Abstract
Objectives:
The diagnosis, symptom onset, treatment, prognosis, radiographic features and effect of litigation on patients suffering temporomandibular disorders (TMDs) following motor vehicle accidents (MVAs) are still unknown yet highly debated. This review summarizes literature on this topic and provides evidence-based guidance to dental practitioners.
Methods
We applied PRISMA guidelines and their extension for scoping reviews (PRISMA-ScR). The search strategy was defined, and the electronic search included PubMed, MEDLINE, EMBASE, Cochrane Library, Web of Science, and Scopus. Extracted data were organized into categories, and we present a narrative summary of the main findings.
Results:
We included 37 articles in the review: 15 assessed the diagnosis of TMD following an MVA; 6 assessed onset of symptoms; 13 analyzed treatment options; 10 reviewed prognosis; 6 reviewed imaging findings; and 4 reviewed litigation factors.
Conclusions:
The review revealed heterogeneous results regarding the diagnosis, treatment, prognosis, imaging and litigation factors in MVA-related TMD patients. Future studies are recommended, and no definitive conclusions were drawn.
Introduction
Motor vehicle accidents (MVAs), defined as collisions involving motor vehicles with other vehicles, pedestrians, animals or stationary objects, are known to cause a variety of injuries, including whiplash-associated disorders (WADs). Whiplash is characterized by a sudden, forceful back-and-forth movement of the neck, which is frequently associated with the onset of symptoms of temporomandibular disorder (TMD).1,2 The prevalence of TMD after an MVA is reported to be significantly higher than that in the general population not involved in MVAs, with a notable incidence of TMD in those reporting a history of whiplash.3,4 In 2022, Canada saw an increase in the number of fatalities, serious injuries and total injuries from MVAs compared with the previous year. Despite this, there has been a long-term decline in the number of MVAs resulting in a single injury but no fatalities: from 150 493 in 2003 to 89 787 in 2022. The most frequent occurrences of serious injuries and fatalities were among people aged 25–34 years.1,5
The interrelation between TMDs and MVAs remains a subject of both medical and legal debate, compounded by the inherent variability in symptom presentation and the multifactorial nature of treatment approaches. This complexity is further amplified by significant legal implications, particularly concerning the future care costs and litigation in some Canadian provinces.
TMD encompasses a spectrum of over 30 clinical conditions affecting the temporomandibular joint (TMJ) and associated musculature. These conditions are generally classified into 3 primary categories: joint disorders, masticatory muscle disorders and TMD-related headaches.6 The pathophysiology of MVA-related TMD may involve both direct mechanical trauma to the TMJ and indirect effects, such as changes in the central nervous system, with psychological stress playing a contributory role.2,7
In addition to the indirect trauma associated with whiplash during MVAs, patients may also experience direct trauma from various internal and external sources, such as airbags, seatbelts and other components of the vehicle, as well as external objects, such as poles and roads.8 This scoping review seeks to consolidate and evaluate the existing literature on the nexus of TMD and MVAs concerning diagnosis, symptom onset, radiographic presentation, treatment modalities, prognostic outcomes and litigation, thereby informing the broader medical, dental and legal communities on optimal management strategies for this patient group.
Methods
Our study population included all patients aged ≥18 years, who had been involved in an MVA. All settings of MVA accidents and patient complaints were included, i.e., patients seen in all clinical contexts (medical and dental settings). There was no restriction on geographic location.
The databases PubMed, EMBASE, Web of Science, Cochrane and Scopus were queried. Types of studies included were experimental, observation and reviews. There was no limit on articles by date, but only articles published in English were used. The review was registered with PROSPERO (ID CRD42023400003).
Terms used in the search strategy were: (motor* OR vehicle* OR automobile* OR car OR cars OR truck* OR traffic) adj3 (accident* OR collision* OR crash*) AND temporomandibular OR temporo mandibular
On 28 May 2023, we identified 400 articles from Scopus, 285 from MEDLINE, 145 from PubMed, 505 from Embase, 322 from Web of Science and 7 from Cochrane. All articles were uploaded to Covidence (Melbourne, Australia) for organization and screening. After removing duplicates, 697 articles were screened for relevance using titles and abstracts independently by NB and KP. RF resolved any conflicts. A total of 141 full-text articles were then independently reviewed by authors NB and KP, and 37 articles were included (Figure 1).
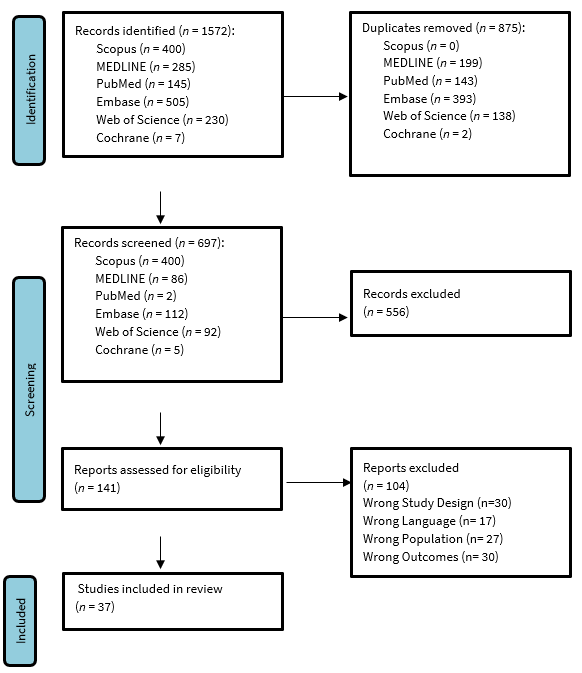
Figure 1: PRISMA flowchart of search strategy and results.
Results
The 37 articles analyzed in this review were categorized according to their primary focus among the search objectives, although several articles addressed more than 1 of the 6 areas of interest. Table 1 illustrates the distribution of articles across these outcomes: 15 articles were concerned with diagnosis,4,9–22 6 with symptom onset,23–28 13 with treatment options,15,16,18,24–26,29–35 10 with prognosis,13,24–26,29,36–40 6 with radiographic features40–45 and 5 with litigation factors.21,25,31,38,43 Some articles contributed to multiple outcomes. Relevant findings from each article were systematically highlighted and are detailed in Tables 2–7.
|
Topic |
Included articles |
|---|---|
| Diagnosis of TMD (n = 15) | Abd-Ul-Salam et al. 20029 Bal et al. 202010 Häggman-Henrikson et al. 201611 Eklund et al. 202012 Fernandez et al. 2009 13 Häggman-Henrikson et al. 20144 Klobas et al. 200414 Krogstad et al. 199815 Kronn 1993 16 Lampa et al. 2017 17 Landzberg et al. 2017 18 Marini et al. 2013 19 McKay & Christensen 199820 Ferrari et al. 1999 21 Visscher et al. 200522 |
| Onset of symptoms (n = 6) | Al-Ani 202323 Corsalini et al. 202224 Epstein & Klasser 201125 Epstein et al. 201026 Salé & Isberg 200727 Severinsson et al. 201028 |
| Treatment of TMD (n = 13) | Corsalini et al. 202224 Epstein 199229 Epstein & Klasser 201125 Epstein et al. 201026 Klobas et al. 200630 Kolbinson et al. 199731 Krogstad et al. 199815 Kronn 199316 Landzberg et al. 201718 Moses & Skoog 198632 McNamara et al. 199633 Naqvi & Fating 202034 Romanelli et al. 199235 |
| Prognosis of TMD (n = 10) | Böthun et al. 202336 Corsalini et al. 202224 Epstein 199229 Epstein & Klasser 201125 Epstein et al. 201026 Fernandez et al. 200913 Kasch et al. 200237 Kolbinson et al. 199838 Lampa et al. 202039 Salé et al. 201440 |
| Radiographic features of TMD (n = 6) | Ferrari & Leonard 199841 Garcia & Arrington 199642 Grushka et al. 200743 Lee et al. 201844 Lee et al. 202145 Salé et al. 201440 |
| Litigation factors (n = 5) | Epstein & Klasser 201125 Ferrari et al. 199921 Grushka et al. 200743 Kolbinson et al. 199731 Kolbinson et al. 199838 |
|
Authors, year, country |
Setting, study design |
Key findings |
|---|---|---|
|
Note: MVA = motor vehicle accident, TMD = temporomandibular disorder, TMJ = temporomandibular joint, WAD = whiplash associated disorder. |
||
| Abd-Ul-Salam et al. 2002, Canada9 |
Dental school/hospital Retrospective review Arthroscopic findings in patients with whiplash injury |
Disc displacement without reduction was common in WAD patients. Synovitis occurred in 73% of the patients, but severe synovitis was rare (7%). Mild to severe adhesions in 67% of joints. |
| Bal et al. 2020, Turkey10 |
Orofacial pain clinic at Yeditepe University Faculty of Dentistry Retrospective review Trauma and whiplash effect on clicking and crepitation |
Direct and/or whiplash trauma was not associated with TMDs or TMJ sounds, such as clicking/crepitation. |
| Häggman-Henrikson et al. 2016, Sweden11 |
Umeå University Hospital Cross-sectional study Comparing pain between patients with or without trauma |
Jaw pain, pain on movement and jaw locking were commonly seen in patients suffering from neck trauma. |
| Eklund et al. 2020, Sweden12 |
Umeå University Hospital Randomized controlled trial Comparing jaw and head/neck amplitude between whiplash and non-whiplash groups |
Compared with controls, WAD cases showed smaller jaw movement amplitude and higher neck pain intensity. High neck pain cases had significantly smaller jaw movement amplitudes. |
| Fernandez et al. 2009, USA13 |
Literature review Comparing traumatic and non-traumatic TMD patients |
Increased incidence of limited jaw mobility, masticatory muscle tenderness and internal derangement found in MVA cases. |
| Häggman-Henrikson et al. 2014, Sweden4 |
Systematic review Prevalence and sign/symptoms of TMD following MVA |
Compared with patients with TMD localized to the facial region, TMD patients with a history of whiplash trauma reported more TMD symptoms (limited jaw opening, increased TMD pain, headaches and stress). |
| Klobas et al. 2004, Sweden14 |
Public dental clinic Cross-sectional study Questionnaire and clinical exam evaluating TMJ in patients with chronic WAD and control |
TMD symptoms (limited opening, pain to palpation, TMJ clicking) were significantly higher in WAD group compared with the control group. |
| Krogstad et al. 1998, Norway15 |
Orofacial pain clinic Cross-sectional study Compare psychological and physical distress in whiplash patients receiving treatment |
WAD patients had higher scores than the non-traumatic TMD patients regarding obsession, somatization, depression and anger/hostility. |
| Kronn 1993, Ireland16 |
Accident and Emergency Department, St James' Hospital Cross-sectional study Cervical whiplash patients compared with control patients |
TMJ pain (p < 0.001) and limitation of mouth opening (p < 0.01). were significantly more frequent in the WAD group. Joint sounds and jaw deviation were not significantly different between groups. |
| Lampa et al. 2017, Sweden17 |
Emergency department at Umeå University Hospital Cross-sectional study Compare whiplash-related TMD to control patients |
WAD patients show signs of impaired chewing capacity as indicated by susceptibility to earlier onset of fatigue and pain while chewing during acute stages. |
| Landzberg et al. 2017, USA18 | Narrative review | Among TMD sufferers, jaw pain and dysfunction were more severe in those with a history of cervical whiplash. |
| Marini et al. 2013, Italy19 |
Department of Orthodontics and Gnathology, University of Bologna, Italy Case–control study Compare the frequency of specific TMD diagnoses in patients who had late whiplash syndrome and control group |
Prevalence of myofascial pain and disc displacement with reduction was significantly higher in patients after MVA who experienced orofacial pain than in patients with chronic orofacial pain who had no history of MVA. No significant differences between patients after MVA and control patients concerning the frequency of osteoarthritis or disc displacement without reduction. |
| McKay & Christensen 1998, USA20 | Narrative review | TMJ disc displacement and inflammation following MVA often represent pre-existing disease entity that MVA exacerbates. |
| Ferrari et al. 1999, Lithuania21 |
Traffic police department of Kaunas, Lithuania Retrospective study Rear-end collision patients compared with controls |
Both groups exhibited similar frequency of jaw pain. Both groups exhibited a low prevalence of joint sounds, jaw locking, tinnitus and facial pain. |
| Visscher et al. 2005, Netherlands22 |
Roessingh Rehabilitation Center Cross-sectional study Comparison of WAD pain group and control group with no neck pain |
WAD pain group more often suffered from TMD pain and widespread pain than the no-neck-pain group. WAD patients exhibited greater psychological distress. |
|
Authors, year, country |
Setting, study design |
Key findings |
|---|---|---|
|
Note: MVA = motor vehicle accident, TMD = temporomandibular disorder, TMJ = temporomandibular joint, WAD = whiplash associated disorder. |
||
| Al-Ani 2023, UK23 | Narrative review | Click development after an accident is common and correlated with functional limitation. TMD symptoms might not become apparent until pain from other structures subsides (3–4 weeks). Other symptoms can mask TMD symptoms. |
| Corsalini et al. 2022, Italy24 | Dental Prosthesis Department, University of Bari Prospective clinical study Patients examined at multiple time points after MVA | Patients often perceive no pain or injury immediately after MVA. Symptomatology gradually increases in the following days. |
| Epstein & Klasser 2011, USA25 | Narrative review | Evidence for delayed onset/recognition of TMD after whiplash is grade B. |
| Epstein et al. 2010, USA26 | Narrative review | Incidence of new symptoms of TMDs among MVA patients was 5 times that of control group and higher in females than males. Delated painful symptoms at 1-year follow up were seen in 19%. |
| Salé & Isberg 2007, Sweden27 | Hospital emergency department Controlled prospective study 60 patients assessed and examined before whiplash and multiple time points after | 33% of whiplash sufferers are at risk of developing delayed TMJ pain and dysfunction with onset during the year after the accident. |
| Severinsson et al. 2010, Sweden28 | Emergency hospital departments, primary health clinics and Volvo accident investigation team Controlled prospective study Assessment of jaw pain following MVA | Jaw symptoms are uncommon in the acute phase following MVA, but frequently develop over months after an accident. Women have symptoms more often than men. Symptoms after low-impact rear-end accidents are common. |
|
Authors, year, country |
Setting, study design |
Key findings |
|---|---|---|
|
Note: MVA = motor vehicle accident, NSAID = nonsteroidal anti-inflammatory drug, TENS = transcutaneous electrical nerve stimulation, TMD = temporomandibular disorder, TMJ = temporomandibular joint, WAD = whiplash associated disorder. |
||
| Corsalini et al. 2022, Italy24 |
Dental prosthesis department, University of Bar Prospective clinical study Use of Zimmer collar use and occlusal splint |
Patients who used occlusal splint therapy as a stand-alone treatment, and did not use pharmacologic intervention showed the worst outcomes. |
| Epstein 1992, Canada29 | Narrative review |
The effect of occlusal appliances in reducing pain associated with TMD is well documented. No evidence to support the suggestion that structural changes (e.g., occlusal treatment or surgery) are required in TMD management. |
| Epstein & Klasser 2011, USA25 | Narrative review | Multiple therapeutic approaches exist for TMD, including NSAIDs, psychotropic agents, steroids and anesthetics. Prednisone is mentioned as an option for acute management, while intramuscular injections are noted for chronic cases. Evidence for muscle relaxants and analgesics remains limited. |
| Epstein et al. 2010, USA26 | Narrative review |
Prednisone can be used for acute pain within 1 week of injury. For chronic symptoms, intramuscular lidocaine was superior to placebo. Myofascial trigger point injection was effective, but no difference was documented between saline and botulinum toxin. Limited evidence for pharmacotherapy. |
| Klobas et al. 2006, Sweden30 |
Rehabilitation centre Case–control study 55 patients diagnosed with chronic TMD and WAD; 25 underwent jaw exercises and 30 followed regular rehab |
Jaw exercises did not help chronic whiplash TMD patients' pain complaints but did improve range of motion. |
| Kolbinson et al. 1997, Canada31 |
Oral medicine private practice Cross-sectional study Comparing treatments and their success in TMD patients with and without MVA |
MVA patients tended to receive more types of treatment over a longer period and have poorer treatment outcomes compared with the non-trauma group. |
| Krogstad et al. 1998, Norway15 |
Cross-sectional study Compare somatic complaints and psychological distress in a group of whiplash patients and examine the effects of conservative treatments. |
Treatment focused on the entire body musculature with cognitive and behavioural approaches best. Conservative treatment does not appear to have a clear positive influence on patients' headache frequency and intensity. |
| Kronn 1993, Ireland16 |
Accident and emergency department, St James' Hospital Cross-sectional study 40 consecutive patients with a cervical whiplash injury were examined and compared with 40 matched controls |
WAD group is more likely to seek treatment for their symptoms compared with controls. |
| Landzberg et al. 2017, USA18 | Narrative review |
Traditional treatments tend to work more poorly in patients with a history of whiplash. A multidisciplinary approach, including psychological evaluation, is recommended. |
| McNamara et al. 1996, Australia33 |
Case–control study Comparison between MVA and control groups with TMD response to arthroscopic treatment |
Arthroscopic surgery reduced pain for both groups. |
| Naqvi & Fating 2020, India34 |
Case study 1 patient with 3-year history of TMD symptoms following MVA |
Physiotherapy (TENS, myofascial release and isometric exercises) can help improve range of motion and reduce pain. |
| Romanelli et al. 1992, Canada35 |
Craniofacial pain clinical research unit, Mount Sinai Hospital Retrospective study Comparison of various treatment modalities |
Mandibular bite plane (splint) saw 73% improvement in symptoms for non-MVA and 43% for MVA patients. Physiotherapy saw 74% improvement in symptoms for non-MVA and 64% for MVA patients. NSAID saw 76% improvement in symptoms for non-MVA and 76% for MVA patients. Moist heat and massage saw 77% improvement in symptoms for non-MVA and 59% for MVA patients. Overall more success in modalities when no MVA history. |
|
Authors, year, country |
Setting, study design |
Key findings |
|---|---|---|
|
Note: MVA = motor vehicle accident, TMD = temporomandibular disorder, TMJ = temporomandibular joint, WAD = whiplash associated disorder. |
||
| Böthun et al. 2023, Sweden36 |
Emergency department Case–control study Pain on palpation on neck muscles, jaw muscles and jaw movements post whiplash |
Individuals with whiplash trauma present a higher risk for short-term and long-term jaw pain but exhibit normal jaw movements. Women have a worse prognosis than men. |
| Corsalini et al. 2022, Italy24 |
Dental prosthesis department, University of Bar Prospective clinical study Craniomandibular dysfunction indices |
Acute WAD disorders are often self-limiting over a few months.
Symptom chronicity appears mostly related to lesion severity, possible pre-existence of craniomandibular dysfunction/disorder and patient age. |
| Epstein 1992, Canada29 | Narrative review |
Statistically significant prognostic factors for MVA-related TMD include rear and front collision, occipital headache, referred symptoms, intracapsular pain/headache, abnormal neurology, positive radiology, osteoarthrosis and insurance claims. Trauma-associated TMD vs non-trauma associated TMD responds less well to therapy. Clicking resolves in 25% of MVA patients. 70% of patients with non-painful clicking will develop pain. |
| Epstein & Klasser 2011, USA25 | Narrative review | Many factors affect prognosis including pre-existing history, physical and psychological factors. |
| Epstein et al. 2010, USA26 | Narrative review |
Approximately 15–40% of patients with acute WAD develop chronic symptoms. Both groups (WAD and non-WAD) responded equally well to conservative treatment. |
| Fernandez et al. 2009, USA13 | Narrative review | Thorough, comprehensive assessment required in MVA patients. Balance and postural abnormalities, shoulder-neck headache, stress habits and centrally mediated pain factors should be included as potential variables of prognosis. |
| Kasch et al. 2002, Denmark37 |
Case–control study Assess TMJ pain in post-MVA patients |
Global pain intensity was low after 4 weeks and 6 months post-injury (McGill Pain Questionnaire and exam by dentist), suggesting whiplash is not a major risk factor in the development of TMD issues. |
| Kolbinson et al. 1998, Canada38 |
Private oral medicine practice Retrospective review 50 patients with post-motor vehicle accident TMD |
Significant predictors of the number of treatment visits were the severity of vehicle damage, headrest use, position in the vehicle and insurance claim status. Impact direction and number of MVAs were significant predictors of neck muscle tenderness scores. The severity of vehicle damage and patient age were significant predictors of final jaw muscle tenderness scores. |
| Lampa et al. 2020, Sweden39 |
Emergency department Prospective cohort study Evaluate the course of orofacial pain and jaw disability in relation to neck pain, neck disability and psychosocial factors at the acute stage and the chronic stage after whiplash trauma |
A majority (68%) of cases with pain in the jaw region in the acute stage also reported jaw pain at the 2-year follow up. |
| Salé et al. 2014, Sweden40 |
Emergency department Controlled prospective study 15-year follow-up on whiplash-related TMD compared with control patients |
The prevalence of TMJ symptoms in patients was increased and significantly higher than in control participants from inception throughout the 15-year study period. |
|
Authors, year, country |
Setting, study design |
Key findings |
|---|---|---|
|
Note: ADDWoR = anterior disc displacement without reduction, ADDWR = anterior disc displacement with reduction, DDWoR = disc displacement without reduction, LPM = lateral pterygoid muscle, MVA = motor vehicle accident, TMD = temporomandibular disorder, TMJ = temporomandibular joint. |
||
| Ferrari & Leonard 1998, USA41 | Narrative review |
Clinicians often report that an association between TMD symptoms and abnormal imaging findings is equivalent to demonstrating a causal relation, which has not been proven. There is a high prevalence of TMJ imaging abnormalities in the asymptomatic population; from the third decade of life onward, most patients exhibit remodeling. |
| Garcia & Arrington 1996, USA42 | Case–control study |
Among 164 patients, internal derangement was present in 143 (87%) of TMJs; 118 (72%) demonstrated disc displacement with reduction; 25 (15%) demonstrated disc displacement without reduction; only 21 (13%) of TMJs were found to be normal. Because of the lack of a suitable control group, no conclusions were drawn. |
| Grushka et al. 2007, USA43 | Dental centre for TMD Retrospective study | A significantly lower incidence of clinically diagnosed disc and bony changes in the post-MVA (74%) compared with the control group (88%); a significantly lower frequency of disc displacement found on MRI in the post-MVA (48%) compared with the control group (69%). |
| Lee et al. 2018, Korea44 | Retrospective case–control study |
Patients with whiplash were more likely to have DDWoR (53.3% vs. 28.9%) and disc deformity (64.4% vs. 33.3%), which were significantly higher than those in the control group (all p < 0.05). Distributions of effusion, ADDWR and condylar degeneration in the TMD group were not significantly different from the control group. |
| Lee et al. 2021, Korea45 | Retrospective case–control study |
Atrophy of the LPM was most commonly seen in the trauma group, as was disc deformity. The clinical symptoms of TMD were not correlated with MRI findings in the trauma group. |
| Salé et al. 2014, Sweden40 |
Emergency department Controlled prospective study |
15-year follow up found that MRI findings of TMJ disorder were as prevalent in patients exposed to whiplash trauma as in control participants (TMJ symptoms or not). TMJ pain was not associated with TMJ disc displacement. |
|
Authors, year, country |
Setting, study design |
Key findings |
|---|---|---|
|
Note: MVA = motor vehicle accident, TMD = temporomandibular disorder, TMJ = temporomandibular joint. |
||
| Epstein & Klasser 2011, USA25 | Narrative review | Impact of litigation on the prognosis of TMD following MVA; 1 study showed significantly more symptomatic complaints among litigating patients. |
| Ferrari et al. 1999, Lithuania21 |
Traffic police department of Kaunas, Lithuania Retrospective study Rear-end collision patients compared with controls |
Cultural and psychosocial factors led to less reporting of chronic TMD symptoms after whiplash injuries in Lithuania compared with Western societies, where symptom expectation, amplification and insurance fraud are more prevalent. |
| Grushka et al. 2007, USA43 |
Dental centre for TMD Retrospective study Comparison between MVA litigating and non-litigious groups |
Clinical examination demonstrated no significant difference) in the range of opening between the litigating and nonlitigating patients. TMJ capsulitis was significantly more prevalent in the litigating group. MRI studies demonstrated no differences in disc displacement or osteoarthritis, but disc displacement without reduction was found significantly more frequently in the litigating group. |
| Kolbinson et al. 1998, Canada38 |
Oral medicine private practice Cross-sectional study Patients with past MVA were interviewed |
75% had persistent jaw pain, jaw dysfunction and headache; over 80% reported chronic neck pain. Insurance claim settlement status did not affect symptoms. |
| Kolbinson et al. 1997, Canada31 |
Oral medicine private practice Cross-sectional study Comparing treatment outcomes in patients involved in litigation compared with those not |
Patients who were in litigation were in treatment significantly longer, required more sessions and self-reported greater pain. They had less pain reduction and improvement than the non-litigating group. |
In the diagnosis of TMD patients after an MVA (Table 2),4,9–22 evidence suggests no unifying symptomatology. In multiple studies, people with recent whiplash trauma reported a higher prevalence of jaw pain, higher pain intensity and greater symptoms compared to patients without a history of whiplash trauma. 7,11,14 Common diagnoses included limited mouth opening and disc displacement.14 However, it was also suggested that in patients with TMD and whiplash injury, higher pain prevalence might be a result of psychological distress.
Regarding the onset of TMD symptoms following an MVA (Table 3), 1 paper reports immediate symptoms after a whiplash injury, including a “click” sound and limited mouth opening.23 Nonetheless, acute symptoms of whiplash trauma are uncommon and little to no pain is usually perceived immediately after the injury.24,28 Corsalini et al.24 suggest that symptomatology increases over the few days following injury, while Al-Ani23 suggests it may take up to 3 or 4 weeks for symptoms to develop; others suggest that period may be up to a year.27,28
Treatment options for TMDs following an MVA (Table 4) primarily involve conservative strategies, such as medications, physiotherapy and occlusal appliance therapy. Adopting a comprehensive full-body treatment approach is recommended, especially under the supervision of clinicians who specialize in these conditions, including pain physicians or dental specialists such as oral medicine specialists and oral surgeons. Although surgery is generally not the first course of action and has been minimally explored in post-MVA scenarios, minimally invasive procedures, like arthrocentesis and arthroscopy, may be considered for cases presenting with structural damage or jaw locking.
Multiple factors could impact the prognosis of TMD patients following an MVA (Table 5). Gender, age, initial severity, pre-existing conditions and type of collision were a few of the factors assessed. Also examined was which factors could impact certain types of injury, i.e., limited mouth opening vs. jaw tenderness. The development of acute TMD issues into chronic TMD issues was also examined.26,29
Radiographic features of TMD that are evident following an MVA include disc displacement, with and without reduction, and MRI was used in many studies (Table 6). The development of osteoarthritis does not appear to be related to an MVA.
We examined whether ongoing litigation impacted TMD signs and symptoms and whether there were any objective differences between non-litigating and litigating patients (Table 7). The relevance of these findings to Canadian clinicians may change depending on whether their province has “no-fault insurance.” In 1 study, significantly more symptomatic complaints were noted by litigating patients.25 However, the opposite was seen in a Lithuanian study.21 Grushka et al.43 reported no difference in range of opening; however, TMJ capsulitis was significantly more common in the litigating group vs. the non-ligating group.43 Disc displacement with reduction was greater in litigating patients. In 1 article, no apparent difference in symptoms was found between those who had settled claims and those who had not31; however, those in litigation were in treatment longer, requested more treatment and reported more pain.
Discussion
Existing research shows mixed findings related to TMD diagnosis following an MVA. In diagnosing TMD, patient questionnaires and self-reported pain levels need to be considered in the context of a widespread pain complaint. Masticatory muscle pain and headaches are common after whiplash.4 Crepitus is typically not associated with whiplash trauma, although disc displacement and adhesions are commonly seen.9 Other studies have rebutted this finding.10 An unknown, yet critically important factor, is whether TMJ disc displacement is a result of the trauma or simply a pre-existing condition.20 This is known to influence medical/legal proceedings. Osteoarthritis has not been found more often following MVAs.19 However, findings suggestive of disc displacement (clicking and deviation on opening) and limited mouth opening appear to be common features, with TMJ pain found commonly.16 A significant factor contributing to chronic pain is psychological distress, which may present secondary to an MVA.22 A thorough evaluation must include muscle palpation, range of motion measurement, jaw function assessment and psychological screening. General dentists encountering patients with TMD stemming from MVAs should consider referring them to specialists in this field for accurate diagnosis. A thorough TMJ evaluation is crucial to establish a dependable baseline of TMJ health. Without this foundational assessment, it becomes challenging to evaluate damage or the worsening of pre-existing conditions, retrospectively. In addition, without a clear baseline, monitoring the degree of improvement can be problematic. This is especially vital in litigation cases, where precise diagnostic benchmarks are essential.
When considering the onset of TMD after an MVA, it is essential to include a wide timeframe. Typically, acute symptoms are minimal and may be masked by the severity of other problems, or they may gradually increase with edema diffusion in soft tissues.23 Delayed onset may range from a few weeks after the injury to a year; delayed onset occurs in a third of people exposed to whiplash trauma. This wide range of symptoms demands careful examination and further study to narrow it down. A common cause of delayed onset is that more serious cervical symptoms can mask the TMD concerns and can take several weeks to resolve.23 TMD symptoms following MVAs tend to present within a few months. However, dental practitioners should monitor patients closely for up to a year after whiplash trauma occurs, as delayed onset and recognition are more common than acute onset.
Forms of treatment for TMD include occlusal appliances, occlusal adjustments, surgeries, medications (analgesics, muscle relaxants, anti-inflammatories, etc.), physiotherapy and psychological treatments. Establishing a good baseline and monitoring changes are paramount to successful treatment. MVA-related TMD patients tend to receive more types of treatments and medications and have poorer outcomes compared to patients without a history of MVA. Most articles tend to support the notion that initial treatment should be conservative (medications, physiotherapy, psychological counseling, occlusal appliance therapy) before moving on to surgery if needed. The success of muscle relaxants and analgesics is limited.26 In acute situations, prednisone can be considered. Intramuscular lidocaine (trigger point injections) is superior to no treatment for chronic symptoms. Botulin type-A toxin in small trials has been shown to provide some general relief of symptoms and increased range of motion in patients with whiplash.46 The success of jaw exercises in reducing symptoms is inconsistent across studies, with some showing positive benefits,30 but others not.34 Occlusal appliances have been shown to reduce TMD29 and also to be successful when used in conjunction with other treatments, such as physiotherapy and pharmacotherapy.24 The reviewed studies exhibited significant variation in the types of occlusal appliances used, their specific indications and the subsequent treatments administered. Consequently, it is not possible to offer specific recommendations.
There is no evidence of the success of treatments proposing structural changes (occlusal treatment or surgery) in post-MVA patients.29 Krogstad has suggested that the best course of treatment is a holistic, biopsychosocial approach.15 Referral to chronic multidisciplinary pain clinics that include a psychologist is ideal; however, wait times are often long and treatment is difficult to access. Minimally invasive surgical procedures, such as arthrocentesis have been shown to be effective for pain relief and reestablishing normal opening; however, this has not been studied thoroughly in the context of MVAs.47 Treatment approaches for TMD related to whiplash vary widely, and no standardized method has been established. A general dentist should ensure that a precise diagnosis is made before beginning conservative treatment. If the diagnosis remains unclear, a referral is recommended. If there is no improvement after a short period of conservative treatment or if legal considerations are critical, collaboration with appropriate specialists is recommended. Although early intervention is likely to be advantageous, there is currently no evidence explicitly supporting this assertion.
It has been suggested by multiple articles that women, in general, are at higher risk than men for more clinical symptoms.36,39 It has also been shown that age can be a significant factor in jaw tenderness, maximum opening and symptom chronicity, with older patients exhibiting poorer prognoses. 38 Other factors that have been shown to impact chronicity are severity and pre-existing jaw dysfunction/disorder.24 Rear and front collisions and insurance claims have all been shown to be significant prognostic factors.29 The severity of vehicle damage and age affect final jaw muscle tenderness, while only age and gender affect maximum opening.38 From this, we can see that multiple factors influence various TMD symptoms. Regarding the progression of TMD from an acute to a chronic state, non-painful clicking will develop in 70% of patients,29 and approximately 15–40% of patients with acute symptoms develop chronic symptoms.26 According to another article,39 68% of patients with jaw pain report it again at the 2-year follow up. It is common for pain to persist for years, and often symptoms can worsen over time. The reason for this needs to be further elucidated.
In examining MRI findings for patients with TMD following an MVA, most studies cannot correlate TMJ findings with the MVA. However, Lee et al.44 report that TMD patients with whiplash are more likely to have disc displacement without reduction and disc deformity. Grushka et al.43 found a high prevalence of disc displacement, both with and without reduction, in TMD patients post-MVA. However, compared to non-trauma TMD patients, post-MVA patients demonstrated a significantly lower frequency of disc displacement based on MRI findings, suggesting fewer anatomical changes in the temporomandibular joint.
Similarly, Salé and Isberg27 reported that their imaging findings in patients after whiplash trauma were the same as those with no previous trauma and that TMJ pain was not associated with disc displacement. Clinical symptoms of TMD could not be correlated with MRI findings, and there was no difference between patients with whiplash TMJ and non-whiplash TMJ with disc displacement without reduction and condylar degeneration.44 A complex issue is that osseous changes occur naturally with aging and might be mistakenly attributed to the MVA.41 The reviewed studies did not include panoramic radiographs. Furthermore, the correlation between MRI and CT findings and symptoms of TMD following MVAs remains ambiguous. Nonetheless, clinical evaluations should guide the decision-making process concerning the use of imaging techniques.
TMJ capsulitis and imaging that shows disc displacement without reduction are significantly more common among litigating patients compared with non-litigating groups; other signs, symptoms and radiographic features show no significant differences. However, there is a noticeable tendency for litigating patients to remain in treatment longer and report higher levels of pain. This may be attributed to the pursuit of financial compensation during litigation or more severe symptoms prompting the need for legal representation. In Lithuania,21 no increased severity of symptoms was reported for litigating patients, and compensation tended to be statistically lower. Why litigating patients may require more prolonged treatment remains unclear, and additional research is warranted. According to Alberta regulations,48 TMJ injuries involving bone or teeth damage or disc displacement are not classified under minor injury regulation, which has implications for litigation and the costs of future care. In litigation cases, a dental specialist is recommended to oversee the management of care to ensure accurate diagnosis and effective monitoring, including evaluating potential malingering.
This scoping review has several strengths, including a comprehensive search strategy encompassing multiple databases and a rigorous screening process to ensure the proper selection of relevant articles. The adherence to PRISMA-ScR guidelines further substantiates the methodological rigour of this review. This has allowed for a thorough examination of the multifaceted relation between TMD and MVAs. However, this scoping review also has limitations. The primary constraint is the heterogeneity of the studies included, which vary in terms of methods, sample sizes and outcomes measured. This diversity makes it challenging to draw definitive conclusions and limits the generalizability of the findings. In addition, longitudinal limits of studies in the included articles restrict our understanding of the long-term outcomes of TMD post-MVA.
Given these limitations, several areas of future research are recommended to enhance our understanding of TMDs post-MVAs. First, well-designed, longitudinal studies are needed to explore the progression of TMD from acute symptoms to chronic conditions. Such studies would help clarify the timelines of symptom development and resolution and identify early predictors of chronicity. This information could greatly improve both prognosis and intervention strategies.
Second, there is a need for standardized diagnostic criteria and outcome measures in studies related to TMD post-MVA. The current heterogeneity complicates comparisons across studies and limits the ability to draw conclusions. Consistent use of diagnostic criteria is suggested. Standardizing these elements would allow for more effective meta-analyses and systematic reviews, providing clearer insights into effective treatments.
Another area for future research is the role of psychological factors in the development and management of TMD following MVAs. Given the impact of psychological stress and trauma in chronic TMD cases, more detailed studies exploring the interplay between psychological conditions and physical symptoms are necessary. In addition, comparative studies that evaluate the efficacy of conservative versus surgical interventions, the role of pharmacological treatments and the benefits of multidisciplinary care approaches are needed. These studies should aim to identify the most effective and patient-centred treatment protocols.
Finally, the role of litigation in shaping the symptoms and outcomes of TMD following MVAs warrants extensive exploration. Future research should endeavour to ascertain whether ongoing litigation directly influences patient symptoms and treatment results or if it simply coincides with more severe instances. Clarifying this relationship is important for shaping the legal and insurance frameworks that impact TMD patients post-accident. These research initiatives would not only fill existing knowledge gaps but also significantly enhance the clinical management and legal aspects of TMD cases related to MVAs, ultimately improving patient outcomes.
Conclusion
This scoping review has explored the multifaceted relation between TMD and MVAs, shedding light on diagnostic challenges, symptom onset variability, treatment efficacy and the impacts of litigation. The evidence underscores the heterogeneous nature of TMD post-MVA, reflecting a complex interplay of physical injuries and psychological factors.
The findings reveal that TMD symptoms can vary widely in their onset and severity and are influenced by factors, such as the nature of the accident and individual patient characteristics. Although conservative treatment approaches, including medication, physiotherapy and occlusal appliance therapy, remain primary, the review highlights the need for a comprehensive treatment strategy incorporating a multidisciplinary team. This approach not only addresses the physical aspects of TMD but also the psychological impacts, which are often significant.
Litigation appears to influence patient experiences and treatment outcomes, with litigating patients often reporting prolonged symptoms and requiring extended treatment periods. This aspect underscores the need for thorough documentation and a nuanced understanding of the legal context in managing TMD post-MVA.
This review has identified several gaps in the current research, particularly the need for longitudinal studies to better understand the progression of TMD from acute to chronic conditions post-accident. In addition, more rigorous investigations into the effectiveness of various treatment modalities in this specific patient population are warranted. Although our understanding of TMD post-MVA has advanced, significant challenges remain and further studies are required.
THE AUTHORS
Acknowledgments and Funding
Corresponding author: Reid Friesen: Mike Petryk School of Dentistry, Faculty of Medicine & Dentistry, University of Alberta, Edmonton, Alberta. Email: rtfriese@ualberta.ca
NB received funding support from the Oral Medicine and Pathology Undergraduate Studentship.
This article has been peer reviewed.
The authors declare that they have no competing interests.
References
- Toney-Butler TJ, Varacallo M. Motor vehicle collisions. Treasure Island, Fla: StatPearls Publishing; 2024. Available: https://pubmed.ncbi.nlm.nih.gov/28722984/ (accessed 2024 Nov. 20).
- Weinberg S, Lapointe H. Cervical extension-flexion injury (whiplash) and internal derangement of the temporomandibular joint. J Oral Maxillofac Surg. 1987;45(8):653-6.
- Häggman-Henrikson B, List T, Westergren HT, Axelsson SH. Temporomandibular disorder pain after whiplash trauma: a systematic review. J Orofac Pain. 2013;27(3):217-26.
- Häggman-Henrikson B, Rezvani M, List T. Prevalence of whiplash trauma in TMD patients: a systematic review. J Oral Rehabil. 2014;41(1):59-68.
- Canadian motor vehicle traffic collision statistics. Ottawa: Transport Canada; 2022. Available: https://tc.canada.ca/en/road-transportation/statistics-data/canadian-motor-vehicle-traffic-collision-statistics-2022 (accessed 2024 June 5).
- Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28(1):6-27.
- Cairns BE. Pathophysiology of TMD pain — basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil. 2010;37(6):391-410.
- Giovannini E, Santelli S, Pelletti G, Bonasoni MP, Cornacchia A, Pelotti S, et al. Pediatric motor vehicle crashes injuries: a systematic review for forensic evaluation. Int J Legal Med. 2024;138(4):1329-41.
- Abd-Ul-Salam H, Kryshtalskyj B, Weinberg S. Temporomandibular joint arthroscopic findings in patients with cervical flexion-extension injury (whiplash): a preliminary study of 30 patients. J Can Dent Assoc. 2002;68(11):693-6.
- Bal B, Koksal T, Ebeoglu B, Oral K. Retrospective analysis of trauma incidence in patients with temporomandibular disorders. Dent Traumatol. 2020;36(6):618-23.
- Häggman-Henrikson B, Lampa E, Marklund S, Wänman A. Pain and disability in the jaw and neck region following whiplash trauma. J Dent Res. 2016;95(10):1150-60.
- Eklund A, Wiesinger B, Lampa E, Österlund C, Wänman A, Häggman-Henrikson B. Jaw-neck motor function in the acute stage after whiplash trauma. J Oral Rehabil. 2020;47(7):834-42.
- Fernandez CE, Amiri A, Jaime J, Delaney P. The relationship of whiplash injury and temporomandibular disorders: a narrative literature review. J Chiropr Med. 2009;8(4):171-86.
- Klobas L, Tegelberg A, Axelsson S. Symptoms and signs of temporomandibular disorders in individuals with chronic whiplash-associated disorders. Swed Dent J. 2004;28(1):29-36.
- Krogstad BS, Jokstad A, Dahl BL, Soboleva U. Somatic complaints, psychologic distress, and treatment outcome in two groups of TMD patients, one previously subjected to whiplash injury. J Orofac Pain. 1998;12(2):136-44.
- Kronn E. The incidence of TMJ dysfunction in patients who have suffered a cervical whiplash injury following a traffic accident. J Orofac Pain. 1993;7(2):209-13.
- Lampa E, Wänman A, Nordh E, Häggman-Henrikson B. Effects on jaw function shortly after whiplash trauma. J Oral Rehabil. 2017;44(12):941-7.
- Landzberg G, El-Rabbany M, Klasser GD, Epstein JB. Temporomandibular disorders and whiplash injury: a narrative review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124(2):e37-46.
- Marini I, Paduano S, Bartolucci ML, Bortolotti F, Bonetti GA. The prevalence of temporomandibular disorders in patients with late whiplash syndrome who experience orofacial pain: a case–control series study. J Am Dent Assoc. 2013;144(5):486-90.
- McKay DC, Christensen LV. Whiplash injuries of the temporomandibular joint in motor vehicle accidents: speculations and facts. J Oral Rehabil. 1998;25(10):731-46.
- Ferrari R, Schrader H, Obelieniene D. Prevalence of temporomandibular disorders associated with whiplash injury in Lithuania. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87(6):653-7.
- Visscher C, Hofman N, Mes C, Lousberg R, Naeije M. Is temporomandibular pain in chronic whiplash-associated disorders part of a more widespread pain syndrome? Clin J Pain. 2005;21(4):353-7.
- Al-Ani Z. Whiplash-associated temporomandibular disorders: a review article. Prim Dent J. 2023;12(1):79-84.
- Corsalini M, Capodiferro S, dell'Olio F, Albanese G, Quaranta N, Solarino B, et al. Cranio-mandibular disorders after whiplash injury: a mono-institutional clinical study on 31 patients. Int J Environ Res Public Health. 2022;19(2):901.
- Epstein JB, Klasser GD. Whiplash-associated disorders and temporomandibular symptoms following motor-vehicle collisions. Quintessence Int. 2011;42(1):e1-14.
- Epstein JB, Klasser GD, Kolbinson DA, Mehta SA. Orofacial injuries due to trauma following motor vehicle collisions: Part 2. Temporomandibular disorders. J Can Dent Assoc. 2010;76:a172.
- Salé H, Isberg A. Delayed temporomandibular joint pain and dysfunction induced by whiplash trauma: a controlled prospective study. J Am Dent Assoc. 2007;138(8):1084-91.
- Severinsson Y, Bunketorp O, Wenneberg B. Jaw symptoms and signs and the connection to cranial cervical symptoms and post-traumatic stress during the first year after a whiplash trauma. Disabil Rehabil. 2010;32(24):1987-98.
- Epstein JB. Temporomandibular disorders, facial pain and headache following motor vehicle accidents. J Can Dent Assoc. 1992;58(6):488-9.
- Klobas L, Axelsson S, Tegelberg A. Effect of therapeutic jaw exercise on temporomandibular disorders in individuals with chronic whiplash-associated disorders. Acta Odontol Scand. 2006;64(6):341-7.
- Kolbinson DA, Epstein JB, Senthilselvan A, Burgess JA. A comparison of TMD patients with or without prior motor vehicle accident involvement: treatment and outcomes. J Orofac Pain. 1997;11(4):337-45.
- Moses AJ, Skoog GS. Cervical whiplash and TMJ. Basal Facts. 1986;8(2):61-3.
- McNamara DC, Rosenberg I, Jackson PA, Hogben J. Efficacy of arthroscopic surgery and midlaser treatments for chronic temporomandibular joint articulator disc derangement following motor vehicle accident. Aust Dent J. 1996;41(6):377-87.
- Naqvi WM, Fating TB. Temporomandibular joint dysfunction: a non-invasive approach towards the management of a long-standing condition. Int J Pharm Res. 2020;12:1131-4.
- Romanelli GG, Mock D, Tenenbaum HC. Characteristics and response to treatment of posttraumatic temporomandibular disorder: a retrospective study. Clin J Pain. 1992;8(1):6-17.
- Böthun A, Häggman-Henrikson B, Stålnacke BM, Wänman A, Nordh E, Lampa E, et al. Clinical signs in the jaw and neck region following whiplash trauma — a 2-year follow-up. Eur J Pain. 2023;27(6):699-709.
- Kasch H, Hjorth T, Svensson P, Nyhuus L, Jensen TS. Temporomandibular disorders after whiplash injury: a controlled, prospective study. J Orofac Pain. 2002;16(2):118-28.
- Kolbinson DA, Epstein JB, Senthilselvan A, Burgess JA. Effect of impact and injury characteristics on post-motor vehicle accident temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(6):665-73.
- Lampa E, Wänman A, Nordh E, Stålnacke BM, Häggman-Henrikson B. The course of orofacial pain and jaw disability after whiplash trauma: a 2-year prospective study. Spine (Phila Pa 1976). 2020;45(3):e140-7.
- Salé H, Bryndahl F, Isberg A. A 15-year follow-up of temporomandibular joint symptoms and magnetic resonance imaging findings in whiplash patients: a prospective, controlled study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(4):522-32.
- Ferrari R, Leonard MS. Whiplash and temporomandibular disorders: a critical review. J Am Dent Assoc. 1998;129(12):1739-45.
- Garcia Jr R, Arrington JA. The relationship between cervical whiplash and temporomandibular joint injuries: an MRI study. Cranio. 1996;14(3):233-9.
- Grushka M, Ching VW, Epstein JB, Gorsky M. Radiographic and clinical features of temporomandibular dysfunction in patients following indirect trauma: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(6):772-80.
- Lee YH, Lee KM, Auh QS, Hong JP. Magnetic resonance imaging-based prediction of the relationship between whiplash injury and temporomandibular disorders. Front Neurol. 2018;8:725.
- Lee YH, Lee KM, Auh QS. MRI-based assessment of masticatory muscle changes in TMD patients after whiplash injury. J Clin Med. 2021;10(7):1404.
- Juan FJ. Use of botulinum toxin-A for musculoskeletal pain in patients with whiplash associated disorders. BMC Musculoskelet Disord. 2004;5:5.
- Nitzan DW, Dolwick MF, Martinez GA. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49(11):1163-7.
- Minor injury regulation (Alberta Regulation 123/2004). Edmonton: Government of Alberta; 2020. Available: https://open.alberta.ca/publications/2004_123 (accessed 2024 June 04)



