID-19 risk in community settings: a tool for operators. Ottawa: Government of Canada; 2021. Available: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/risk-informed-decision-making-workplaces-businesses-covid-19-pandemic.html (accessed 2021 Jul. 25).
- Managing healthcare operations during COVID-19. Atlanta: Centers for Disease Control and Prevention; 2021. Available: https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html (accessed 2021 Jul. 25).
- Greenhalgh T, Jimenez JL, Prather KA, Tufekci Z, Fisman D, Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021;397(10285):1603-5.
- Michaels D, Wagner GR. Occupational Safety and Health Administration (OSHA) and worker safety during the COVID-19 pandemic. JAMA. 2020;13;324(14):1389-90.
- COVID-19 cases and deaths among health care workers in Canada. Ottawa: Canadian Institute for Health Information; 2021. Available: https://www.cihi.ca/en/covid-19-cases-and-deaths-among-health-care-workers-in-canada (accessed 2020 Dec 15).
- Kambhampati AK, O’Halloran AC, Whitaker M, Magill SS, Chea N, Chai SJ, et al. COVID-19-associated hospitalizations among health care personnel — COVID-NET, 13 states, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1576-83.
- COVID-19 in dental care settings. Toronto: Public Health Ontario; 2020. Available: https://www.publichealthontario.ca/-/media/documents/ncov/ipac/2020/07/covid-19-dental-care-settings.pdf?la=en (accessed 2021 Jul. 25).
- Guidance for dental settings: interim infection prevention and control guidance for dental settings during the coronavirus disease 2019 (COVID-19) pandemic. Atlanta: Centers for Disease Control and Prevention; 2020. Available: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed 2020 Dec. 15).
- Mazur A. Public health warns of COVID-19 exposure at Trenton dentist’s office. Global News. 2020;14 Oct. Available: https://globalnews.ca/news/7396068/public-health-covid-19-exposure-trenton-dentist/ (accessed 2021 Jul. 25).
- Louis A. FNHA announces COVID-19 exposure at Seabird Island Dental Clinic. Chilliwack Progress. 2020;19 Oct. Available: https://www.theprogress.com/news/fnha-announces-covid-19-exposure-at-seabird-island-dental-clinic/
- Banger C. COVID-19 outbreak declared at Waterloo Region dental service; region reports 20 new cases. CTVNews. 2020;16 Oct. Available: https://kitchener.ctvnews.ca/covid-19-outbreak-declared-at-waterloo-region-dental-service-region-reports-20-new-cases-1.5144674 (accessed 2021 Jul. 25).
- Clarke K. Hamilton surpasses 500 active COVID cases. Hamilton Spectator 2020;30 Nov. Available: https://www.thespec.com/news/hamilton-region/2020/11/29/covid-hamilton-latest-news.html (accessed 2021 Jul. 25).
- Baker JK. 84 new cases of COVID-19 in Waterloo Region, one more death. CTV News. 2020;19 Dec. Available: https://kitchener.ctvnews.ca/84-new-cases-of-covid-19-in-waterloo-region-one-more-death-1.5238975 (accessed 2021 Jul. 25).
- COVID-19 outbreak declared at Pembroke, Ont., dental office. CBC News. 2020;30 Dec. Available: https://www.cbc.ca/news/canada/ottawa/pembroke-dentist-office-outbreak-covid-1.5849471 (accessed 2021 Jul. 25).
- Census program. Ottawa: Statistics Canada; 2021. Available: https://www12.statcan.gc.ca/census-recensement/index-eng.cfm (accessed 2021 Jan. 20).
- O*NET database releases archive. O*NET Online, National Center for O*Net Development; 2021. Available: https://www.onetcenter.org/db_releases.html (accessed 2021 Jan. 20).
- Browse by O*NET data. O*NET Online, National Center for O*Net Development; 2021. Available: https://www.onetonline.org/find/descriptor/browse/ (accessed 2021 Jan. 20).
- Standard occupational classification. Washington, DC: United States Bureau of Labor Statistics; 2018. Available: https://www.bls.gov/soc/ (accessed 2021 Jan. 20).
- O*Net occupation update summary. O*NET Online, National Center for O*Net Development; 2021. Available: https://www.onetcenter.org/dataUpdates.html (accessed 2021 Jan. 20).
- Vu V. Connecting the dots: linking Canadian occupations to skills data. Toronto: Brookfield Institute for Innovation + Entrepreneurship; 2019. Available: https://brookfieldinstitute.ca/connecting-the-dots-linking-canadian-occupations-to-skills-data/ (accessed 2021 Jan. 20).
- Hawkins D. Differential occupational risk for COVID‐19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;63(9):817-20.
- Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One. 2020;15(4):e0232452.
- Zhang M. Estimation of differential occupational risk of COVID‐19 by comparing risk factors with case data by occupational group. Am J Ind Med. 2021 Jan;64(1):39-47.
- Which occupations have the highest potential exposure to the coronavirus (COVID-19)? London: Office for National Statistics; 2020. Available: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/articles/whichoccupationshavethehighestpotentialexposuretothecoronaviruscovid19/2020-05-11 (accessed 2021 Jul. 26).
- Azuma K, Yanagi U, Kagi N, Kim H, Ogata M, Hayashi M. Environmental factors involved in SARS-CoV-2 transmission: effect and role of indoor environmental quality in the strategy for COVID-19 infection control. Environ Health Prev Med. 2020;25(1):66.
- Dingel JL, Neiman B. How many jobs can be done at home? [white paper]. Chicago: Becker Friedman Institute for Economics at UChicago; 2020. Available: https://bfi.uchicago.edu/wp-content/uploads/BFI_White-Paper_Dingel_Neiman_3.2020.pdf (accessed 2021 Jul. 26).
- COVID-19: guidance on indoor ventilation during the pandemic. Ottawa: Government of Canada; 2021. Available: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/guide-indoor-ventilation-covid-19-pandemic.html (accessed 2021 Jan. 20).
- Vázquez-Rodríguez I, Estany-Gestal A, Seoane-Romero J, Mora MJ, Varela-Centelles P, Santana-Mora U. Quality of cross-infection control in dental laboratories. A critical systematic review. Int J Qual Health Care. 2018;30(7):496-507.
- Biron C, Brun JP, Ivers H, Cooper CL. At work but ill: psychosocial work environment and well‐being determinants of presenteeism propensity. J Public Ment Health. 2006;5(4):26-37.
- Lui JNM, Andres EB, Johnston JM. Presenteeism exposures and outcomes amongst hospital doctors and nurses: a systematic review. BMC Health Serv Res. 2018;18(1):985.




