Abstract
Introduction:
Although condylar fractures are common in the field of oral and maxillofacial surgery, the approach to their treatment is not straightforward. Multiple soft-tissue approaches are available, but it is unclear which yields the best outcomes. In this retrospective study, we aimed to determine whether a transparotid or submandibular soft-tissue approach to treating condylar fractures yields better outcomes.
Methods
This study consisted of a retrospective chart audit and an in-person assessment. The chart audit involved all patients who presented to the Queen Elizabeth II Health Sciences Centre (Halifax) between 2012 and 2022 with condylar fracture treated with open reduction and internal fixation. The chart review assessed each patient’s maximum interincisal opening, paresthesia, nerve function, infection and occlusion. The in-person assessment further assessed scar satisfaction, overall patient satisfaction with the treatment process and cosmetic results, and the incidence of Frey syndrome. Outcomes with the transparotid and submandibular approaches were compared using the Mann–Whitney U test for continuous variables and the χ2 or Fisher exact test for categorical variables, with significance level set at p < 0.05 (2-tailed).
Results:
Data were collected from the charts of 32 patients who met the eligibility criteria during the study period; 14 of these patients also underwent an in-person assessment (at 1 to 7 years after the surgery). Statistical analysis of data from the chart audit and in-person assessment suggested no difference between the 2 approaches in terms of surgical outcomes after condylar fractures.
Conclusions:
The optimal approach for treatment of condylar fractures should be determined individually, based on the surgeon’s preference, fracture location and extent of the fracture.
Introduction
Oral and maxillofacial surgeons commonly treat mandibular fractures. Condylar fractures account for roughly 24% of mandibular fractures, presenting as a sole or secondary fracture, depending on the mechanism of injury.1 The mandibular condyle is subdivided into 3 regions: the condylar head, condylar neck and subcondylar region1 (Fig. 1); fractures can occur in any of these areas.
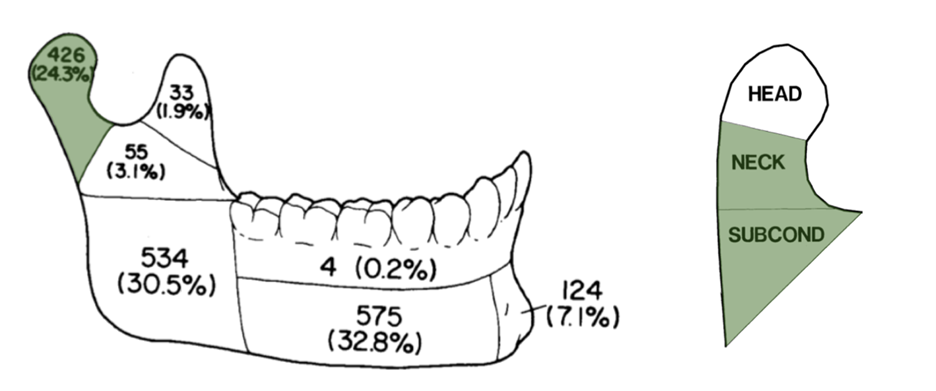
Figure 1: Prevalence of mandibular fractures and regions of the mandibular condyle. HEAD = condylar head; NECK = condylar neck; SUBCOND = subcondylar region.
Fractures can be classified with the Spiessl and Schroll system, where they are categorized by degree of displacement and height of the fracture.2 Type I fractures are nondisplaced or minimally displaced and are typically treated with a closed approach, which involves rigid maxillomandibular fixation to prevent excessive jaw movement and allows the bone to heal indirectly through callus formation. If the fracture is excessively displaced or dislocated (Spiessl and Schroll types II–V), the decision may be made to treat it by open reduction and internal fixation (ORIF). The condylar fractures most commonly treated with ORIF are type II (low fractures with displacement) and type IV (low fractures with dislocation).2 In ORIF, the general concept is that an incision is made to expose the fracture site, the fracture is reduced, and surgical plates are placed to fix the fracture.1,3 In the current study, we focused solely on cases in which ORIF approaches were used to treat condylar fractures.
Multiple ORIF approaches are available to treat condylar fractures; however, the 2 most commonly used at our centre are the transparotid (TP) and submandibular (SM) approaches. The incision for the TP approach is made inferior to the ear lobe and parallel to the posterior border of the ramus.4 The incision for the SM approach is made near the angle of the mandible and parallels the inferior border of the mandibular body4 (Fig. 2a and 2b). Other approaches include the preauricular approach, commonly used in temporomandibular joint surgery, where an incision is made in the natural crease just anterior to the auricle, and the intraoral approach, which is usually reserved for very low subcondylar fractures due to the relatively difficult visualization.
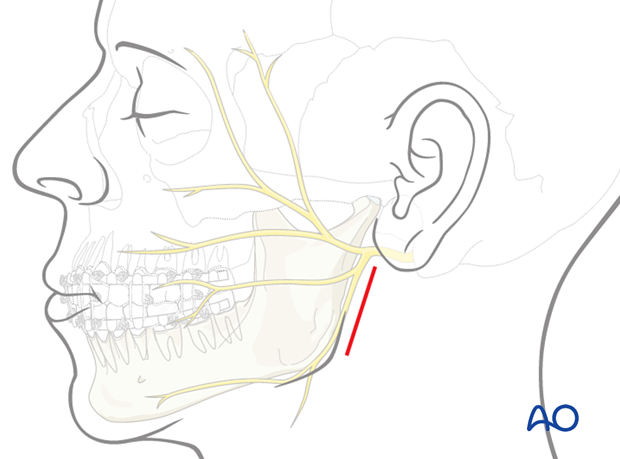
Figure 2a: Schematic of incisions for a transparotid approach. The red line indicates an example fracture site. Adapted, with permission, from AO Foundation. Available: aofoundation.org
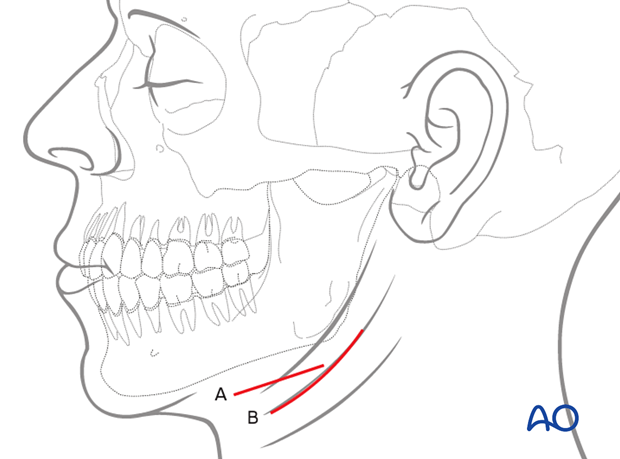
Figure 2b: Schematic of incisions for a submandibular approach. Labels “A” and “B” are different incision designs for a submandibular approach. Adapted, with permission, from AO Foundation. Available: aofoundation.org
The main benefit of a TP approach is proximity to the area of the fracture, which makes plate fixation easier.5,6 A TP approach also facilitates the placement of more than one fixation plate at optimal angles, maximizing stability. However, the smaller incision may make visualization of the fracture more difficult.5,6 The greatest drawback of the TP approach is proximity to the facial nerve trunk, which increases the risk for iatrogenic nerve damage.7 In contrast, although the incision for an SM approach is further from the facial nerve trunk, it is also further from the area of the fracture, making fixation of the plates more difficult.4
It is currently unclear whether the TP or the SM approach yields better surgical results with fewer postoperative complications. In this study, we investigated which of the 2 approaches yields better surgical outcomes, with fewer postoperative complications, with the ultimate goal of determining which can be regarded as the more favourable approach for future surgeries.
Methods
Study Design
Our retrospective cohort study was conducted in 2 parts: a retrospective chart audit and an in-person assessment. Participants were selected from all patients who presented to the Queen Elizabeth II Health Sciences Centre (Halifax) between January 1, 2012, and January 1, 2022, with condylar fracture treated with ORIF. Patients were included if they had a unilateral condylar or subcondylar fracture that was treated by a TP or SM approach. Patients were excluded if they had bilateral fractures, fractures that were not treated with ORIF or fractures that were not treated by a TP or SM approach; patients who were missing at the time of postsurgical follow-up and those who passed away postoperatively were also excluded. All information for the chart audit was collected from the second-week follow-up appointment. This time point was selected because 2 weeks is a required follow-up period (as per department protocol), it allowed for the greatest number of participants, and it was deemed to have allowed for an appropriate amount of initial soft-tissue healing.
All patients in the chart audit group were contacted to participate in an in-person assessment; patients who were unable to attend the in-person assessment were excluded from that portion of the study. Figure 3 outlines the study design and participant selection process in more detail. All in-person participants received compensation, as approved by the institutional research ethics board.
Study protocol and ethics approval was obtained from the Nova Scotia Health (NSH) Research Ethics Board (#1027886), which allowed us to collect nonidentifiable personal health information. Patients who met the inclusion criteria were contacted to obtain their informed consent for a more thorough review of their chart. Patients who consented to participate in the in-person assessment signed an informed consent form at the time of the study, as approved by the NSH Research Ethics Board.
Variables
The predictor variable for this study was treatment of condylar fracture using either a TP or SM approach, as previously defined.
The retrospective chart audit portion of the study explored maximum interincisal opening (MIIO), paresthesia, motor weakness, postoperative infection and changes from preoperative occlusion as outcome variables. The MIIO was defined as the distance from the incisal edge of the most extruded maxillary central incisor to the incisal edge of the most extruded mandibular central incisor when the patient’s mouth was open as wide as was comfortably possible. Paresthesia was defined as loss of normal sensation of the skin overlying areas innervated by the trigeminal nerve and/or the superficial cervical plexus of veins. Motor weakness at 2 weeks after surgery was defined as weakness of the muscles of facial expression that are innervated by the facial nerve. Postoperative infection was defined as the presence of any of the cardinal signs of infection not attributable to motor weakness or the normal swelling expected after surgery. Changes from preoperative occlusion were defined as grade 1, where there was recovery to preinjury occlusion (as stated by the patient), or grade 2, where there was mild malocclusion requiring prosthodontic or orthodontic treatment.
The in-person assessment involved determination of paresthesia, postoperative infection and changes from preoperative occlusion, as defined above, as well as assessment of Frey syndrome, motor weakness, patient and observer scar satisfaction, and overall patient satisfaction. Frey syndrome is a rare neurologic condition in which mastication induces hidrosis and facial flushing because fibres of the glossopharyngeal nerve have been damaged during dissection through the parotid gland.8 The TP approach involves gross dissection through the parotid gland, and Frey syndrome may thus be more prevalent with that approach. Motor weakness at the time of the in-person assessment was defined as reduction or complete loss of function of the muscles of facial expression innervated by the facial nerve and was assessed using the House–Brackmann scale (as outlined in Table 1).9 This scale was selected because it has been considered the benchmark for a simple, validated and reliable test to assess facial nerve damage.10 Patient and observer satisfaction with healing of the scar was based on the Patient and Observer Scar Assessment Scale (POSAS), version 2.0.11 The POSAS is a validated tool that has been used worldwide to assess scarring in surgical patients.11 Finally, overall patient satisfaction was defined as the patients’ satisfaction with the treatment process, including the surgery, postsurgical care and overall results. To date, the literature contains only limited studies with similar outcomes assessing patients’ attitudes toward and satisfaction with the surgery itself.
|
Grade |
Description of weakness |
Measurement of displacement (mm) |
Function (%) |
Estimated function (%) |
|---|---|---|---|---|
| I | Normal | 8/8 | 100 | 100 |
| II | Slight | 7/8 | 76–99 | 80 |
| III | Moderate | 5/8 or 6/8 | 51–75 | 60 |
| IV | Moderately severe | 3/8 or 4/8 | 26–50 | 40 |
| V | Severe | 1/8 or 2/8 | 1–25 | 20 |
| VI | Total | 0/8 | 0 | 0 |
Additional variables assessed in this study (which were used to exclude the possibility of confounding variables) were age, sex, side of the fracture (left or right), location of the fracture (subcondylar or condylar), number of fixation plates used, smoking, alcohol consumption and diabetes. Smoking and alcohol consumption were defined as the use of any amount of the substance(s) at the time of surgery. Diabetes was defined as prior diagnosis of type 1 or type 2 diabetes mellitus with no resolution at the time of the surgery.
Data Collection
To measure MIIO, the patient was asked to open their mouth as wide as possible without assistance. A ruler was then zeroed at the incisal edge of the mandibular central incisors. The measurement was taken at the level of the incisal edge of the maxillary central incisors, with the ruler resting gently on the teeth, without any bends.
Paresthesia was assessed using the cotton wisp test. This involved using a cotton ball and, with the patient’s eyes closed, lightly touching different areas of the face that correspond with the various sensory nerves in the maxillofacial region. The patient was then asked whether they felt anything. To further increase the validity of this test, the patient was also asked if they felt anything without the investigator having touched any area of their face. Paresthesia was documented as being absent or present, depending on whether the patient did or did not feel the cotton wisp, respectively.
As indicated above, motor weakness was assessed using different methods in the 2 parts of the study. For the chart audit portion, motor weakness was assessed as present or absent based on objective findings during the 2-week follow up appointment. This assessment would have involved asking the participant to perform a variety of movements involving the muscles of facial expression. For the in-person assessment portion of the study, the House–Brackmann scale was used to assess weakness of the facial nerve.9 This method involves placing a measurement device with 1-mm markings at the labial commissures and the upper eyelid on each side of the face and asking the participant to smile and lift their eyebrows, respectively. Total displacement is measured for both the mouth and the eye and is evaluated over a maximum total of 8 mm. A score of 8/8 indicates a normal nerve with 100% function.
In the chart audit portion of the study, infection was defined as the presence of any of the cardinal signs of infection (redness, warmth, swelling, pain, loss of function) that were not attributable to motor weakness. Swelling after surgery is normal because of increased postoperative vascularity in the area. If swelling persisted or worsened, and was associated with increased pain and redness, it was considered an infective process. During the in-person assessment, participants were asked if they had experienced any of the cardinal signs of infection after their follow-up appointments, and their responses were cross-referenced with the postoperative chart notes.
Given that participants would likely have presented to the hospital with a malocclusion due to their injury, the preoperative and postoperative chart notes, as well as participants’ descriptions of their teeth before injury, were reviewed to ensure the accuracy of our findings.
Frey syndrome was assessed by asking patients whether they experienced abnormal or increased hidrosis during mastication, compared to the preoperative situation.
The POSAS was used to assess both the participant’s and the examiner’s satisfaction with the scar. The examiner collecting the data was trained in using the POSAS by an oral and maxillofacial surgeon familiar with the tool; this examiner(MA) was the sole examiner for all in-person assessments. For each patient, the examiner assigned a score from 0 to 9 for each element of the easy-to-use tool, then summed and averaged the individual scores to generate a final score between 0 and 9.
Overall patient satisfaction was measured objectively by asking patients “on a Likert scale of 1 to 10, how satisfied are you with your surgery, including the presurgical care, the surgery itself, and the postsurgical care and results?”
Data Analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS), version 27 (IBM, Armonk, NY), with significance level set at p < 0.05 (2-tailed). Data were checked for normality. Differences between the TP and SM groups were analyzed using the Mann–Whitney U test for continuous variables or the χ2 test for categorical variables (or the Fisher exact test when more than 20% of the cells contained expected frequencies of less than 5).
Results
A total of 275 patients presented to the study hospital with condylar fracture during the study period. Of these, 32 met the eligibility criteria and were included in the chart audit, as outlined in Fig. 3. Fourteen of these patients were available to attend an in-person assessment, all between 1 and 7 years from the date of their surgery.
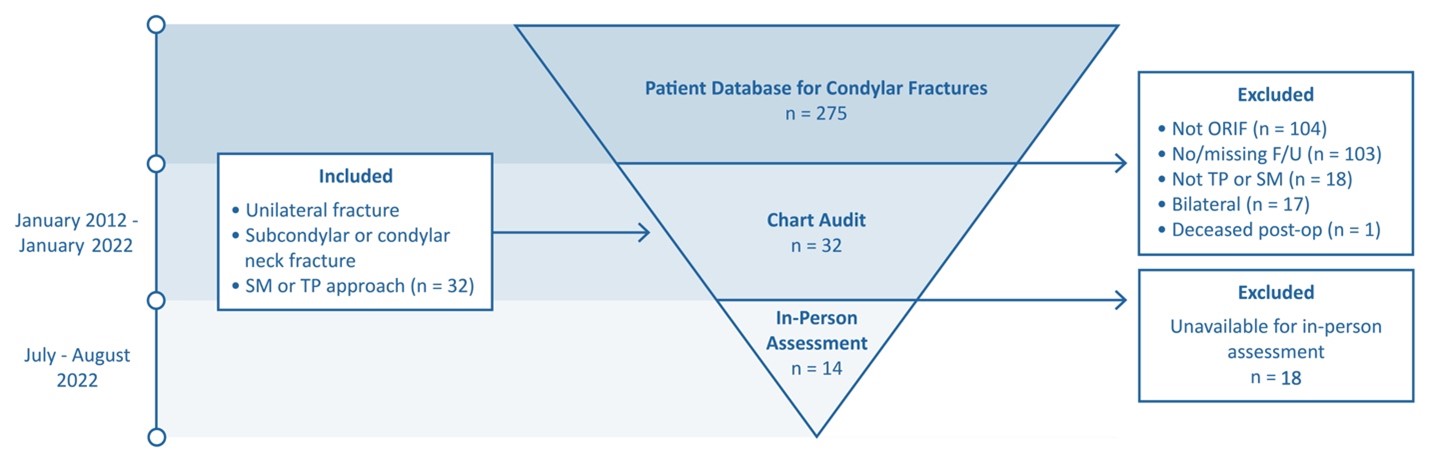
Figure 3: Study design and participant selection process. The cause of the sole postoperative death was due to complications unrelated to treatment of condylar fracture. F/U = follow-up; ORIF = open reduction and internal fixation; post-op = postoperatively; SM = submandibular; TP = transparotid.
The characteristics of the study participants are summarized in Table 2. The median age of participants was 37.0 years (range 14 to 68 years). The majority were male (88%), most presented with subcondylar fractures (88%), and most required 2 plates (94%). Left and right fractures were about equally represented. Most participants self-reported that they smoked (63%) and consumed alcohol (80%). None of these factors differed significantly between the SM and TP groups (p > 0.05), which indicated a lack of confounding factors for these variables within our sample.
|
Characteristic |
Group; no. (%) of patientsa,b |
p value |
||
|---|---|---|---|---|
|
All n = 32 (100) |
Submandibular approach |
Transparotid approach |
||
|
Note: NA = not applicable. |
||||
| Age (years) | 0.69 | |||
| Median | 37.0 | 36.0 | 38.5 | |
| Range | (14–68) | (19–68) | (14–61) | |
| Sex | 0.61 | |||
| Male | 28 (88) | 15 (54) | 13 (46) | |
| Female | 4 (12) | 3 (75) | 1 (25) | |
| Side | 0.69 | |||
| Left | 17 (53) | 9 (53) | 8 (47) | |
| Right | 15 (47) | 9 (60) | 6 (40) | |
| Location | > 0.99 | |||
| Subcondylar | 28 (88) | 16 (57) | 12 (43) | |
| Condylar neck | 4 (12) | 2 (50) | 2 (50) | |
| No. of plates | > 0.99 | |||
| 1 | 2 (6) | 1 (50) | 1 (50) | |
| 2 | 30 (94) | 17 (57) | 13 (43) | |
| Smoking habit | 0.20 | |||
| Yes | 20 (62) | 13 (65) | 7 (35) | |
| No | 12 (38) | 5 (42) | 7 (58) | |
| Alcohol consumptionc | > 0.99 | |||
| Yes | 24 (80) | 14 (58) | 10 (42) | |
| No | 6 (20) | 4 (67) | 2 (33) | |
| Diabetes mellitus (type 1 or type 2) | NA | |||
| Yes | – | – | – | |
| No | 32 (100) | 18 (56) | 14 (44) | |
Table 3 outlines the data collected from the chart audit portion of our study. The outcomes of MIIO, paresthesia, motor weakness and change in occlusion were similar with the SM and TP approaches (p > 0.05). No postoperative infection was reported for any patient in either group.
|
Characteristic |
Group; no. (%) of patientsa,b |
p value |
||
|---|---|---|---|---|
|
All n = 32 (100) |
Submandibular approach |
Transparotid approach |
||
|
Note: NA = not applicable; SD = standard deviation. |
||||
| Maximum interincisal opening (mm), mean ± SD | 27.2 ± 8.4 | 26.1 ± 8.0 | 28.3 ± 9.2 | 0.58 |
| Paresthesia | 0.67 | |||
| No | 26 (81) | 14 (54) | 12 (46) | |
| Yes | 6 (19) | 4 (67) | 2 (33) | |
| Motor weakness | 0.10 | |||
| No | 27 (84) | 13 (48) | 14 (52) | |
| Yes | 5 (16) | 5 (100) | 0 (0) | |
| Infection | ||||
| No | 32 (100) | 18 (56) | 14 (44) | NA |
| Yes | – | – | – | |
| Change from preoperative occlusion | > 0.99 | |||
| Grade 1 | 27 (84) | 15 (56) | 12 (44) | |
| Grade 2 | 5 (16) | 3 (60) | 2 (40) | |
Similarly, the outcomes measured during the in-person assessments did not differ significantly between the 2 approaches (Table 4). As with the chart audit (based on follow-up 2 weeks after surgery), paresthesia, motor weakness and change from preoperative occlusion were similar between the 2 groups at the in-person assessments up to 7 years after surgery. No infections or cases of Frey syndrome were reported with either approach. Finally, POSAS scores and overall satisfaction were similar in the 2 groups.
|
Characteristic |
Group; no. (%) of patientsa,b |
p value |
||
|---|---|---|---|---|
|
All n = 14 (100) |
Submandibular approach |
Transparotid approach |
||
|
Note: IQR = interquartile range; NA = not applicable. |
||||
| Paresthesia | 0.67 | |||
| No | 12 (86) | 3 (25) | 9 (75) | |
| Yes | 2 (14) | 2 (100) | 0 (0) | |
| Infection | NA | |||
| No | 14 (100) | 5 (36) | 9 (64) | |
| Yes | – | – | – | |
| Change from preoperative occlusionc | > 0.99 | |||
| Grade 1 | 11 (85) | 3 (27) | 8 (73) | |
| Grade 2 | 2 (15) | 2 (100) | 0 (0) | |
| Frey syndrome | NA | |||
| No | 14 (100) | 5 (36) | 9 (64) | |
| Yes | - | - | - | |
| Motor weakness (mm), median (IQR) | 8.0 (7.0-8.0) | 8.0 (7.0–8.0) | 8.0 (8.0-8.0) | 0.61 |
| Patient scar satisfaction,d median (IQR) | 8.0 (4.5–9.0) | 7.0 (3.0–9.0) | 9.0 (5.5–9.0) | 0.61 |
| Observer scar satisfaction,d median (IQR) | 7.0 (5.8–9.0) | 7.0 (6.0–8.0) | 7.0 (1.5–9.0) | 0.90 |
| Overall patient satisfaction,e median (IQR) | 9.5 (8.4–10.0) | 8.0 (7.8–10.0) | 10.0 (9.0–10.0) | 0.24 |
Discussion
The objective of this retrospective study was to determine whether a TP or SM approach yields better surgical results, with fewer postoperative complications, in treating patients with unilateral subcondylar or condylar neck fractures. Using a retrospective chart audit and an in-person assessment, we were able to evaluate certain variables that have been established in the literature as being of importance in the treatment of patients with condylar fracture.
Comparison of the outcomes measured in each portion of the study did not establish the superiority of either approach, given that the observed differences were not statistically significant. As such, there is insufficient evidence to suggest that either the TP or the SM approach yields better outcomes with fewer postoperative complications. However, the chart review showed that 28% of patients in the SM group but none of those in the TP group had motor weakness at the 2-week postsurgical follow-up (Table 3). Although the TP approach is usually noted in the literature as being associated with an increased incidence of iatrogenic facial nerve damage,7 a few factors might have affected the results in our study. For example, surgical technique might have been a factor, if the facial nerve was identified and better protected with the TP approach. Conversely, the relatively inferior location of a fracture, with possible damage to the facial nerve, might have prompted use of the SM approach, or there may have been damage to the marginal mandibular branch of the facial nerve (which can be damaged with less force than is needed to harm the larger branches closer to the facial nerve trunk). Nevertheless, all patients showed near-complete recovery by the time of the in-person assessment.
Other studies have reported the clinical follow-up results of a single surgical approach or have examined slightly different outcomes (e.g., closed reduction versus ORIF).12,13 Our study, however, compared the outcomes of different soft-tissue approaches for ORIF of condylar fractures. Ebenezer and Ramalingam4 compared approaches for rigid fixation of subcondylar fractures (n = 5 per group) and reported similar results to ours, specifically, no statistically significant differences between the groups.
Eckelt and others14 showed that although ORIF is superior to closed reduction techniques for condylar fractures, the type of internal fixation had no effect on treatment outcome. This conclusion aligns with our findings. In their meta-analysis, Al-Moraissi and Ellis15 also concluded that surgical treatment is superior to and yields better outcomes than closed reduction. However, Ellis and Dean3 noted anecdotally that the retromandibular approach, a variant of the TP approach, is most reliable. Some authors have even argued that surgeons must consider whether open treatment (i.e., ORIF) is indicated at all, given its higher complication rate compared with closed reduction, especially for higher and more complex fractures of the condyle.16 In fact, Devlin and Hislop17 suggested a more comprehensive consent form to cover the increased risk and higher complication rates inherent to ORIF for condylar fractures.
Our study employed a larger sample size than previous similar studies; however, there is a possibility of type II error due to lack of sufficient power. A low response rate and loss to follow-up limit the generalizability of the results; however, for these types of studies, it is difficult to obtain and follow larger numbers of patients. Our study, which consisted of a chart review and in-person assessment, provides 2 perspectives using similar data; we were thus able to assess both short- and long-term progression of outcomes. The use of validated tools, such as the House–Brackmann scale and the POSAS, provided high-quality data. We believe that patient satisfaction is a crucial aspect of overall surgical success, since patients are the ones living with the surgical results, and we stressed the importance of patient satisfaction through evaluation of several variables. Although our study used several objective measures, some of the data were self-reported, and those findings may be vulnerable to bias. Due to the nature of follow-up at our institution, there may be interobserver variability bias in the chart audit portion of this study. This potential bias stems from multiple surgeons and residents assessing patients postoperatively without appropriate calibration. Therefore, the results should be interpreted with caution.
Future iterations of this study could include analysis of the formation of salivary fistulas with the TP approach, given close proximity of the parotid gland and duct to the surgical site. Loss of ramus height could also be assessed. Furthermore, the use of intraoperative imaging might be beneficial to verify the accuracy of fracture reduction. In the current study, results of intraoperative imaging were not available for analysis because such imaging is not a standard of practice at our institution; rather, imaging is completed at patients’ follow-up appointments. Moreover, it may be beneficial to assess the time required to access the surgical site with each approach; it is expected that the TP approach would be faster, as it is closer to the site of the fracture. Finally, it may be helpful to evaluate the need for revision surgeries with each approach, whether for the fixation itself or the scarring.
Conclusion
We conclude that the best approach to repair of a condylar fracture is to be determined on an individual basis, taking into account the surgeon’s preference and the location and extent of the fracture. Schneider and others18 reached a similar conclusion, suggesting a tailored approach to the selection of surgical technique based on the location and severity of the fracture and patient-specific factors. We believe that a prospective study comparing the TP and SM approaches would provide more valuable output and validity. Furthermore, we have identified possible improvements that could be implemented into chart records for postoperative follow-up appointments to improve future data analyses. For example, sections specific to the degree of nerve function, specifically cranial nerves V and VII, MIIO and patient pain rating on a visual analogue scale could be added to the chart. These changes would allow for easy evaluation of patients’ progress during the healing period.
THE AUTHORS
Corresponding author: Dr. Mo Alabdoulsalam, 5981 University Ave, PO Box 15000, Halifax, NS B3H 4R2. Email: mo.a@dal.ca
Acknowledgements: The authors thank Dr. Leigha Rock for her expertise in statistical analyses, data processing and the publication process, as well as the Oral and Maxillofacial Department, Nova Scotia Health Authority, for the space and resources to conduct the study at a location suitable for the patients.
This article has been peer reviewed.
Funding provided by Canadian Association of Oral and Maxillofacial Surgeons in the form of a research grant that allowed patients to be compensated for their time and effort in participating in the study.
References
- Ellis E 3rd. Method to determine when open treatment of condylar process fractures is not necessary. J Oral Maxillofac Surg. 2009;67(8):1685-90. doi: 10.1016/j.joms.2009.03.062
- Spiessl B, Schroll K. Gelenkfortsatz und Gelenkköpfchenfrakturen. In: Spiessl B, editor. Gesichtsschädel. Stuttgart (Germany): Georg Thieme Verlag; 1972. pp. 58-99, 136-152.
- Ellis E 3rd, Dean J. Rigid fixation of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol. 1993;76(1):6-15. doi: 10.1016/0030-4220(93)90285-c
- Ebenezer V, Ramalingam B. Comparison of approaches for the rigid fixation of sub-condylar fractures. J Maxillofac Oral Surg. 2011;10:38-44. doi: 10.1007/s12663-010-0145-1
- Koirala U, Subedi S. Retromandibular transparotid approach for subcondylar mandibular fracture: A retrospective study. Dent Traumatol. 2021;37(2):314-20. doi: 10.1111/edt.12626
- Lee JS, Kang SH. Direct transparotid approach via a modified mini-preauricular incision for open reduction and internal fixation of subcondylar fractures. J Korean Assoc Oral Maxillofac Surg. 2021;47(4):327-34. doi: 10.5125/jkaoms.2021.47.4.327
- Shi D, Patil PM, Gupta R. Facial nerve injuries associated with the retromandibular transparotid approach for reduction and fixation of mandibular condyle fractures. J Craniomaxillofac Surg. 2015;43(3):402-7. doi: 10.1016/j.jcms.2014.12.009
- Motz KM, Kim YJ. Auriculotemporal syndrome (Frey syndrome). Otolaryngol Clin North Am. 2016;49(2):501-9. doi: 10.1016/j.otc.2015.10.010
- House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985;93(2):146-7. doi: 10.1177/019459988509300202
- Reitzen SD, Babb JS, Lalwani AK. Significance and reliability of the House-Brackmann grading system for regional facial nerve function. Otolaryngol Head Neck Surg. 2009;140(2):154-8. doi: 10.1016/j.otohns.2008.11.021
- van de Kar AL, Corion LUM, Smeulders MJC, Draaijers LJ, van der Horst CMAM, van Zuijlen PPM. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116(2):514-22. doi: 10.1097/01.prs.0000172982.43599.d6
- Klatt J, Pohlenz P, Blessmann M, Blake F, Eichhorn W, Schmelzle R, et al. Clinical follow-up examination of surgically treated fractures of the condylar process using the transparotid approach. J Oral Maxillofac Surg. 2010;68(3):611-7. doi: 10.1016/j.joms.2009.04.047
- Handschel J, Ruggeberg T, Depprich R, Schwarz F, Meyer U, Kubler NR, et al. Comparison of various approaches for the treatment of fractures of the mandibular condylar process. J Craniomaxillofac Surg. 2012:40(8):e397-401. doi: 10.1016/j.jcms.2012.02.012
- Eckelt U, Schneider M, Erasmus F, Gerlach KL, Kuhlisch E, Loukota R, et al. Open versus closed treatment of fractures of the mandibular condylar process – a prospective randomized multi-centre study. J Craniomaxillofac Surg. 2006;34(5):306-14. doi: 10.1016/j.jcms.2006.03.003
- Al-Moraissi EA, Ellis E 3rd. Surgical treatment of adult mandibular condylar fractures provides better outcomes than closed treatment: A systematic review and meta-analysis. J Oral Maxillofac Surg. 2015;73(3):482-93. doi: 10.1016/j.joms.2014.09.027
- Ellis E 3rd, McFadden D, Simon P, Throckmorton G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000;58(9):950-8. doi: 10.1053/joms.2000.8734
- Devlin MF, Hislop WS. Open reduction and internal fixation of fractured mandibular condyles by a retromandibular approach: Surgical morbidity and informed consent. Br J Oral Maxillofac Surg. 2002;40(1):23-5. doi: 10.1054/bjom.2001.0748
- Schneider M, Lauer G, Eckelt U. Surgical treatment of fractures of the mandibular condyle: A comparison of long-term results following different approaches—Functional, axiographical, and radiological findings. J Craniomaxillofac Surg. 2007;35(6):151-60. doi: 10.1016/j.jcms.2007.01.003


