Abstract
Objectives:
To investigate the impact of a COVID-19 mandated lockdown on the type and frequency of dental services accessed at an undergraduate dental clinic in southwestern Ontario.
Methods:
We retrieved anonymized sociodemographic (n = 4791) and billing data (n = 11616) of patients for 2 periods of 199 days, before (T1) and after (T2) lockdown. We applied descriptive statistics and used Student’s t test to compare the type and frequency of dental services provided between the 2 periods. We mapped forward sortation area (FSA) codes of each patient.
Results:
Of the 4791 patients seen collectively in T1 and T2, most (67%) sought care before the lockdown. In both periods, most patients were ≥ 60 years of age (51.8%), female (33.9%) and residing in an urban area (88.6%). Compared with T1, there was a significant increase in middle-aged adults (p = 0.002) and significantly fewer patients earning over CAD 100 000 (p = 0.021) in T2. A total of 11616 billable procedures were carried out during T1 and T2: in T1, most procedures were preventative, whereas in T2, most were related to urgent care. Significantly fewer males than females sought urgent care, regardless of time. Finally, mapping showed a decrease in patients from Toronto, central and northern Ontario and clustering of patients in southwestern Ontario.
Conclusions:
We noted an overall reduction in billed services following the COVID-19 lockdown. The decrease in both billed services and patients seen during T2 demonstrates the impact of COVID-19 on access to timely and definitive dental care during the first 2 years of the pandemic.
On 11 March 2020, the World Health Organization classified COVID-19 as a pandemic.1 As of 19 August 2022, the number of cases in Canada had reached 4 135 607, with Ontario reporting the highest count among all 8 jurisdictions at 1 392 435 cases.2 The community spread of a virus can be measured by the rate of positive tests: as of June 2022, 64 092 283 tests had been performed with 12.4% of them positive.2
Given the high infection rates of the virus, on 20 March 2020, the Royal College of Dental Surgeons of Ontario (RCDSO) strongly recommended the suspension of all non-essential and elective dental services.3 Recall examinations, routine dental cleanings, extraction of asymptomatic teeth, restorative dentistry, including treatment of asymptomatic carious lesions, and cosmetic dentistry constituted non-essential care.4 Furthermore, because of the presumed airborne transmission of the virus,5 the Centers for Disease Control and Prevention (CDC) in the United States strongly recommended delaying dental procedures involving the use of aerosols, such as those using high-speed handpieces, air/water syringes and ultrasonic scalers.6
The imposition of new guidelines had consequences for the frequency of services provided during the pandemic across the health care sector. Decreases were seen in hospital admissions, diagnostics services and therapeutics.7 One Canadian study8 reported a 17% decrease in tooth extractions, a 17% decrease in silver diamine fluoride application and a > 80% reduction in endodontic and restorative treatments, compared with a period before the pandemic (2019). Visits to community and hospital-based dental clinics also decreased.9
One area affected by the restrictions on the use of aerosol-generating procedures (AGPs) was endodontics. Without high-speed handpieces to carry out traditional endodontic treatments, practitioners turned to non-AGPs and pharmacologic intervention to manage endodontic emergencies.10 In some cases, patients found palliation insufficient to manage their pain and opted for extraction.10 Other adverse effects of delayed dental treatments included tooth fracture, lost provisional restorations and recurring infections.10
Moreover, the pandemic had adverse effects on dental care providers. Dental professionals were initially thought to be at higher risk of contracting COVID-19.11 A study looking at dental practitioners in 30 countries found that 87% reported fears regarding contracting COVID from either a patient or co-worker.12 Among these dentists, 2/3 wanted to close their practice until the number of infected individuals in their region declined.12 Furthermore, a study of 10 117 nurses in British Columbia revealed a 10–15% increase in anxiety and depression among them at the start of the pandemic.13
Dentists were quick to adapt their provision of dental treatment by turning to teledentistry. The use of telephone triage, clinic questionnaires and body temperature measurements has been highlighted by some authors and encouraged by the CDC.6 Furthermore, remote consultations using messaging services (e.g., WhatsApp; Meta Platforms, Menlo Park, Calif., USA) have shown promise for monitoring patient conditions after oral surgery.14 A 2021 cross-sectional study found 49.3% of dentists reporting use of teledentistry15; 36% of dentists cited the pandemic as the reason for starting to use teledentistry for patient triage, consultations and education.15 This alternative means for evaluating patients post-operatively allowed the limiting of in-person clinical procedures for urgent cases only.
Finally, abundant reports describe various populations who experience barriers to access to oral health services. These include low socioeconomic groups, people living with HIV,16 senior adults,17 those with low literacy18 and the uninsured.19 It is noteworthy that populations who experience barriers are the same ones who are most vulnerable to contracting COVID-19.20
Therefore, we aimed to investigate the impact of a COVID-19 mandated lockdown on patients attending the undergraduate Schulich Dental School Clinic in southwestern Ontario by exploring the following factors before and after lockdown:
- Sociodemographic differences – specifically age, sex, location of residence, payment type and average household income
- Associations between patients’ sociodemographic characteristics and the provision of urgent dental care
- How the number of dental procedures (categorized into 8 disciplines) changed
- The geographic distribution of patients visiting the dental clinic to evaluate the influence of transportation and geographic radius on access to care
Methods and materials
For this retrospective study, we examined the electronic dental records of 4791 patients seen in the main clinic (adults) at the Schulich School of Dentistry. For this study, the patient population of a dental school clinic is of special interest because this group is typically overrepresented by those who experience many barriers to care, including cost.21
The records included demographic data, medical history, dental history, clinical examination results, radiographs, appointment records and a list of procedure codes billed to the patient and their associated date. Finally, geographic information was obtained by collecting the first 3 digits of a patient’s postal code — referred to as forward sortation area (FSA) codes.
Inclusion/Exclusion Criteria
Our study sample included all patients ≥ 19 years who meet the clinic’s eligibility criteria. For this study, we chose a time when the undergraduate clinic was operating before government-mandated lockdowns (T1) and a time when the clinic was operating after the lockdowns (T2). Comparisons between T1 and T2 were then made to see the effect of the lockdown on variables of interest.
In accordance with ministry of health guidelines, private practice dental clinics across Ontario were closed from 17 March to 15 June 2020. Therefore, we defined T2 as all dates from 15 June to 31 December 2020 (inclusive). To set T1 at the same length (199 days) and during the same season as T2, we defined T1 as 15 June to 31 December 2019 (inclusive).
Data Collection and Variable Construction
A single Excel file containing data from both T1 and T2 was generated (Microsoft, Redmond, Wash., USA) A list of all appointments completed, along with the date, was retrieved. Procedures were diagnostic, restorative, prosthodontic, emergency, oral surgery, preventative and endodontic in nature. A list of billing codes was extracted to compare the types of procedures performed in T1 and T2. Along with each appointment entry, we included the patient’s age, sex and FSA code. There was no identification of patients who came during both T1 and T2 or patients who came multiple times in a period. This design has been adopted in multiple current research studies investigating the impact of COVID-19 on patients.22-26
Data Organization
The procedure codes for each appointment were grouped into 9 undergraduate “clinic types” to differentiate treatments: 1. Complete exam, including diagnosis and treatment planning; 2. Restorative anterior, relating to direct anterior composite restorations; 3. Restorative posterior, relating to direct posterior composite restorations; 4. Prosthodontics, including both fixed and removeable appliances; 5. Emergency, relating to incision and drainage and emergency examinations; 6. Oral surgery, including simple and complicated extractions; 7. Preventative procedures, including scaling, debridement and prophylaxis; 8. Endodontics, including pulpotomy, pulpectomies and non-surgical root canal treatments; and 9. Miscellaneous.
Demographic data (age and sex) included 3 possibilities for sex (male, female and unstated) and 3 categories for age (18–29, 30–60 and > 60 years).
Data Analysis
We compared the number of patients seen and the number of procedure codes billed between T1 and T2. Specific data on the number of procedure codes billed for each clinic type were also analyzed. We divided dental procedures into 2 categories: urgent (emergency, endodontic and oral surgery procedures) and non-urgent (all others). The basis for including endodontic and oral surgery procedures in a single category called “urgent care” is supported by literature showcasing the prevalence of infection- and pain-related pathosis requiring root canal treatment or extractions. A study by Shqair and colleagues26 found that 79% of emergency visits were related to caries, with endodontic treatment the most frequent treatment of choice. Furthermore, a 4-year study observing 5333 patients attending an emergency department for dental pain found that, among patients who had a prior visit to the department, extraction was the most common treatment.27
Univariate analyses were calculated as frequencies and percentages for all variables. Bivariate analyses, using Χ2 tests and ANOVA, were conducted to determine the association between exposure variables (age category, sex, average household income, history of dental attendance and history of chronic medical conditions) and the outcome variable (dental clinic attendance during T1 and T2). Statistical significance was set at p < 0.05. We used simple bivariate analysis and did not account for any confounders. We used only full/complete billing records for T1 and T2. Hence, we did not incur the problem of missing data in this investigation.
Finally, the geographic distribution of patients was analyzed using FSA codes. First, the FSA codes were used to designate whether a patient was residing in a rural or urban area. As per the Government of Canada’s guidelines, the 2nd character in the FSA code denotes the area as urban or rural. A 0 indicates a wide-range rural and all other digits denote the region as urban. The FSA codes were also used to assign an average household income to each patient based on data from the 2016 Census from Statistics Canada28. Tables and figures were generated to present the differences in this variable among patients between T1 and T2. Finally, maps were created on ArcGIS software (v. 10.6.1; ESRI, Redlands, Calif., USA) to show a visual representation of patients’ distribution between T1 and T2.
Ethics approval
This study was approved by Western University’s Human Subjects Ethics Review Board (HSERB). The HSERB is registered with the US Department of Health & Human Services under Institutional Review Board registration number IRB 00000940.
Results
The first objective of this study was to investigate differences among patients — specifically with respect to age, sex, location of residence, payment type and average household income — between T1 and T2. Table 1 provides a summary of the sociodemographic characteristics of all patients seen at the Schulich dental clinic during these pre- and post-lockdown periods. Overall, 4791 patients sought care in the main dental clinic in both time periods, with the majority (3209, 67.0%) seeking care before the lockdown (T1). The mean age during T1 was 59.3 years, while in T2 it was 57.1 years. In both T1 and T2, most patients lived in urban areas (89% and 90%, respectively) and were not enrolled in government subsidy programs (97.8% and 97%). Significantly more 30–60-year-old patients attended the clinic during T2. Significantly, fewer patients earning over CAD 100 000 visited during T2 compared with T1 (p = 0.021)
|
Variable |
Patients, no. (%) |
|||
|---|---|---|---|---|
|
T1 (n = 3209) |
T2 (n = 1582) |
Total (n = 4791) |
Χ2 (p) |
|
|
Note: Bold face p values indicate statistically significant differences. |
||||
| Age category | ||||
| 18–29 years | 373 (11.6) | 162 (10.2) | 535 (11.2) | 12.02 |
| 30–60 years | 1133 (35.3) | 639 (40.4) | 1722 (36.0) | (0.002) |
| > 60 years | 1703 (53.1) | 781 (49.4) | 2484 (51.8) | |
| Gender | ||||
| Female | 1277 (39.8) | 622 (39.2) | 1899 (39.6) | 3.37 |
| Male | 1012 (31.5) | 537 (33.9) | 1549 (32.3) | (0.185) |
| Unstated | 920 (28.7) | 423 (26.7) | 1343 (28.1) | |
| Location of residence | ||||
| Rural | 353 (11.0) | 158 (10.0) | 511 (10.7) | 1.14 |
| Urban | 2856 (89.0) | 1424 (90.0) | 4280 (89.3) | (0.285) |
| Payment method | ||||
| Government subsidy programs | 71 (2.2) | 48 (3.0) | 119 (2.5) | 2.95 |
| Other (i.e., out of pocket, private insurance, unknown) | 3138 (97.8) | 1534 (97.0) | 4672 (97.5) | (0.085) |
| Average annual household income, CAD | ||||
| 40 000–59 999 | 263 (8.2) | 129 (8.1) | 392 (8.2) | 7.74 (0.021) |
| 60 000–99 999 | 2082 (64.9) | 1085 (68.6) | 3167 (66.1) | 1230 (87.3) |
| ≥ 100 000 | 862 (26.8) | 367 (23.2) | 1229 (25.7) | |
| Unknown | 2 (0.1) | 1 (0.1) | 3 (0.1) | |
A second objective of this study was to investigate the association between patients’ sociodemographic status and the provision of urgent dental care during T1 and T2 (Table 2). Specifically, differences in age, sex and income levels were noted when it came to seeking out dental care between T1 and T2, highlighting the disproportionate effect of the COVID-19 pandemic on populations. More older patients sought non-urgent care in T1 than in T2 (p < 0.001). Significantly fewer males and more individuals who did not state their gender sought urgent care at the undergraduate clinic in T1 and T2 (p < 0.001). Significantly, fewer rural residents sought urgent dental care in T1 than in T2 (p < 0.001). Significantly more patients receiving government subsidies attended the clinic for non-urgent procedures during T2 (p = 0.036) than during T1. In addition, significantly fewer patients earning ≥ CAD 100 000 reported to non-urgent care during T2 compared with T1 (p = 0.029).
|
Variable |
Patients, no. (%) |
|||||
|---|---|---|---|---|---|---|
| T1 | T2 | |||||
|
Urgent |
Non-urgent |
Total |
Urgent |
Non-urgent |
Total |
|
|
Note: 1 = Urgent treatment, T1 vs. T2, 2 = Non-urgent treatment, T1 vs. T2, 3 = Urgent vs. non-urgent treatment during T1, 4 = Urgent vs. non-urgent treatment during T2. Bold face p values indicate statistically significant differences. |
||||||
| Age category | ||||||
| 18–29 years | 136 (14.2) | 237 (10.5) | 373 (11.6) | 68 (12.1) | 94 (9.2) | 162 (10.2) |
| 30–60 years | 422 (44.0) | 711 (31.6) | 1133 (35.3) | 232 (41.1) | 407 (40.0) | 639 (40.4) |
| > 60 years | 401 (41.8) | 1302 (57.9) | 1703 (53.1) | 264 (46.8) | 517 (50.8) | 781 (49.4) |
| Χ2 (p) | 3.91 (0.142)1 | 21.87 (0.001)2 | 69.65 (< 0.001)3 | 4.11 (0.128)4 | ||
| Gender | ||||||
| Female | 321 (33.4) | 956 (42.5) | 1277 (39.8) | 208 (36.9) | 414 (40.7) | 622 (39.3) |
| Male | 295 (30.8) | 717 (31.9) | 1012 (31.5) | 182 (32.3) | 355 (34.9) | 537 (33.9) |
| Unstated | 343 (35.8) | 577 (25.6) | 920 (28.7) | 174 (30.8) | 249 (24.4) | 423 (26.8) |
| Χ2 (p) | 3.97 (0.137)1 | 2.87 (0.238)2 | 38.03 (< 0.01)3 | 7.59 (0.022)4 | ||
| Location of residence | ||||||
| Rural | 67 (7.0) | 286 (12.7) | 353 (11.0) | 50 (8.9) | 108 (10.6) | 158 (10.0) |
| Urban | 892 (93.0) | 1964 (87.3) | 2856 (89.0) | 514 (91.1) | 910 (89.4) | 1424 (90.0) |
| Χ2 (p) | 1.77 (0.184)1 | 2.921 (0.087)2 | 22.51 (< 0.001)3 | 1.23 (0.268)4 | ||
| Payment | ||||||
| Government subsidy programs | 20 (2.1) | 51 (2.3) | 71 (2.2) | 12 (2.1) | 36 (3.5) | 48 (3.0) |
| Other (i.e., out of pocket, private insurance, unknown) | 939 (97.9) | 2199 (97.7) | 3138 (97.8) | 552 (97.9) | 982 (96.5) | 1534 (97.0) |
| Χ2 (p) | 0.000 (0.956)1 | 4.36 (0.036)2 | 0.102 (0.749)3 | 2.45 (0.117)4 | ||
| Average annual household income, CAD | ||||||
| 40 000–59 999 | 95 (9.9) | 170 (7.5) | 265 (8.3) | 43 (7.4) | 87 (9.5) | 130 (8.1) |
| 60 000–99 999 | 614 (64.0) | 1468 (65.2) | 2082 (64.9) | 387 (68.6) | 698 (68.6) | 1085 (68.7) |
| ≥ 100 000 | 250 (26.1) | 612 (27.2) | 862 (26.8) | 134 (23.7) | 233 (22.9) | 367 (23.2) |
| Χ2 (p) | 3.93 (0.140)1 | 7.08 (0.029)2 | 4.97 (0.083)3 | 0.494 (0.781)4 | ||
A third objective was to investigate the types and changes in frequency of dental treatments provided between T1 and T2 (Figure 1). Overall, 11 616 procedures were billed in the 2 periods, with more (66.6%) billed for T1. During T2, the category with the highest proportion of billed procedures was urgent care (33.5%), whereas in T1 the highest proportion of procedures (34.3%) were preventative. Higher proportions of services billed in T2 than T1 were in the categories urgent care (33.5%), restorative anterior (9.5%), restorative posterior (21.3%) and prosthodontics (5.1%).
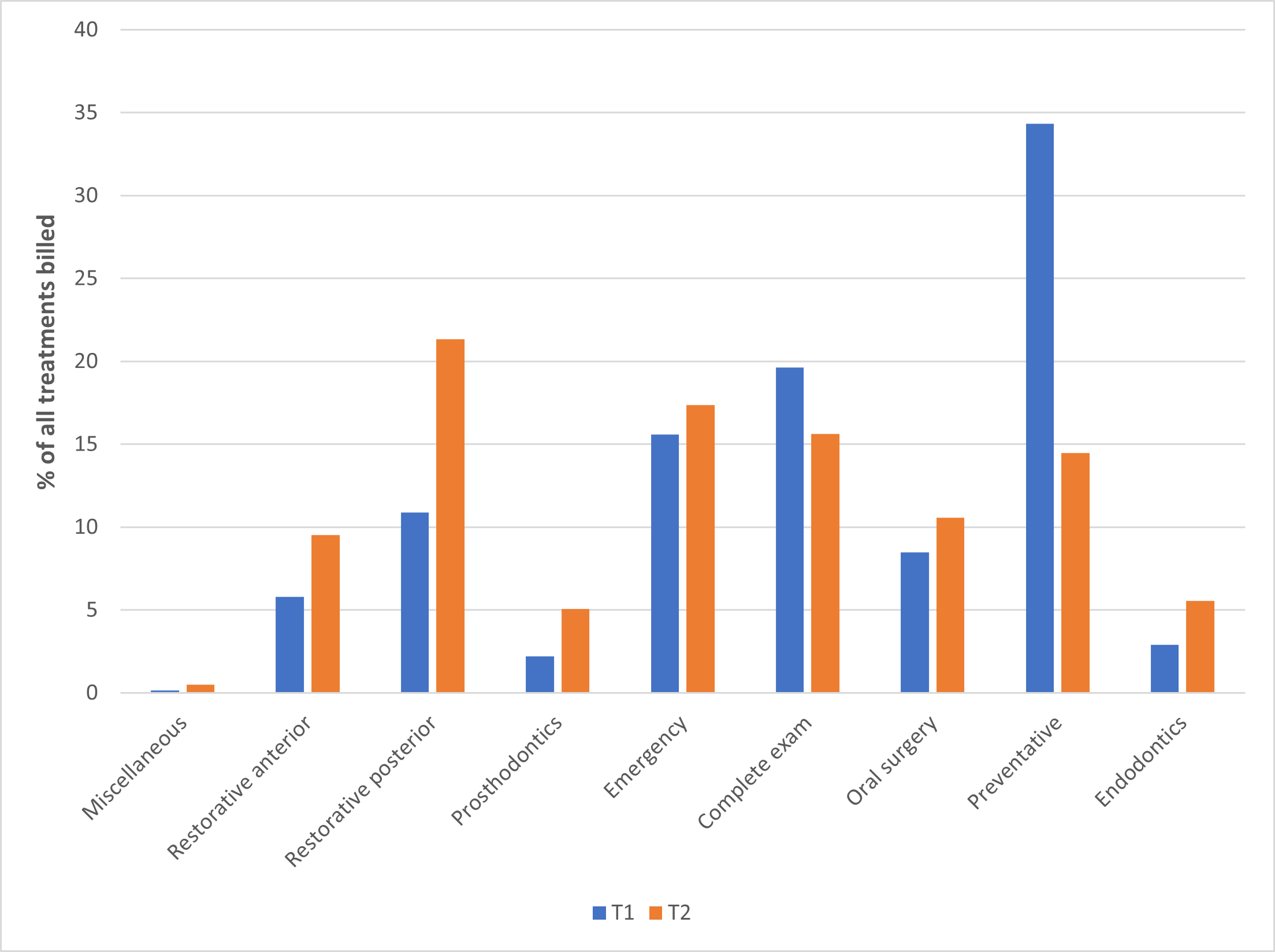
Figure 1: Comparison of treatments completed at an undergraduate dental clinic during a pre-lockdown period (T1, n = 3209) and a post-lockdown period (T2, n = 1582).
Finally, we looked at the geographic distribution of patients during T1 and T2 to determine the influence of transportation and distance on access to care. First, comparing the maps between T1 and T2 show a marked decrease in total counts of patients seen in T2 with a larger portion of the map in T2 being uncoloured. Specifically, the total count of patients coming from the Greater Toronto Area (GTA), which includes Toronto, Peel and York Region public health areas, was reduced in T2 compared with T1. There was also a decrease in total patient counts arising from the Northeast of the province. In T1, the largest patient counts (shown in dark red) came from various areas in the Middlesex-London Health Unit, In T2, the same total patient count came from the central part of the Middlesex-London Health Unit where the undergraduate dental school was located (shown by black dots).
Discussion
This study aimed to investigate the effects of a COVID-19 mandated lockdown on the provision of dental care at an undergraduate dental clinic in southwestern Ontario. Our results align with similar studies showing that the pandemic shifted the sociodemographic characteristics of patients seeking dental care15 as well as the type29,30 and frequency23 of that care.
The number of patients visiting the dental clinic during a 199-day period after lockdown (1582) was a bit less than half the number visiting during a similar period before lockdown (3164), a finding that coincides with other studies.24,30,31 This decline may be attributed to fear among patients regarding the spread of COVID-19 in a dental setting. Ibrahim and colleagues32 reported that more than two-thirds of patients perceived a moderate to high risk of contracting COVID-19 through dental visits; those with a high level of self-reported fear of contracting COVID-19 were 6 times less likely to visit a dentist.33
The decrease in provision of dental care after lockdown can also be attributed to a decrease in clinic chairs and clinical staff available. One of the earliest changes caused by the pandemic was a decline in health care worker attendance.34 Absenteeism was reported to be especially high among nurses and ancillary workers.35 Guidelines set by the RCDSO during T2 stipulated that all AGPs were to take place in enclosed operatories.36 As most dental chairs at the undergraduate clinic were open operatories, this restriction significantly contributed to the decline in dental appointments available to patients. Furthermore, the requirement for fallow time between appointments to allow for clearance of aerosols further reduced clinic availability for patients. Community-acquired COVID-19 exposures and infections among caregivers (students, faculty, and staff) further reduced the provision of dental services during T2.37
The reduction in available dental care affected the type of dental treatments provided during and after the lockdown. There was an overall shift preventative and diagnostic treatments during T1 to more restorative and urgent care procedures in T2. A comparative study in Brazil showed a 1.4-fold decrease in preventative appointments, such as consultations, during COVID compared with pre-pandemic periods.38 Chisini and colleagues30 found a reduction of > 99% in preventative procedures but a minimal reduction in urgent care procedures during pandemic measures compared with an earlier period.
In our study, preventative procedures included debridement and prophylaxis with the use of ultrasonic scaling and air-water spray, which produce droplets and aerosols.39 Thus, the restrictions on and reduced capacity to perform AGPs during the pandemic explain the reduction in preventative procedures. Despite the barriers to accessing dental care during the pandemic, pain-driven dental visits did not decline.37 Our study found an increase in oral surgery and endodontic treatments post-lockdown which was consistent with the results of other similar investigaions.22,23 As expected, the data show that a reduction in access to care during the pandemic led to increased disease progression in the populations studied.
Most patients attending the undergraduate clinic during both periods were ≥ 60 years, female, residents of urban areas and not enrolled in a government subsidy program. As Canadian seniors are living longer, they are accumulating comorbidities that contribute to extensive oral health needs such as xerostomia, periodontal disease, root caries and poor oral hygiene resulting from dexterity issues.40,41 Because the elderly are least likely to be insured,42 subsidized health clinics, such as the undergraduate dental clinic, act as a hub for this patient population. The increased use of dental health services by the elderly has also been cited in other studies.43 Finally, the dominance of female patients using dental services has also been noted,31-33 with females being more likely to engage in health seeking behaviours than their male counterparts.44-46 More specifically, women are more likely to report oral pain than men.47 These gender differences in health seeking behaviours have been attributed to cultural expectations of gender roles48 and increased pain tolerance by men.49 Similar trends are seen in other studies showing men to be more reluctant to seek help for medical problems such as cancerous lumps,50 chest pain,51 and overall have fewer visits to the emergency department.
Comparing the provision of urgent care between the 2 periods, several significant findings are noteworthy. First, adults ≥ 60 years sought non-urgent care in both periods. A study by Hajek and colleagues52 concluded that delayed dental visits were positively associated with younger age, and the elderly were not as affected in terms of dental attendance during the pandemic. Data from the Canadian Community Health Survey45 showed that, although 68% of people in Ontario reported having dental insurance, this number declines to 36% among older adults. The undergraduate dental clinic fees are subsidized. This makes care at a dental school attractive to people with low or fixed income, including pensioners.
The location of patients’ residence was important, as this factor has been shown to affect access to care. For example, rural populations have an increased prevalence of both tooth loss and caries compared with metropolitan populations.53 The increased distance rural patients must travel to clinics comes with a transportation cost that has also been reported as a significant barrier to the use of dental services.54 Our results identified significant findings related to the location of residence and dental treatment provided during T1 and T2. Figures 2 and 3 show a reduction in patients from the GTA – one of the largest metropolitan areas in Ontario, with reduced dental attendance at the undergraduate dental clinic reported by Peel and Toronto public health units post pandemic. Meanwhile, other smaller health units either saw no change in patient attendance (e.g., Huron Perth Health Unit, Lambton Public Health, Region of Waterloo and Hamilton Public Health) or saw an increase (e.g., Middlesex-London Health Unit and Southwestern Public Health). The greater spread of COVID-19 in the GTA caused stringent lockdown restrictions, a plausible reason for the reduced dental attendance from this metropolitan area. In November 2020, the Ontario government categorized its 34 public health units based on community transmission rates: green (prevent), yellow (protect), orange (restrict), red (control), and grey (lockdown).55 Until this framework was eliminated in April 2021, Toronto and the Peel region remained continuously grey, while regions in southwestern Ontario were coded grey or red.55 Patients from the GTA consequently had more difficulty accessing dental services at the university clinic as evident from our geographic scan.
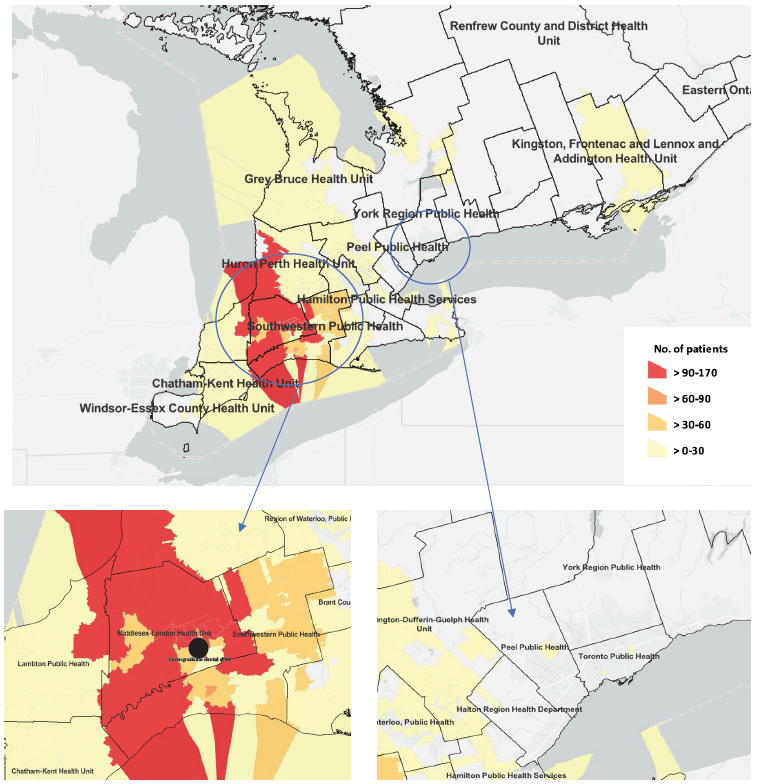
Figure 2: Distribution of patients at an undergraduate dental clinic by forward sortation code and public health county before COVID-19 lockdown (T1, n = 3209).
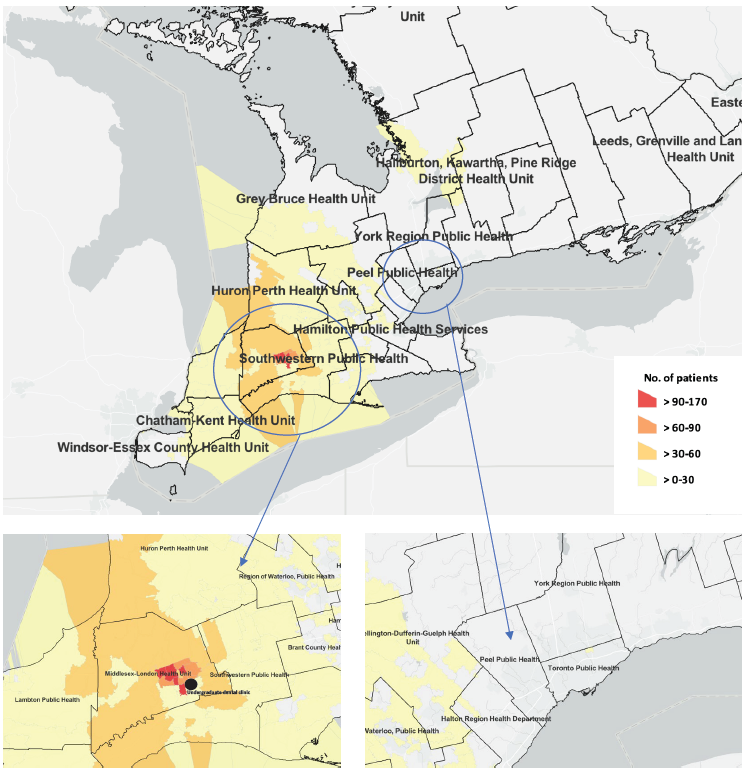
Figure 3: Distribution of patients at an undergraduate dental clinic by forward sortation code and public health county during COVID-19 lockdown (T2, n = 1582).
A decline in access to care has patient implications that have been well studied. Reduced access leads to late diagnosis and treatment, which can lead to serious odontogenic infections. Long and Corsar56 found a significant increase (35–80%) in hospital admissions resulting from dental abscesses. Furthermore, the reduced access to care seen during the pandemic also translated into increased prescription of antibiotics.57 Besides the burden on the hospital system and the complication of antibiotic resistance, delayed access to dental care has also been shown to lead to potentially life-threatening conditions. The progression of odontogenic infections during COVID-19 has been studied with specific cases reported of Ludwig’s angina, necrotizing fasciitis and peritonsillar abscesses.58 In all 3 cases, fear of COVID-19 was reported as the cause of delayed care.58
The main aim of this study was to investigate the effects of the pandemic on the provision of dental treatment in an undergraduate dental clinic. However, it is also important to address the implications of those effects for learners. During the pandemic, dental schools across Canada were operating on a limited basis under new IPAC guidelines in place. These changes included discontinuing preventative procedures, such as scaling, in 3 dental schools.59 One school resumed treatment but with added protective measures — increasing the preoperative set-up time.59 One school performed AGPs in enclosed rooms only.59 These changes have had direct effects on learners, with students reporting a reduced clinical experience, particularly in oral surgery, compared with their seniors who worked in non-pandemic times.60 Furthermore, although the number of student clinicians remained the same, the number of patients decreased (Table 1). This resulted in fewer cases for students to work on and learn from.
Direct patient care in clinical settings is essential for learners to achieve the competencies needed to work in their field. Hattar et al.61 showed that dental students expressed apprehension regarding their ability to work independently as a clinician because of the lack of one-on-one clinical experience. In a survey of 3348 medical students from 13 medical schools in Libya, 86% of students reported that their clinical training was suspended because of the COVID-19 outbreak.62 Most (69.6%) reported that the pandemic had affected the timeline of their training.
Although the RCDSO has lifted the requirement for closed AGP operatories and fallow time, these restrictions can be re-instated at any time and, hence, dental professionals should be fully prepared.63 Our study was conducted at an undergraduate dental clinic and can serve as a reference to encourage other undergraduate dental clinics to adopt new strategies to mitigate patient decline and to improve learning experience in anticipation of another breakout. Dental professionals must also face the added dilemma of “long COVID,” a term used to describe the persistence of symptoms in those previously recovered from the virus.64 The populations most vulnerable to COVID-19, and therefore long COVID, are the same ones that experience barriers to accessing oral health services: the immunocompromised,65 low socioeconomic groups, older adults, low-literacy individuals and the uninsured.20 Our study highlighted the role of transportation and geographic distance on access to care and, therefore, strategies to improve access to facilities should be explored. Furthermore, the dental workforce must also learn to balance existing dental anxiety along with the COVID anxiety that exists now.66
The pre- and post-lockdown periods we compared included only June to December, as the undergraduate dental clinic was closed from March to May 2020, and the pandemic had not yet been declared in January and February 2020. However, seasonal differences in dental treatments, such as increased frequency of dental trauma in winter months, have been reported in the literature.67 Our study is limited by the fact that it is retrospective and does not make any inference about current dental conditions and needs of patients. The pandemic continued past our timeframe for T2 and, thus, our study should be replicated for a more recent period (2022). Furthermore, the way our undergraduate dental clinic categorizes certain procedures may constitute a limitation. For instance, incision and drainage procedures were included in the endodontics category, whereas other academic institutions would term these “emergency” procedures. Despite these limitations, this is the first study of its kind in Canada to highlight the change in geographic distribution of patients seeking subsidized dental care before and during lockdown.
Other limitations to our study include the study of total count of patients rather than patient density for the geographical distribution and a patient population that may not be representative of the patient population accessing dental care in private practice. We also looked at the total number of procedures billed and number of patients in T1 and T2. However, a patient may have attended multiple appointments in either or both periods. We did not distinguish among these possibilities. The number of times the same patient had an appointment in each period could be examined in future studies to further determine the reasons for patients returning to the clinic.
Furthermore, although 1 of our objectives was to explore the association between patients’ sociodemographic characteristics and the provision of urgent care, it would be helpful to review those sociodemographic characteristics in T1 and T2 for each individual discipline. Finally, we acknowledge that root canal treatment, which was included in the category “urgent care,” can be performed in a non-urgent setting, such as iatrogenic pulpal exposure.
Several future directions can be taken to mitigate the challenges noted in this study, i.e., reduced access to care. Teledentistry is a viable means to address lack of access to care. For example, digital radiographs can be used by distant clinicians to diagnose periapical lesions in anterior teeth.68 Distant diagnosis using digital cameras and email has also been shown to be effective in treatment of oral lesions.69 Furthermore, the use of teledentistry is not new to the dental profession. In a 2023 study,15 49.3% of surveyed dentists reported using teledentistry. More than half of the respondents mentioned teledentistry as a viable means for triaging patients, not only for care but also for follow ups.15
Finally, a follow-up study, perhaps with a smaller sample size, can be conducted to examine which patients appeared both before and during lockdown and how the type of dental treatment they received changed between periods.
Conclusion
As we continue to navigate the pandemic, its impact on access to dental care is becoming apparent. This retrospective study adds to the body of knowledge showing reduced dental visits since the onset of the pandemic. It also shows a shift from preventative to more restorative and urgent care procedures after lockdown, highlighting the effect of delayed dental treatment. Anxiety among patients, limitations imposed by regulatory authorities and illness from COVID-19 among dental health care providers may have played a role in diminished access to oral health care as well as what type of services were provided and a subsequent observable escalation in the severity of disease. The importance of preventative approaches and timely management of existing dental diseases has been reinforced by data gathered before, during and after the height of the pandemic.
THE AUTHORS
Corresponding author: Dr. Abbas Jessani, Schulich School of Medicine and Dentistry, Western University, 1151 Richmond St, London ON N6A 3K7. Email: ajessani@uwo.ca
Acknowledgements: We thank Mr. Jon Oliva for facilitating data collection for this study.
This article has been peer reviewed.
The authors have no declared financial interests.
References
- WHO Director-General’s opening remarks at the media briefing on COVID-19 — 11 March 2020. Geneva: World Health Organization; 2020. Available: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed 2022 June 26).
- COVID-19 daily epidemiology update. Ottawa: Public Health Agency of Canada; 2020. Available: https://health-infobase.canada.ca/covid-19/?stat=num&measure=cases_total&map=pt#a2 (accessed 2022 June 28).
- RCDSO update — March 20, 2020 (COVID-19). Toronto: Royal College of Dental Surgeons of Ontario; 2020. Available: https://www.rcdso.org/en-ca/standards-guidelines-resources/rcdso-news/articles/5299 (accessed 2022 Aug. 21).
- Definitions of emergency, urgent and non-emergent and non-urgent care. Toronto: Royal College of Dental Surgeons of Ontario; 2022. Available: https://az184419.vo.msecnd.net/rcdso/pdf/standards-of-practice/RCDSO_COVID19_Definitions.pdf (accessed 2022 Aug. 22).
- Coronavirus disease (COVID-19): how is it transmitted? Geneva: World Health Organization; 2021. Available: https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-covid-19-how-is-it-transmitted (accessed 2022 June 27).
- Healthcare workers: dental settings. Atlanta: Centers for Disease Control and Prevention; 2020 Feb. 11.
- Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, To EJ, et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3)e045343.
- Rabie H, Figueiredo R. Provision of dental care by public health dental clinics during the COVID-19 pandemic in Alberta, Canada. Prim Dent J. 2021;10(3):47-54.
- Moharrami M, Bohlouli B, Amin M. Frequency and pattern of outpatient dental visits during the COVID-19 pandemic at hospital and community clinics. J Am Dent Assoc. 2022;153(4):354-64.e1.
- Patel B, Eskander MA, Ruparel NB. To drill or not to drill: management of endodontic emergencies and in-process patients during the COVID-19 pandemic. J Endod. 2020;46(11):1559-69.
- As Albertans return to work, who is at the highest risk of exposure to the novel coronavirus? Edmonton: Alberta Federation of Labour; 2020. Available: https://www.afl.org/as_albertans_return_to_work_who_is_at_the_highest_risk_of_exposure_to_the_novel_coronavirus (accessed 2022 Aug 22).
- Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health. 2020;17(8):2821.
- Havaei F, Smith P, Oudyk J, Potter GG. The impact of the COVID-19 pandemic on mental health of nurses in British Columbia, Canada using trends analysis across three time points. Ann Epidemiol. 2021;62:7-12v.
- Giudice A, Barone S, Muraca D, Averta F, Diodati F, Antonelli A, et al. Can teledentistry improve the monitoring of patients during the Covid-19 dissemination? A descriptive pilot study. Int J Environ Res Public Health. 2020;17(10):3399.
- Cheuk R, Adeniyi A, Farmer J, Singhal S, Jessani A. Teledentistry use during the COVID-19 pandemic: perceptions and practices of Ontario dentists. BMC Oral Health. 2023;23(1):72.
- Jessani A, Aleksejuniene J, Donnelly L, Phillips JC, Nicolau B, Brondani M. Dental care utilization: patterns and predictors in persons living with HIV in British Columbia, Canada. J Public Health Dent. 2019;79(2):124-36.
- Gaszynska E, Szatko F, Godala M, Gaszynski T. Oral health status, dental treatment needs, and barriers to dental care of elderly care home residents in Lodz, Poland. Clin Interv Aging. 2014;9:1637-44.
- Almutlaqah MA, Baseer MA, Ingle NA, Assery MK, Al Khadhari MA. Factors affecting access to oral health care among adults in Abha City, Saudi Arabia. J Int Soc Prev Community Dent. 2018;8(5):431-7.
- Locker D, Maggirias J, Quiñonez C. Income, dental insurance coverage, and financial barriers to dental care among Canadian adults. J Public Health Dent. 2011;71(4):327-34.
- Brian Z, Weintraub JA. Oral health and COVID-19: increasing the need for prevention and access. Prev Chronic Dis. 2020;17:E135.
- Haq M, Numekevor L, Singh P, Chisholm A. Community health profile southwestern Ontario. London: SouthWestern Academic Health Network; 2016. Available: https://www.swahn.ca/Uploads/ContentDocuments/CC%20license%20-%20Community%20Health%20Profile%20for%20Southwestern%20Ontario%20.pdf (accessed 2023 April 28).
- Nijakowski K, Cieślik K, Łaganowski K, Gruszczyński D, Surdacka A. The impact of the COVID-19 pandemic on the spectrum of performed dental procedures. Int J Environ Res Public Health. 2021;18(7):3421.
- Obeidat L, Masarwa N, AlWarawreh A, El-Naji W. Dental treatments during the COVID-19 pandemic in three hospitals in Jordan: retrospective study. Interact J Med Res. 2020;9(4):e24371.
- Guo H, Zhou Y, Liu X, Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 2020;15(4):564-7.
- Alshami ML, Abdulkareem AA, Gul SS, Shareef YA. Impact of COVID-19 on the frequency of dental appointments and types of dental health care services. Dentistry 3000. 2022;10(1).
- Shqair AQ, Gomes GB, Oliveira A, Goettems ML, Romano AR, Schardozim LR, et al. Dental emergencies in a university pediatric dentistry clinic: a retrospective study. Braz Oral Res. 2012;26(1):50-6.
- Okunseri C, Zbin S, Zheng C, Eichmiller F, Okunseri E, Szabo A. Emergency department visits and dental procedures: Mission of Mercy, 2013–2016. Clin Cosmet Investig Dent. 2019;11:157-62.
- Statistics Canada. Income of households in 2015 highlight tables, 2016 Census – forward sortation areas. Available https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=FSA&Code1=V5Y&Geo2=PR&Code2=01&Data=Count&SearchText=V5Y&SearchType=Begins&SearchPR=01&B1=All&TABID=2 (accessed April 28th, 2023).
- Meisha DE, Alsolami AM, Alharbi GM. Social determinants of seeking emergency and routine dental care in Saudi Arabia during the COVID-19 pandemic. BMC Oral Health. 2021;21(1):212.
- Chisini LA, Costa FDS, Sartori LRM, Corrêa MB, D’Avila OP, Demarco FF. COVID-19 pandemic impact on Brazil’s public dental system. Braz Oral Res. 2021;35:e082.
- Üstün N, Akgöl BB, Bayram M. Influence of COVID-19 pandemic on paediatric dental attendance. Clin Oral Investig. 2021;25(11):6185-91.
- Ibrahim MS, Alibrahim H, Al Madani A, Alamri A, Bamashmous M, Tounsi A. Fear factor in seeking dental care among Saudis during COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(20):10589.
- González-Olmo MJ, Ortega-Martínez AR, Delgado-Ramos B, Romero-Maroto M, Carrillo-Diaz M. Perceived vulnerability to Coronavirus infection: impact on dental practice. Braz Oral Res. 2020;34:e044.
- Do D, Sarker M, Chen S, Lenjani A, Tikka P, Bärnighausen T, Geldsetzer P. Healthcare worker attendance during the early stages of the COVID-19 pandemic: a longitudinal analysis of fingerprint-verified data from all public-sector secondary and tertiary care facilities in Bangladesh. J Glob Health. 2020;10(2):020509.
- Damery S, Wilson S, Draper H, Gratus C, Greenfield S, Ives J, et al. Will the NHS continue to function in an influenza pandemic? A survey of healthcare workers in the West Midlands, UK. BMC Public Health. 2009;9(1):142.
- Royal College of Dental Surgeons of Ontario. COVID-19: Managing infection risks during in-person dental care. Dispatch Magazine 2020;22 May. Available: https://www.rcdso.org/en-ca/rcdso-members/dispatch-magazine/articles/5347 (accessed 2023 Apr. 28).
- Walter E, von Bronk L, Hickel R, Huth KC. Impact of COVID-19 on dental care during a national lockdown: a retrospective observational study. Int J Environ Res Public Health. 2021;18(15):7963.
- de Oliveira MM, Fuller TL, Gabaglia CR, Cambou MC, Brasil P, de Vasconcelos ZFM, et al. Repercussions of the COVID-19 pandemic on preventive health services in Brazil. Prev Med. 2022;155:106914.
- Han P, Li H, Walsh LJ, Ivanovski S. Splatters and aerosols contamination in dental aerosol generating procedures. Appl Sci. 2021;11(4):1914.
- Seniors in transition: exploring pathways across the care continuum. Ottawa: Canadian Institute for Health Information; 2017. Available: https://www.cihi.ca/sites/default/files/document/seniors-in-transition-report-2017-en.pdf (accessed 2023 Oct. 23).
- Yao CS, MacEntee MI. Inequity in oral health care for elderly Canadians: part 1. Oral health status. J Can Dent Assoc. 2013;79:d114.
- Sadeghi L, Manson H, Quiñonez CR. Report on access to dental care and oral health inequalities in Ontario. Toronto: Public Health Ontario; 2013. Available: https://www.publichealthontario.ca/-/media/documents/D/2012/dental-oral-inequalities.pdf (accessed 2023 Oct. 23).
- Nasseh K, Vujicic M. Dental care utilization steady among working-age adults and children, up slightly among the elderly. Research brief. Chicago: Health Policy Institute; 2016. Available: https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/resources/research/hpi/hpibrief_1016_1.pdf (accessed 2023 Oct. 23).
- Reda SF, Reda SM, Thomson WM, Schwendicke F. Inequality in utilization of dental services: a systematic review and meta-analysis. Am J Public Health. 2018;108(2):e1-e7.
- Zangiabadi S, Costanian C, Tamim H. Dental care use in Ontario: the Canadian Community Health Survey (CCHS). BMC Oral Health. 2017;17(1):165.
- Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. J Womens Health (Larchmt). 2012;21(2):140-5.
- Kikwilu EN, Masalu JR, Kahabuka FK, Senkoro AR. Prevalence of oral pain and barriers to use of emergency oral care facilities among adult Tanzanians. BMC Oral Health. 2008;8:28.
- Das M, Angeli F, Krumeich AJSM, van Schayck OCP. The gendered experience with respect to health-seeking behaviour in an urban slum of Kolkata, India. Int J Equity Health. 2018;17(1):24.
- Fillingim RB, Browning AD, Powell T, Wright RA. Sex differences in perceptual and cardiovascular responses to pain: the influence of a perceived ability manipulation. J Pain. 2002;3(6):439-45.
- Sanden I, Larsson US, Eriksson C. An interview study of men discovering testicular cancer. Cancer Nurs. 2000;23(4):304-9.
- Richards HM, Reid ME, Watt GCM. Socioeconomic variations in responses to chest pain: qualitative study. BMJ. 2002;324(7349):1308-17.
- Hajek A, De Bock F, Huebl L, Kretzler B, König HH. Postponed dental visits during the COVID-19 pandemic and their correlates. Evidence from the nationally representative COVID-19 snapshot monitoring in Germany (COSMO). Healthcare (Basel). 2021;9(1):50.
- US Department of Health and Human Services Oral Health Coordinating Committee. US Department of Health and Human Services oral health strategic framework, 2014–2017. Public Health Rep. 2016;131(2):242-57.
- McKernan SC, Reynolds JC, Ingleshwar A, Pooley M, Kuthy RA, Damiano PC. Transportation barriers and use of dental services among Medicaid-insured adults. JDR Clin Trans Res. 2018;3(1):101-8.
- Eliott, S. Ontario's COVID-19 response: a history of announced measures, 2020–2022. Sausalito, Calif.: JD Supra; 2022. Available: https://www.jdsupra.com/legalnews/ontario-s-covid-19-response-a-history-1280608/ (accessed 2022 Aug. 23).
- Long L, Corsar K. The COVID-19 effect: number of patients presenting to the Mid Yorkshire Hospitals OMFS team with dental infections before and during the COVID-19 outbreak. Br J Oral Maxillofac Surg. 2020;58(6):713-4.
- Shah S, Wordley V, Thompson W. How did COVID-19 impact on dental antibiotic prescribing across England? Br Dent J. 2020;229(9):601-4.
- Altıntaş E. Complications of dental infections due to diagnostic delay during COVID-19 pandemic. BMJ Case Rep. 2022;15(4):e247553.
- Steinberg N, Allison P, Levin L. Infection prevention strategies concordance in Canadian dental schools during the COVID-19 pandemic. Int Dent J. 2022;72(5):682-90.
- Kielty P. The perceived effect of Covid-19 on undergraduate education in oral surgery: a qualitative study. DChDent dissertation. Dublin: Trinity College Dublin; 2022. Available: http://www.tara.tcd.ie/bitstream/handle/2262/101359/The%20Perceived%20Effect%20of%20Covid-19%20on%20Undergraduate%20Education%20in%20Oral%20Surgery%20-%20A%20Qualitative%20Study-1.pdf?sequence=3&isAllowed=y (accessed 2023 Oct. 23).
- Hattar S, AlHadidi A, Sawair FA, Alraheam IA, El-Ma’aita A, Wahab FK. Impact of COVID-19 pandemic on dental education: online experience and practice expectations among dental students at the University of Jordan. BMC Med Educ. 2021;21(1):151.
- Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS One. 2020;15(11):e0242905.
- Al Kawas S, Al-Rawi N, Talaat W, Hamdoon Z, Salman B, Al Bayatti S, et al. Post COVID-19 lockdown: measures and practices for dental institutes. BMC Oral Health. 2020;20(1):291.
- Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr. 2021;15(3):869-75.
- Dziedzic A, Tanasiewicz M, Tysiąc-Miśta M. Dental care provision during coronavirus disease 2019 (COVID-19) pandemic: the importance of continuous support for vulnerable patients. Medicina (Kaunas). 2020;56(6):294.
- Peloso RM, Pini NIP, Sundfeld Neto D, Mori AA, de Oliveira RCG, Valarelli FP, et al. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Braz Oral Res. 2020;34:e84.
- Lam R, Abbott P, Lloyd C, Lloyd C, Kruger E, Tennant M. Dental trauma in an Australian rural centre. Dent Traumatol. 2008;24(6):663-70.
- Živković D, Tošić G, Mihailović B, Miladinović M, Vujičić B. Diagnosis of periapical lesions of the front teeth using the internet. PONS Med J. 2010;7(4):138-43.
- Torres-Pereira C, Possebon RS, Simões A, Bortoluzzi MC, Leāo JC, Giovanini AF, et al. Email for distance diagnosis of oral diseases: a preliminary study of teledentistry. J Telemed Telecare. 2008;14(8):435-8.





