Abstract
Background:
To investigate, among Ontario dentists, (1) self-reported barriers to access to sedation and general anesthesia (GA) services and (2) their current use of sedation and GA.
Methods
Of Ontario dentists practising, 3001 were randomly selected to complete a 16-question survey by mail or online in 2011. Mixed analysis of variance (ANOVA) followed by independent-sample t tests or 1-way ANOVA evaluated the relation between dentists’ views and demographic variables including sex, clinical experience and size of primary practice.
Results:
Of the participants (n = 1076; 37.9% response rate), 69.7% were male, 84.4% were general practitioners, mean time in practice was 20.6 years (0.5–42 years) and 42.2% were in cities of over 500 000 people. Most dentists (60.2%) provided anesthesia services, although 38.2% indicated lack of training and the belief that there is no patient demand (25.3%) as reasons not to use anesthesia in their offices. Nitrous oxide was used 17.5% of the time for all dental procedures except implants. Barriers to referral of patients for anesthesia services included high costs associated with sedation/GA (72.2%) and patient fear of anesthesia (33.5%).
Conclusions:
This study identified a perceived lack of patient demand, lack of dentist training, high costs of sedation/GA and patient fear of sedation/GA as primary barriers to use of sedation/GA in Ontario dental practices. The use of various anesthesia modalities is diverse, with 60.2% of dentists providing sedation/GA.
According to the literature, dental patients express a need for sedation and general anesthesia (GA) in conjunction with dental procedures.1-6 Numerous factors are reported as reasons for patients’ interest in sedation/GA, including treatment complexity, medical or behavioural indicators and varying levels of dental anxiety.5,7-9 Studies also report improved oral health resulting from sedation/GA services attributed to increased patient attendance for dental treatment5,7-9
As part of an earlier study, Ontario dentists’ sedation practices were compared with patients’ interest in sedation/GA.10 That study reported that although patients had both an interest and preference for sedation or GA for various dental treatments,2,3,7,8,11,12 dentists were not aware of their patients’ preference.10 This seeming contradiction raises the question of whether the use of sedation/GA with dental procedures is meeting the needs and demands of patients.2,3,6,7,13 Interest lies in whether reasons exist for the reported discrepancy and, further, whether that impacts practice and referral patterns. This resulted in a logical follow-up question regarding what barriers exist to the provision of sedation/GA services.
Current research on differences between patient preference for sedation/GA and dentists’ perception is limited. Multiple reasons have been cited, including dentists’ lack of training; dentist liability and patient safety; and lack of time or remuneration.4,8,11-16 Multiple reasons exist with regard to why patient interest and clinician provision of sedation/GA differ, including the observation that dentists may have limited exposure to sedation/GA in both their training and in their existing clinics.
The purpose of this study was to determine current practice in the use of sedation/GA in dental offices and the barriers to sedation/GA as reported by dental practitioners in Ontario. Recognition of these barriers is needed before strategies can be identified and then implemented to meet patient preference for sedation/GA.
Methods
Dentist Selection
We used a previously described cohort of Ontario dentists’,10 whose views on the use of sedation and GA have been examined. Dentists were selected from the Royal College of Dental Surgeons of Ontario (RCDSO) roster of licensed practising dentists in Ontario in 2011 who included an email address in their RCDSO contact information (n = 6613). A random selection of 3001 dentists was made based on a calculated sample size of 600 with an expected 20% response rate, 95% confidence interval and 4% sampling error.10 Ethics approval for the study was received from the Health Sciences 1 Ethics Review Board at the University of Toronto (#26860).
Data Collection
This descriptive study incorporated a cross-sectional survey, with data collected over 6 weeks. To maximize response rate, clinicians were contacted 4 times and offered paper and electronic versions of the survey. Further details are provided in the earlier study.10
Survey
Survey questions aimed to assess dentists’ reported use of sedation/GA, based on type of dental treatment, and barriers to sedation/GA services and patient referrals. Demographic data were also collected, including dentists’ sex, years in practice, type of practice and size of community served. The survey was field-tested in a sample of general and specialist dentists (n = 20) to assess face validity, comprehension and clarity and revised based on comments received.
Data Analysis
SPSS version 20 was used for descriptive and inferential statistical analysis. Analysis of variance (ANOVA) was used to assess demographic and barrier responses. Statistical significance was set at p < 0.05.
Results
A total of 1076 surveys were returned (713 by mail; 363 online), representing a 37.9% response rate. Study participants were 69.7% male and 30.3% female; general practitioners constituted 84.4% of the sample, with the remaining 15.6% representing clinicians from all 10 dental specialties in Ontario (Table 1).10 Number of years in practice ranged from 0.5 to 42.0, with a mean of 20.6 years. Regarding community served, 42.2% of participants had their primary practice in a city with a population over 500 000; 39.1% were in cities of 50 000–500 000 inhabitants; and 18.6% were in towns of fewer than 50 000 inhabitants. The RCDSO database confirmed that the study population was representative of practising dentists in Ontario, based on all surveyed demographic variables.
|
Characteristic |
No. |
% |
|---|---|---|
|
The sample size varied as some survey questions were not answered by all 1076 respondents. |
||
| Sex (n = 1036) | ||
| Male | 722 | 69.7 |
| Female | 314 | 30.3 |
| Practice type (n = 1036) | ||
| General practitioner | 874 | 84.4 |
| Dental anesthesiologist | 9 | 0.8 |
| Dental public health specialist | 8 | 0.7 |
| Endodontist | 22 | 2.1 |
| Oral medicine/oral pathologist | 4 | 0.4 |
| Oral and maxillofacial radiologist | 1 | 0.1 |
| Oral and maxillofacial surgeon | 22 | 2.1 |
| Orthodontist | 23 | 2.2 |
| Pediatric dentist | 25 | 2.4 |
| Periodontist | 25 | 2.4 |
| Prosthodontist | 23 | 2.2 |
| Time in practice, years (n = 1034, mean = 20.6) | ||
| ≤ 13.0 | 346 | 33.5 |
| 13.1–27.0 | 366 | 35.4 |
| > 27.0 | 322 | 31.1 |
| Community size (n = 1035) | ||
| < 50 000 | 193 | 18.6 |
| 50 001–500 000 | 405 | 39.1 |
| > 500 000 | 437 | 42.2 |
Provision of Anesthesia Services
Most dentists (60.2%) reported providing sedation/GA services in their practice; 39.8% of respondents do not provide these services. A higher proportion of male dentists provide sedation in their practices than female dentists (61.2% vs 58.6%; p < 0.01). Practitioners in communities under 50 000 people are less likely to provide sedation (12%) than those in cities of 50 001–500 000 people (41.8%) or over 500 000 (46.2%) (p < 0.01). No significant relation was noted between provision of sedation/GA and years of clinical experience. Survey respondents identified themselves as the primary provider of sedation in their practices 12% of the time followed by dental anesthesiologists at 6%, other sedation providers at 3.4% and medical anesthesiologists at 3%.
Use of Sedation/Anesthesia Modalities
Dentists reported the percentage of patients who received 1 of 4 types of sedation/GA modalities (nitrous oxide, oral conscious sedation, IV sedation and deep sedation/GA) for 6 specific dental procedures, namely scaling, restorative treatment, root canal therapy, periodontal surgery, extractions and implants (Figure 1). Among the 60.2% of participants providing sedation services in their offices, nitrous oxide was used most of the time (17.1%). Oral, IV and deep sedation/GA were used 9.7%, 7.2% and 5.5% of the time, respectively. Of the 6 dental procedures surveyed, extractions were most likely to include the administration of sedation/GA in conjunction with the procedure.
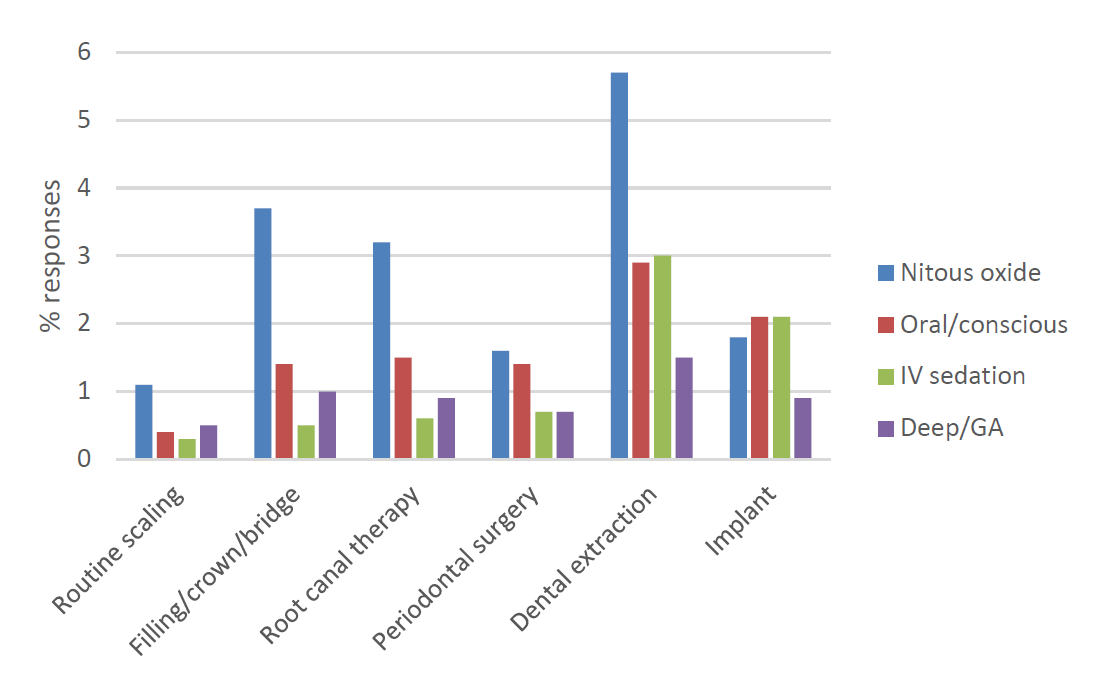
Figure 1: Dentist-reported use of sedation/general anesthesia (GA) for specific dental procedures (n = 648).
Barriers to Provision of Sedation/GA Services
Dentists reported multiple barriers to the use of sedation/GA services. Top reasons included lack of training (38.2%), no patient demand (25.3%), high cost (19.1%) and no patient need (15.1%). Inadequate remuneration, lack of referral source, the belief that sedation or GA is unsafe and other reasons were each reported by fewer than 10% of respondents (Figure 2).
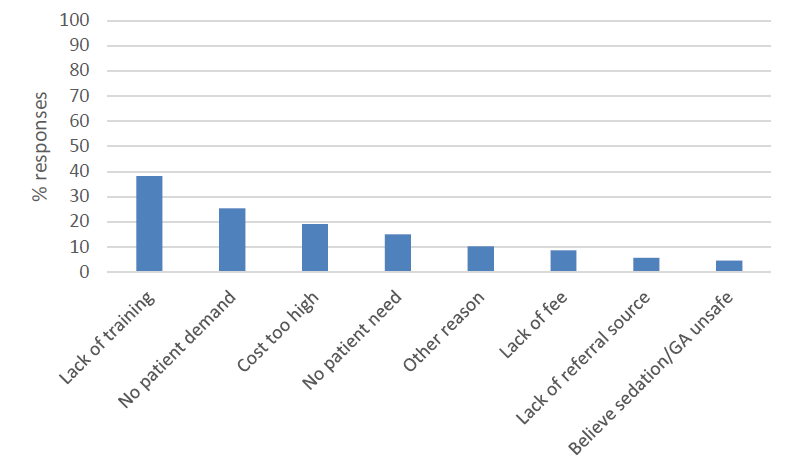
Figure 2: Dentist-reported barriers to providing sedation/general anesthesia (GA) services (n = 1076).
Barriers to Patient Referral for Provision of Anesthesia Services
The high cost of sedation/GA was cited by 72.2% of dentists as the greatest barrier to patient referral for these services. Other barriers included patient fear of sedation or GA (33.5%), long wait time for an appointment (32.2%), long distance to referral source (25.1%), patient disinterest (23.3%) and other barriers (5.9%) (Figure 3).
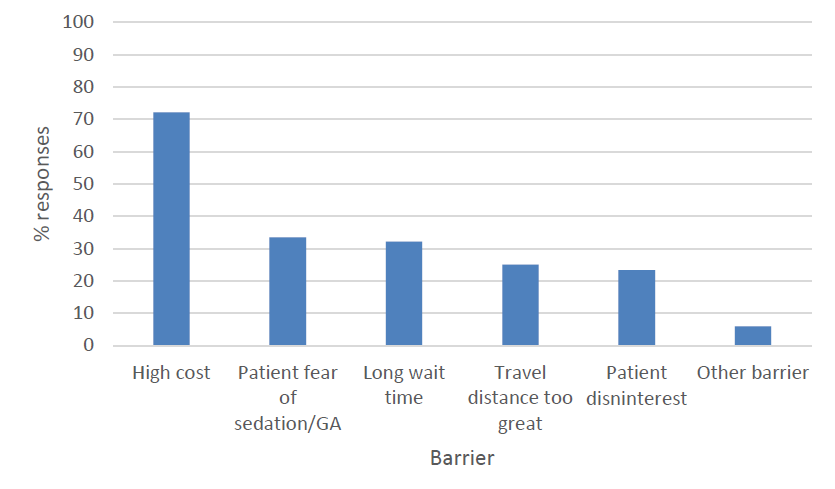
Figure 3: Dentist-reported barriers to patient referral for sedation/general anesthesia (GA) services (n = 1076).
Discussion
Provision of Anesthesia Services and Practice Patterns
The provision of sedation/GA in dental practice is complex, with numerous options available to patients and a range of dental providers able to provide the service. In the current study, 60.2% of respondents provide sedation/GA, most often with nitrous oxide followed by oral sedation. Both of these sedation modalities require the least amount of additional training, associated costs and liability, which may explain the frequency of their use. Ontario dentists approximate their American counterparts where 65% indicated that they provide sedation in their practices14 and nitrous oxide is used most often (21.6% of the time) followed by oral sedation alone (17.1%).1 Our results are prone to potential bias, as sampled dentists may have responded to this survey because of a pre-existing interest in sedation/GA. Ontario dentists’ responses may be under- or over-estimated as no distinction was made between anesthesia modalities nor adjustments made for the use of overlapping modalities.
Predominant providers of sedation/GA were more likely to be male dentists, practising in larger communities. Potentially fewer female practitioners work full time or own practices and, consequently, have less ability to influence sedation/GA provision or resources available to their patients. In addition, the number of male dental graduates has historically exceeded the number of female graduates creating a gender discrepancy. A subsequent Ontario study similarly identified rural locations to be a predictor for poor access to deep sedation and GA, although other modalities of sedation were not studied.17 Preliminary studies, such as this one, are valuable and useful to direct further research into optimal practice patterns and the number of providers required to better meet patients’ preferences for sedation/GA in dental offices.
Barriers to Provision of Sedation/GA and to Patient Referral for Anesthesia Services
Numerous barriers influence dentists’ provision and use of sedation/GA. Understanding these barriers is required to identify strategies to optimize the delivery of sedation/GA to patients.
Cost and Lack of Remuneration: Other studies17,18 have confirmed our finding that the cost of sedation/GA services is a financial burden to dentists and patients alike and poses a significant barrier to their use in dental practices. In Ontario, adjunctive sedation/GA costs can be covered in part or in total by third-party payers (i.e., insurance companies, government social assistance plans) or the patient. Third-party payers may not consider sedation or GA to be “medically necessary” and view local anesthesia as less costly and as effective.19 Currently, no accepted definition of “medical necessity” exists. Although need can be readily identified in behaviourally challenged populations, such as pediatric patients or those who are physically or mentally challenged, it is less obvious among those with dental fear.19 Yet, many reports in the literature corroborate the view that sedation/GA can manage patient anxiety, allowing dental procedures that otherwise would not be performed.1-6
Multiple factors may contribute to dentists’ perception of inadequate remuneration, including not only the units of service time per patient but also the operational fees associated with instituting sedation/GA in a dental clinic and the difficulty of managing anxious patients. The contributing factors may operate independently or in concert. For example, managing anxious patients may prolong appointments or affect a practitioner’s schedule with unpredictable cancellations. Further research is required to clarify and mitigate the specific contributing factors to remove lack of remuneration as a barrier to the provision of sedation/GA.
No Patient Demand, No Patient Need and Patient Disinterest: The literature does not substantiate the view that patients do not demand, need or have interest in sedation/GA for dental procedures.1-6 Canadian studies indicate that dentists underestimate the need and demand for such services, as did our sample of dentists. Multiple studies have demonstrated that patients do want sedation/GA, but that dentists perceive they do not.17,18 Patients and dentists have disparate points of view, which are challenging to account for.10 Numerous variables contribute to patient need, demand or interest, including, but not limited to, the patient’s knowledge of sedation/GA options available for dentistry, the dynamic nature of patient anxiety, the dental procedure being performed and cost to the patient for sedation/GA services. Dentists may dismiss or be unaware of these variables and, thus, perceive no patient need, demand or interest.
Believe Sedation/GA is Unsafe and Patient Fear of Sedation/GA: A 2018 study estimated the prevalence of mortality and morbidity related to office-based deep sedation and GA at 0.8 and 0.25 per million cases, respectively.20 The number of studies investigating or assessing the prevalence of patient fear of sedation/GA or dentist perceptions of sedation/GA safety is limited. It is unclear what affects practitioner and patient views that sedation/GA is unsafe. Perhaps media reports of sedation/GA mortality magnify the risks disproportionately to actual statistics, or any mortality may be considered prohibitive for dental procedures.
Other Barriers to Sedation/GA: Respondents in the current study (2011) and a subsequent study17 cited lack of training in the provision of sedation/GA as a barrier to its administration in their practices. In Canada, no detailed nationwide standardized competencies in the administration of sedation/GA exist for dental schools. Consequently, training and the clinical competency of graduates vary.21 It is possible that variable training affects dentists’ perceptions of other noted barriers to sedation/GA, such as its safety and patient need or demand for such services.
Survey respondents noted inability to find a referral source as a barrier preventing the provision of anesthesia services in their practices. Data on the location of practices with sedation/GA services in Ontario has not been published, nor has the number of sedation/GA providers. This information would be helpful as at least a first step in assessing the availability of sedation/GA services in the province.
For study practitioners who were able to locate a referral source, the reported wait time to see an anesthesia provider was too long, making it a nonviable treatment option, or too far away for their patients to access. A subsequent study showed that type of practice, whether providers were office-based or itinerant and patient health status affected wait times and distances patients had to travel for sedation/GA.17 It is evident that numerous remedies are required to reduce wait times and distance for patients to access sedation/GA services in dental practices.
Study Strengths and Limitations
The primary strength of this study is its demonstration of possible barriers to the provision of sedation/GA and of the practice and pattern of use of sedation/GA across Ontario. The higher than expected response rate, along with the fact that survey participants represented all Ontario dentists in terms of gender, mix of generalists and specialists, clinical years of experience and size of community served, provides confidence in the generalizability of the data. Significant findings in this original study have been strengthened by similar data reported in subsequent studies.17,18
Limitations include the study’s observational design, which relies on dentists’ recall and estimates of percentage use of anesthesia modalities.22-23 Percentages for certain procedures and modalities are < 1%. Small mean values and large standard deviations limit the ability to draw conclusions about the use of such anesthesia modalities in practice. However, health practitioner self-reporting is the current standard method used in the reviewed literature for analyzing practice patterns and obtaining practitioner views.
The data indicate barriers to the provision of sedation/GA and reflect variability in the provision of sedation across Ontario. These results are important in the potential creation of mechanisms to optimize the provision of sedation/GA care for patients.
Conclusions
Most dental practitioners reported providing sedation/GA in their practices using a variety of modalities; however, it is unclear whether current reported use and practice patterns satisfy patient preferences. In addition, multiple barriers limit the provision of sedation/GA in dental practices. The most noted barriers were a perceived lack of patient interest and lack of dentist training. Efforts to optimize sedation/GA services in Ontario are complex and multifactorial. More research and resources should aim to identify solutions that will effectively mitigate the barriers to accessing sedation/GA services for Ontario dental patients.
THE AUTHORS
Corresponding author: Dr. L. Dempster, Faculty of Dentistry, University of Toronto, 124 Edward St, Toronto ON M5G 1G6. Email: l.dempster@dentistry.utoronto.ca
Acknowledgement: This study was funded by the discipline of dental anesthesia at the faculty of dentistry, University of Toronto. The results were originally presented in March 2013 at the International Association of Dental Research Meeting in Seattle, Washington, USA. Dr. Patodia won an award for presenting this research at the 2013 University of Toronto Research Day.
The authors gratefully acknowledge Dr. Daniel Haas for his invaluable knowledge and expertise throughout this project, co-authorship of the first article from this study and comments on earlier versions of this manuscript.
The authors have no declared financial interests.
This article has been peer reviewed.
References
- Abdulwahab M, Al-Sayegh F, Boynes SG, Abdulwahab H, Zovko J, Close J. Assessing the need for anesthesia and sedation services in Kuwaiti dental practice. Anesth Prog. 2010;57(3):91-5.
- Allen EM, Girdler NM. Attitudes to conscious sedation in patients attending an emergency detail clinic. Prim Dent Care. 2005;12(1):27-32.
- Chanpong B, Haas DA, Locker D. Need and demand for sedation or general anesthesia in dentistry: a national survey of the Canadian population. Anesth Prog. 2005;52(1):3-11.
- Dionne RA, Gordon SM, McCullagh LM, Phero JC. Assessing the need for anesthesia and sedation in the general population. J Am Dent Assoc. 1998;129(2):167-73.
- Milgrom P, Newton JT, Boyle C, Heaton LJ, Donaldson N. The effects of dental anxiety and irregular attendance on referral for dental treatment under sedation within the National Health Service in London. Community Dent Oral. 2010;38(5):453-9.
- Smith TA, Heaton LJ. Fear of dental care: are we making any progress? J Am Dent Assoc. 2003;134(8):1101-8.
- Armfield JM, Spencer AJ, Stewart JF. Dental fear in Australia: who’s afraid of the dentist? Aust Dent J. 2006;51(1):78-85.
- Morgan CL, Skelly AM. Conscious sedation services provided in secondary care for restorative dentistry in the UK: a survey. Br Dent J. 2005;198(10):631-5.
- Moore R, Brødsgaard I. Dentists’ perceived stress and its relation to perceptions about anxious patients. Community Dent Oral Epidemiol. 2001;29(1):73-80.
- Patodia S, LeBlanc V, Haas DA, Dempster LJ. Ontario dentists’ estimation of patient interest in anesthesia. J Can Dent Assoc. 2017;82:h2.
- Baron RS, Logan H, Kao CF. Some variables affecting dentists’ assessment of patients’ distress. Health Psychol. 1990;9(2):143-53.
- Boyle CA, Newton T, Milgrom P. Who is referred for sedation for dentistry and why? Br Dent J. 2009;206(6):E12; discussion 322-3.
- Coulthard P, Bridgman CM, Gough L, Longman L, Pretty IA, Jenner T. Estimating the need for dental sedation. 1. The indicator of sedation need (IOSN) – a novel assessment tool. Br Dent J. 2011;211(5):E10.
- Boynes SG, Moore PA, Tan Jr PM, Zovko J. Practice characteristics among dental anesthesia providers in the United States. Anesth Prog. 2010;57(2):52-8.
- Gordon SM, Dionne RA, Snyder J. Dental fear and anxiety as a barrier to accessing oral health care among patients with special health care needs. Spec Care Dentist. 1998;18(2):88-92.
- Wilson PW, Petticrew M, Calnan M, Nazareth I. Effects of a financial survey on health researchers’ response to an online survey: a randomized controlled trial. J Med Internet Res. 2010;12(2):e13.
- Adams A, Yarascavitch C, Quiñonez C, Azarpazhooh A. Use of and access to deep sedation and general anesthesia for dental patients: a survey of Ontario dentists. J Can Dent Assoc. 2017;83:h4.
- Campbell J. Dental sedation and general anaesthesia in Manitoba: a survey of need, demand, and perceptions. Master’s thesis. Toronto: University of Toronto; 2015. Available from: https://tspace.library.utoronto.ca/handle/1807/74687
- Flick WG, Clayhold S. Who should determine the medical necessity of dental sedation and general anesthesia? A clinical commentary supported by Illinois patient and practitioner surveys. Anesth Prog. 1998;45(2):57-61.
- El-Mowafy AO. Mortality and morbidity in office-based deep sedation and general anaesthesia for dentistry in Ontario. Master’s thesis. Toronto: University of Toronto; 2018. Available: https://tspace.library.utoronto.ca/handle/1807/89491
- Ryding HA, Murphy HJ. Use of nitrous oxide and oxygen for conscious sedation to manage pain and anxiety. J Can Dent Assoc. 2007;73(8):711.
- Hill KB, Hainsworth JM, Burke FJT, Fairbrother KJ. Evaluation of dentists’ perceived needs regarding treatment of the anxious patient. Br Dent J. 2008;204(8):E13; discussion 442-3.
- Foley J. The way forward for dental sedation and primary care? Br Dent J. 2002;193(3):161-4.



