Abstract
Background: In contrast to an expected increase in demand for periodontal services with aging of the population, it appears that referrals to periodontists are declining.
Objective: To determine the extent to which general dentists in Nova Scotia, Canada, provide periodontal and surgical implant therapies and to determine the factors influencing a dentist's decision to provide treatment or refer patients to a specialist.
Methods: A cross-sectional survey study was performed. The survey questionnaire was mailed to all 443 general dentists practising in Nova Scotia in summer 2009. The questionnaire presented several clinical scenarios and asked respondents whether they would treat the patient in the office or refer to a specialist. The data were analyzed by logistic regression.
Results: Of the 279 (63.0%) dentists responding to the survey, 272 (61.4% of the total) were eligible for inclusion in the analysis. The majority of dentists reported rendering nonsurgical periodontal therapy, including scaling (98.5%; 262/266), periodontal maintenance (95.9%; 255/266), and treatment for bruxism (95.1%; 252/265). The most common surgical procedures performed by dentists were frenectomy (29.4%; 78/265), gingivectomy (29.3%; 77/263) and crown-lengthening procedures (17.0%; 46/271). Eleven factors significantly influenced dentists' decisions to treat or refer patients. The most common criteria used in selecting a periodontist were satisfaction of previous patients, previous success with the treatment, and the personality of and good communications with the periodontist.
Conclusions: In this study, dentists reported rendering nonsurgical periodontal therapy on a wide scale, whereas their involvement in oral or periodontal and implant surgical therapies was limited.
One of the significant demographic changes occurring in Canada today is the aging of the population. In 2009, the median age of Canadians was 39.5 years, compared to 36.4 years just 10 years earlier.1 Moreover, the proportion of Canadian seniors (age 65 years and older) increased from 13.0% in 2001 to 13.9% in 2009.1 In 2009, seniors constituted 15.8% of the population in the Canadian province of Nova Scotia, 1.9 percentage points above the national average.1
The aging of the population has important implications for oral health professionals, particularly those involved in managing periodontal diseases. Various epidemiologic studies have reported increasing prevalence and severity of periodontitis with age.2-9 This association is believed to be due to the cumulative result of periodontal disease progression over time rather than greater susceptibility of older individuals to the disease process.10 Therefore, it is reasonable to expect that the need for dental and periodontal services will increase as the population ages.11,12
Contrary to the expected increase in demand for periodontal services, however, reports in the dental literature suggest that in North America, referral to periodontists is declining.11-13 A national survey of dental practices in the United States revealed an 8.3% increase in the total number of dental procedures performed between 1990 and 1999.12 During the same period, there was a 1.6% increase in the number of periodontal services performed by general dentists, counterbalanced by a 1.7% decrease in services rendered by periodontists. A more recent survey of dental services rendered in the United States in 2005-06 reported that general dentists performed 2.8 times more comprehensive periodontal examinations, 7.6 times more periodontal scaling and root planing, and 1.4 times more periodontal maintenance procedures than periodontists.13 Therefore, in the United States, it appears that the increased demand for periodontal services is being met by general dentists, not periodontists.
In addition to these quantitative changes, there are reports of qualitative changes in general dentists' referral patterns to periodontists. In a retrospective analysis of periodontal referral patterns in 3 regions of the United States over a 20-year period, Cobb and colleagues14 reported that, among referred patients, both the severity of periodontal disease and the number of missing teeth increased over time. In another study of 100 newly referred patients from 3 periodontal practices in Kansas City, Missouri, Dockter and colleagues15 reported that patients received the same level of periodontal care in general dental offices, irrespective of their periodontal disease status.
This study was undertaken to better understand the provision of periodontal care by general dentists and their profile of referrals to periodontists in Nova Scotia, Canada. In a previous publication, we reported on the extent to which general dentists practising in Nova Scotia examined their patients for periodontal diseases.16 The aim of the present study was to determine the extent and nature of periodontal and surgical implant therapies rendered by the same dentists. The study also investigated factors that may significantly influence a dentist's decision to provide treatment in the office or refer the patient to a specialist.
Methods
Survey Instrument
Details of the methods used in this investigation were reported previously.16 Briefly, following receipt of approval from the Dalhousie University Health Sciences Research Ethics Board, a survey questionnaire was mailed to all 443 general dentists licensed by the Provincial Dental Board of Nova Scotia in summer 2009. To maximize the response rate, follow-up requests were sent by mail at 2 and 6 weeks after the initial mailing.17
The questionaire consisted of 3 sections. Section 1 contained demographic questions about the dentist and questions concerning characteristics of the dental office. Section 2 asked about the extent of the dentists' periodontal examinations, their reasons for referring patients to a specialist and their criteria for selecting a periodontist. Finally, in section 3, the dentists were presented with 23 clinical scenarios and were asked how they would manage each scenario: treat in the office, refer to a periodontist or refer to another specialist.
Data Analysis
Survey data were analyzed with statistical software (Statistical Application Software, version 9.2, SAS Institute, Chicago, IL). Descriptive statistics, including frequency distributions and measures of central tendency, were generated. For 10 of the 23 clinical scenarios, logistic regression analyses were performed to identify potential dentist- and dental office-related factors (e.g. dentist's sex, location of practice, continuing education [CE] courses taken) that would influence the dentist's decision to treat in the office or "refer out" (Table 1). The remaining scenarios were not used in the regression analysis, as the majority of the dentists selected the same outcome. Statistical tests were interpreted at the 5% significance level.
Table 1: Clinical scenarios used in the logistic regression analysis 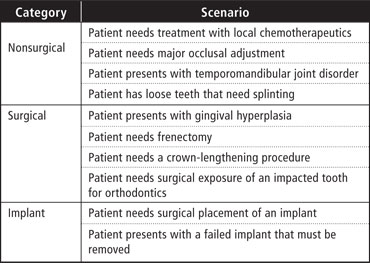
Results
Of the 443 questionnaires sent, 279 responses (63.0%) were returned. Seven responses were excluded from analysis because the dentist had either retired from practice or worked in a military or prison clinical setting, for a final response rate of 61.4% (n = 272). The majority of respondents were male (63.2% [172/272]). Among those who revealed their age, mean age (± standard deviation) was 49.6 ± 9.0 years for men (n = 164) and 39.9 ± 10.8 years for women (n = 96). Of the dentists who responded to the survey, 121 (44.5%) practised in the province's single major urban setting (Halifax). Interestingly, 46.2% of periodontists in Nova Scotia also practise in Halifax.18 Demographic information for study participants is summarized in Table 2.
Table 2: Demographic and practice characteristics of dentists who participated in the survey 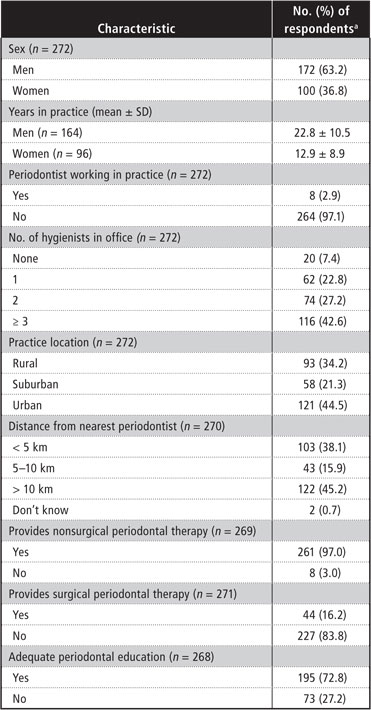
SD = standard deviation.
aExcept where indicated otherwise.
Profile of Periodontal Therapy and Referral Patterns
For 23 clinical scenarios, each dentist was asked to select 1 of 3 options for management: treat in the office, refer to a periodontist or refer to another specialist. The clinical scenarios were classified in 3 categories: nonsurgical periodontal therapy, oral or periodontal surgical therapy, and surgical implant or implant-related therapy.
Nonsurgical Periodontal Therapy
Most of the respondents reported providing scaling (98.5%; 262/266), periodontal maintenance (95.9%; 255/266) and treatment for bruxism (95.1%; 252/265) for their patients (Fig. 1). For temporomandibular joint (TMJ) disorders, 42.8% (113/264) of the dentists reported providing treatment, whereas the remainder referred patients to periodontists (22.7%; 60/264 )or to other specialists (34.5%; 91/264). Although 34.1% (88/258) of the dentists reported providing major occlusal adjustment for their patients, 44.6% (115/258) reported referring patients to periodontists for this type of treatment, and the remaining 21.3% (55/258) reported referring patients to other specialists.
Table 3 lists the factors that were identified as significant predictors of dentists rendering various periodontal therapies in the office, versus referring patients to a periodontist. For nonsurgical therapies, male dentists and those intending to take CE courses in periodontal plastic surgery in the next 2 years were more likely to treat patients in their own offices rather than referring them to other specialists (Table 3). Those practising in an urban location and not planning to take nonsurgical periodontal courses were also more likely to treat in their own offices.
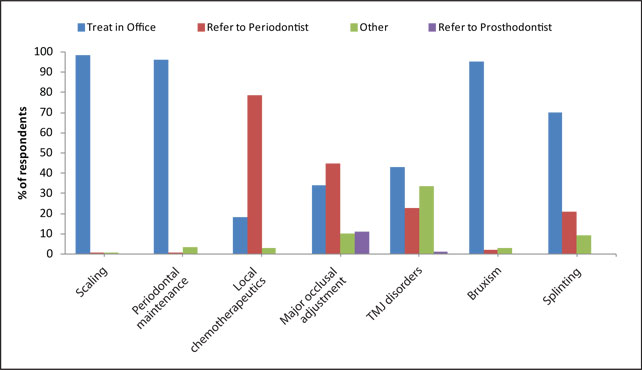 Figure 1: Profile of nonsurgical periodontal therapy among general dentists.
Figure 1: Profile of nonsurgical periodontal therapy among general dentists.
Table 3: Results of logistic regression analysis of factors influencing dentists' decisions to treat in the office or refer out 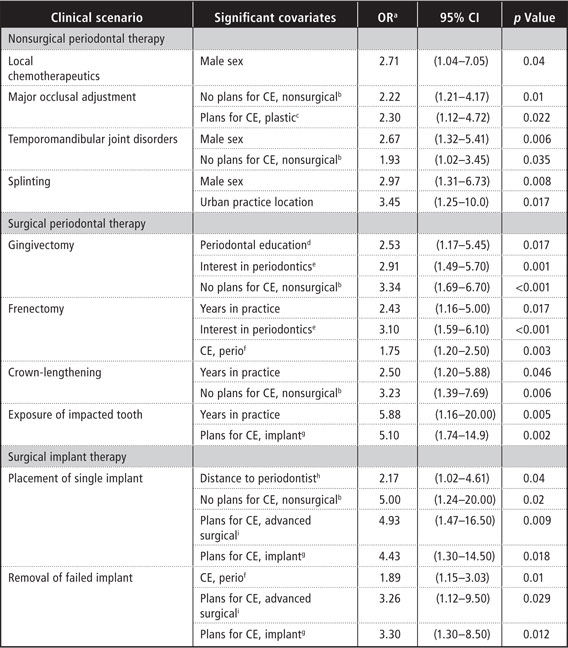
aOdds ratio (treat in office vs. refer), with 95% confidence interval. If OR > 1, the presence of the factor was likely to result in the dentist treating the patient in his or her own office.
bNo plans to take continuing education (CE) courses in nonsurgical periodontics in the next 2 years.
cPlans to take CE courses in periodontal plastic surgery in the next 2 years.
dAdequacy of periodontal education in dental school (yes vs. no).
eInterest in periodontics since graduation from dental school (increased vs. remained the same or decreased).
Oral or Periodontal Surgical Therapy
The most common surgical therapies rendered by the dentists in this study were frenectomy (29.4%; 78/265), gingivectomy (29.3%; 77/263) and crown-lengthening procedures (17.0%; 46/271) (Fig. 2). The dentists performed other surgical procedures much less frequently. Only 0.4% (1/267), 4.5% (12/269) and 4.8% (13/269) of the dentists reported performing preprosthetic vestibular extension procedures, gingival grafts and removal of a torus, respectively. Most dentists (93.3%; 251/269) reported referring patients in need of gingival grafts to a periodontist, whereas 64.7% reported referring patients in need of torus removal to an oral surgeon. Finally, 98.1% (265/270) of the dentists reported referring patients in need of grafting of osseous defects to a periodontist, whereas only 0.7% (2/270) reported referring these patients to an oral surgeon.
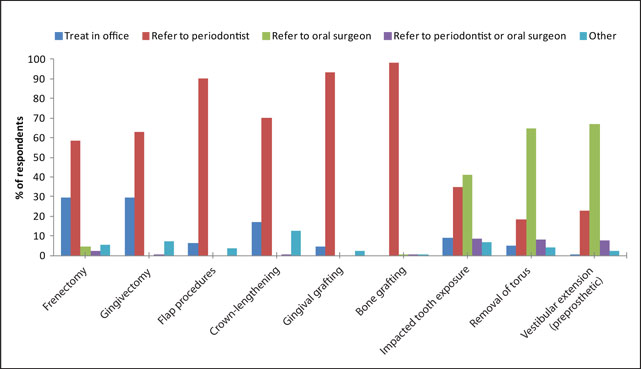 Figure 2: Profile of oral and periodontal surgical therapy among general dentists.
Figure 2: Profile of oral and periodontal surgical therapy among general dentists.
The following factors were found to be predictors of provision of various oral and periodontal surgical therapies in the office: belief that periodontal education in dental school had been adequate, increased interest in periodontics since graduating from dental school, not intending to take CE courses in nonsurgical periodontics in the next 2 years, intending to take CE courses in surgical implant dentistry in the next 2 years, more hours of CE courses in periodontics in the past 3 years and more years in practice (Table 3).
Surgical Implant or Implant-Related Therapy
Few participants reported providing surgical implant or implant-related therapy. Only 7.8% (21/270) of the dentists reported placing singleunit implants (Fig. 3). Of the remainder, 23.7% (64/270) reported referring patients to either a periodontist or an oral surgeon, whereas 34.8% (94/270) reported referring patients specifically to a periodontist and 26.3% (71/270) specifically to an oral surgeon; 7.4% (20/270) reported referring patients to "other" practitioners.
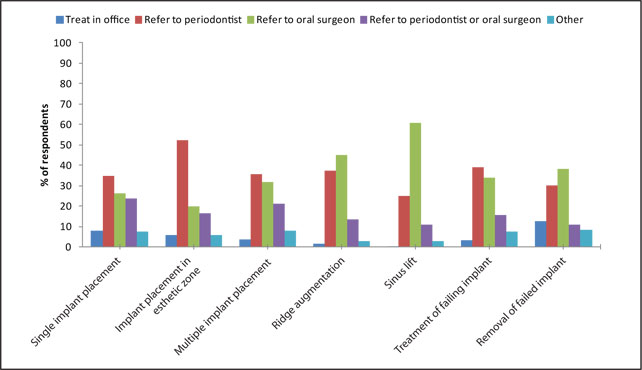 Figure 3: Profile of surgical implant or implant-related therapy among general dentists.
Figure 3: Profile of surgical implant or implant-related therapy among general dentists.
The same trends applied to placement of multi-unit implants and implants in the esthetic zone. Only 5.6% (15/270) of respondents reported placing implants in the esthetic zone. A larger proportion (16.3%; 44/270) of dentists reported referring patients in need of implants in the esthetic zone to either a periodontist or an oral surgeon, whereas 52.2% (141/270) reported referring patients specifically to a periodontist and 20.0% (54/270) specifically to an oral surgeon. Similarly, only 1.5% (4/268) of dentists reported performing ridge augmentation procedures in preparation for placing implants. Again, a larger proportion (13.4%; 36/268) of the dentists reported referring patients to either a periodontist or an oral surgeon, whereas 44.8% (120/268) reported referring patients specifically to an oral surgeon and 37.3% (100/268) specifically to a periodontist. For both types of procedures, the remaining dentists reported referring patients to "other" practitioners; (5.9% [16/270] for placement of implants in the esthetic zone and 3.0% [8/268] for ridge augmentation).
The following factors were found to be predictors of provision of surgical implant therapy in the office: proximity to the nearest periodontist (with greater distance from the nearest periodontist leading to greater likelihood to refer out), not intending to take CE courses in nonsurgical periodontics in the next 2 years, intending to take CE courses in advanced surgical procedures and/or surgical implant dentistry in the next 2 years and more hours of CE courses in periodontics taken in the past 3 years (Table 3).
Reasons for Referring Patients to a Specialist
The most common reason for referring patients to a specialist, cited by 79.4% of respondents, was inadequate training or experience (Fig. 4). The next 2 most common reasons were patients' complicated systemic health (reported by 37.9%) and poor outcome obtained in the past (reported by 30.5%). The least common reasons for referring patients to a specialist were inadequate insurance payment (reported by 0.7%) and "patient cannot afford treatment" (reported by 1.1%).
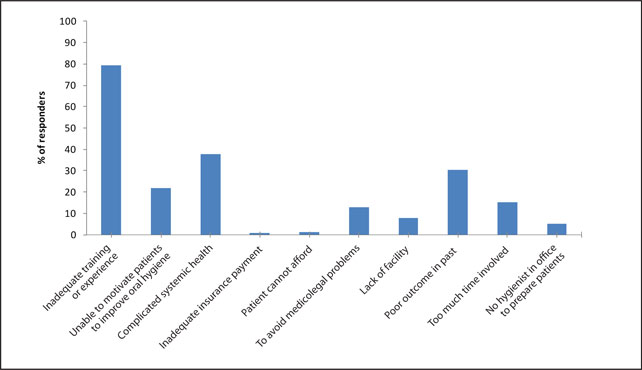 Figure 4: General dentists' reasons for referring patients to a specialist.
Figure 4: General dentists' reasons for referring patients to a specialist.
Selection of a Periodontist
The 3 most common criteria reported for selecting a periodontist were previous patient satisfaction (cited by 74.9% of respondents), the personality of the periodontist (70.8%) and previous success with the periodontist (70.0%) (Fig. 5). Other common criteria were good communication with the periodontist (68.9%), surgical skills and competency of the periodontist (68.2%) and availability in the community (64.7%). Surprisingly, the least common criterion for selecting a periodontist, cited by only 6.0% of respondents, was fellowship in the Royal College of Dentists of Canada.
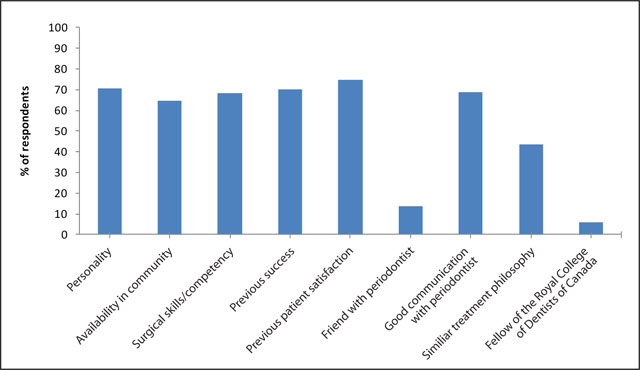 Figure 5: Criteria used by general dentists in selecting a periodontist.
Figure 5: Criteria used by general dentists in selecting a periodontist.
Discussion
As described by previous investigators,11,13,19 most of the dentists in this study reported providing nonsurgical periodontal therapy in their own offices. In a survey of periodontal services rendered by general dentists in the state of Virginia in 2005-06, the majority of dentists reported providing scaling, root planing and periodontal maintenance services in their practices.19 Comparing dental practice trends in the state of Washington between 1993 and 1999, another study reported that the majority of nonsurgical periodontal therapy in both years was performed in general dental offices.11
In contrast to the situation for nonsurgical periodontal therapy, the dentists in this study reported providing oral or periodontal surgical therapy to a much more limited extent. Frenectomy, gingivectomy and crown-lengthening procedures were the most common surgical procedures performed by respondents to this survey. Whereas only 17.0% of the dentists in the current study reported performing crown-lengthening procedures, 48% of the general dentists in the Virginia study reported rendering this surgical service.19 Furthermore, 63.1% of the dentists in the current study reported referring gingivectomy procedures to a periodontist, whereas in the Washington study, this procedure was performed more frequently by general dentists.11 Such regional variation could be due to a number of factors, including differences in undergraduate education, proximity to a periodontist, presence of managed care dictating referral, and whether the dentists had attended a post–dental school training or residency program. In the Virginia study, for example, 39% of dentists surveyed had attended some form of a postgraduate education,19 whereas the dentists in the current study were all general practitioners.
Less than 10% of the dentists in the current study reported placing single implants, and even fewer reported placing implants in the esthetic zone. The data reveal that periodontists would receive most of the referrals for single and multiple implants and for implants to be placed in the esthetic zone. In addition, the dentists reported referring patients in need of implant-related surgical procedures (i.e., sinus and ridge augmentations and removal of failed implants) more commonly to oral surgeons. A recent national survey of Canadian dentists reported on factors associated with dentists' adoption of implant therapy into practice.20 Although it had a low response rate (only 9.3%), the study reported that the rate of dentists providing implant therapy, both surgical and restorative, was lowest in the Atlantic region. This result may have been due to training at the undergraduate level, regional economics or availability of specialists. Further studies are needed to determine the reasons for this practice variation.
We identified 11 factors that influenced dentists' decisions to treat a patient or refer to a specialist. Five factors were related to having taken or intending to take CE courses in periodontics and/or implant dentistry. Dentists with more hours of CE courses taken in the past 3 years were significantly more likely to perform frenectomy procedures in their offices. Similarly, the Virginia study reported a positive correlation between hours of CE in periodontics and performance of crown-lengthening procedures by dentists. 19 Moreover, the current results demonstrate that dentists who did not intend to take courses in nonsurgical periodontics within 2 years were significantly less likely to refer patients who needed major occlusal adjustment, treatment for TMJ disorders, gingivectomy, crown lengthening and surgical placement of single implants. Further studies are needed to determine the factors accounting for these results. Lee and colleagues21 found that dentists who did not refer patients to the periodontist were less interested in taking CE courses in periodontics than dentists who made such referrals. In addition, dentists in the current study who did intend to take CE courses in advanced surgical procedures or surgical implant dentistry within 2 years were significantly more likely to place single-unit implants and/or to remove failed implants than those who did not intend to take such courses.
The results reported here further show that dentists who believed their periodontal education in dental school was adequate were more likely to perform gingivectomy procedures in their offices than those who believed otherwise. This result corroborates the study of Lee and colleagues,21 who examined the referral patterns of 160 general dentists practising in Michigan. In that study, dentists who referred more than 3 patients per month felt less well prepared by their education in dental school than dentists who referred fewer than 3 patients per month to a periodontist.
The most common criteria that general dentists used in selecting a periodontist for referral were the satisfaction of previous patients, the periodontist's previous success with treatment, and the personality of and good communications with the periodontist. In addition, 64.7% of the dentists surveyed cited availability in the community as an important factor in selecting a periodontist. In a United Kingdom study, distance from the specialist was the only factor significantly influencing the number of referrals by general dentists.22
Finally, fellowship in the Royal College of Dentists of Canada was considered important in selecting a periodontist by just 6% of the dentists responding to this survey. In this context, it is important to note that the mandate of the College includes administering the national dental specialty examination.23 Since 2002, all licensed specialists have been required to pass this examination before practising as a specialist.24 Moreover, all licensed specialists who graduated since 2002 are eligible for fellowship. Attaining fellowship status, however, is not mandatory; rather, it is a matter of paying annual dues. Licensed specialists without a fellowship are those who graduated before 2002 or elected not to apply for fellowship status.
Although the results of this study cannot be generalized to other provinces in Canada, the findings can be used by local stakeholders at various levels. Dental educators in Nova Scotia, for example, could use these findings when developing courses for both undergraduate and graduate periodontics programs. Moreover, knowing the criteria that general dentists use when selecting a periodontist for referral will allow periodontists to improve their working relationships with their general practitioner colleagues in an effort to improve patient care. Finally, other investigators can use the methodology of this study to explore the dynamics of general practitioner–specialist referral in their provinces.
The results of this survey concur with others, in terms of the multitude of factors responsible for declining referral from general dentists to periodontists. These findings will facilitate a better understanding of the dynamics of the referral process, which may ultimately lead to more timely diagnosis and treatment of periodontal disease. Further investigation, including qualitative research, is warranted to examine these factors in greater detail.
THE AUTHORS
References
- Statistics Canada. The Daily, November 27, 2009. Canada's population estimates: age and sex. Available: http://www.statcan.gc.ca/daily-quotidien/091127/dq091127b-eng.htm. Accessed 4/7/2011, 2011.
- Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999;70(1):13-29.
- Brown LJ, Oliver RC, Loe H. Evaluating periodontal status of US employed adults. J Am Dent Assoc. 1990;121(2):226-32.
- Gilbert GH, Heft MW. Periodontal status of older Floridians attending senior activity centers. J Clin Periodontol. 1992;19(4):249-55.
- Loe H, Anerud A, Boysen H, Smith M. The natural history of periodontal disease in man. Study design and baseline data. J Periodontal Res. 1978;13(6):550-62.
- Hugoson A, Norderyd O, Slotte C, Thorstensson H. Distribution of periodontal disease in a Swedish adult population 1973, 1983 and 1993. J Clin Periodontol. 1998;25(7):542-8.
- Schurch E,Jr, Lang NP. Periodontal conditions in Switzerland at the end of the 20th century. Oral Health Prev Dent. 2004;2(4):359-68.
- Susin C, Dalla Vecchia CF, Oppermann RV, Haugejorden O, Albandar JM. Periodontal attachment loss in an urban population of Brazilian adults: effect of demographic, behavioral, and environmental risk indicators. J Periodontol. 2004;75(7):1033-41.
- Yoneyama T, Okamoto H, Lindhe J, Socransky SS, Haffajee AD. Probing depth, attachment loss and gingival recession. Findings from a clinical examination in Ushiku, Japan. J Clin Periodontol. 1988;15(9):581-91.
- Niessen LC, Fedele DJ. Aging successfully: oral health for the prime of life. Compend Contin Educ Dent. 2002;23(10 Suppl):4-11.
- Robertson PB, del Aguila MA, Anderson MH. Trends in periodontal care. Periodontol 2000. 2002;30:104-10.
- Brown LJ, Johns BA, Wall TP. The economics of periodontal diseases. Periodontol 2000. 2002;29:223-34.
- American Dental Association. The 2005-06 survey of dental services rendered. 2007:1-159.
- Cobb CM, Carrara A, El-Annan E, Youngblood LA, Becker BE, Becker W, et al. Periodontal referral patterns, 1980 versus 2000: a preliminary study. J Periodontol. 2003;74(10):1470-4.
- Dockter KM, Williams KB, Bray KS, Cobb CM. Relationship between prereferral periodontal care and periodontal status at time of referral. J Periodontol. 2006;77(10):1708-16.
- Ghiabi E, Weerasinghe S. The periodontal examination profile of general dentists in Nova Scotia, Canada. J Periodontol. 2011;82(1):33-40. Epub 2010 Jul 10.
- Edwards PJ, Roberts I, Clarke MJ, DiGuiseppi C, Wentz R, Kwan I, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database of System Rev. 2009(3):MR000008.
- Canadian Academy of Periodontology. Find a periodontist Available: http://www.cap-acp.ca/en/search/index.php?page=2&search=NS. Accessed 4/11/2011.
- Lanning SK, Best AM, Hunt RJ. Periodontal services rendered by general practitioners. J Periodontol. 2007;78(5):823-32.
- Esfandiari S, Majdzadeh R, Feine J. Types of Canadian dentists who are more likely to provide dental implant treatment. Implant Dent. 2011;20(1):76-84.
- Lee JH, Bennett DE, Richards PS, Inglehart MR. Periodontal referral patterns of general dentists: lessons for dental education. J Dent Educ. 2009;73(2):199-210.
- Linden GJ, Stevenson M, Burke FJ. Variation in periodontal referral in 2 regions in the UK. J Clin Periodontol. 1999;26(9):590-5.
- Royal College of Dentists of Canada - Home Available: http://www.rcdc.ca/home.cfm Accessed 5/6/2011.
- Kennedy DB. The Royal College of Dentists of Canada: history, misconceptions and recent developments. J Can Dent Assoc. 2001;67(10):574-6.
