Abstract
Introduction:
Views on silver diamine fluoride (SDF) have been studied in various settings worldwide but remain underexplored in the Canadian context. In this study, we explored awareness, acceptability, general and economic perception and potential patient acceptance of SDF for caries management in children and older adults. We also looked at the impact of an educational workshop on SDF for dental professionals in Northern Ontario.
Methods
A 42-item structured questionnaire was administered to attendees at a workshop on minimally invasive dentistry held in Thunder Bay, Ontario. It elicited information regarding respondents’ demographics, their perception, acceptance and use of SDF and the workshop’s influence on uptake of the material.
Results:
Participants in this cross-sectional study were 53 dental professionals, mainly dental hygienists (45.3%) and dentists (35.8%). Their views on the use of SDF as a minimally invasive technique and on how it was accepted by their patients and patients’ caregivers were generally positive. Respondents reported that the workshop made them more likely to choose SDF for treating children (82.4%) and older adults (87.8%). We noted differences between dentists and non-dentists, specifically regarding potential parental acceptance of SDF staining in anterior temporary teeth (p = 0.030), as well as SDF’s benefits in older adults in long-term care (p = 0.007), with a higher proportion of non-dentists viewing SDF more favourably.
Conclusions:
SDF awareness and acceptance were high among dental professionals in Northern Ontario who attended a workshop presenting the beneficial effects of SDF for children and older adults.
Introduction
Over 7 years have passed since Health Canada approved 38% silver diamine fluoride (SDF) as a dental caries arresting agent.1 This came on the heels of the United States’ Food and Drug Administration’s endorsement in 2014.2 Provider, patient and research interest in SDF has been on the rise ever since.3,4 Since its approval by Health Canada in 2017, particular attention has been paid to studying the advantages of using SDF’s caries arrest effects in children and older adults (≥65 years) as its 38% presentation (that is containing 44 800 ppm of fluoride) is considered a “patient” and “operator” friendly minimally invasive, non-aerosol generating procedure.4,5 In pediatric dentistry, interest in SDF lies in the avoidance of pharmacologic behaviour guidance techniques,6 its application in public health settings7 and its potential cost-effectiveness.8,9 In older adults, it has been suggested as advantageous in root caries10 and dentin hypersensitivity11 management.
Despite evidence of SDF’s uses and advantages, its main drawback is the staining that develops on any demineralized surface it touches. Worldwide, this has been reported to be a point of resistance towards SDF’s use among parents,12 dental professionals13 and some authorities and decision-makers.14,15
In the Canadian context, literature on SDF is scarce. Parents whose children were treated with SDF for severe early childhood caries (ECC) in Manitoba were satisfied with the treatment but desired more guidance and education about the material.16 First Nations and Métis parents (also in Manitoba) similarly reported being open to the treatment, if adequate information was provided beforehand.17 On the education front, a 2018 survey of Canadian dental and dental hygiene programs revealed that SDF use is taught didactically in most programs (93%), but in a lower proportion clinically.18 We found no studies in the literature on the perception of SDF among Canadian dental professionals.
In Canada, SDF could play a beneficial role in caries management. Over a third (38.9%) of Canadian children 1-9 years of age have untreated caries lesions in their temporary teeth.19 This figure is exacerbated in Indigenous children: both the 2009–2010 First Nations Oral Health Survey20 and the 2018 First Nations Regional Health Survey21 revealed disparate outcomes in the oral health of Indigenous children compared with their non-Indigenous counterparts. In older adults, rates of root decayed or filled teeth have been reported to be 43.3% among dentate Canadians aged 60–79 years. 22 These data suggest that, in Canada, children, seniors in long-term care (LTC), Indigenous people, new immigrants, special needs individuals and people with low income are the populations most at risk for developing dental caries.23
Furthermore, health services delivery becomes more challenging in small towns and regions not adjacent to metropolitan areas24,25; this speaks to the structural barriers that exist in delivering and accessing care across the country. Canadian cities and towns that are regional hubs play important roles in commerce, cross-country connectivity and health services. For example, Thunder Bay is a key hub in northwestern Ontario, with its diverse population and close ties to Indigenous peoples in the area and surrounding Treaty lands.26 Thunder Bay is home to multiple health care facilities that provide necessary care and educational centres that train valuable professionals for the region. Although inhabitants of northwestern Ontario have typically traveled to such hubs to receive care, important shifts, like those led by Indigenous Health Transfer initiatives, are permitting self-governance and facilitating access to care to people who have historically been underserved.27
More can be done to strengthen the oral health care capacity in this important region. If the benefits of SDF are to be reaped and its adequate adoption pursued in Thunder Bay and similar regions, dental professionals’ perceptions of the material and potential barriers to its use must be understood. Therefore, this study aimed to analyze the awareness, acceptability among professionals, their general and economic perceptions and potential patient acceptance of SDF for caries management in children and older adults, as well as the impact of an educational workshop among dental professionals in Northern Ontario.
Methods
Study Design: Setting and Participants
We carried out this descriptive cross-sectional study in Thunder Bay, Ontario, on 17 November 2023. Participants were dental professionals who voluntarily completed a questionnaire after attending an in-person continuing education workshop titled: Be SMART: Improve Your Practice with Silver Diamine Fluoride and Glass Ionomer Cement. Dental professionals were viewed as any person who serves populations in the area of oral health care in any capacity (general practitioners, dental specialists, dental hygienists, dental educators, etc.).
An invitation to the workshop was extended to dental professionals in Thunder Bay and surrounding areas, including First Nations communities. It was led by an experienced American-board-certified pediatric dentist with expertise in minimally invasive dentistry. Workshop topics included the use of SDF for children and older adults, the use of glass ionomer cement restorations and the use of combined techniques, also known as SMART: silver modified atraumatic restorative technique.
After the workshop, participants were asked to complete a questionnaire, assisted but not guided by the research team. Written consent was obtained before attendees answered the questionnaire, and their participation (or lack thereof) did not affect their participation or credit for the workshop in any way. Participant anonymity was maintained throughout the study, no names were attached to the study instrument. Data analysis took this a step further by assigning participant identification numbers. Participants did not receive compensation for completing the questionnaire, and attendance at the workshop was free of charge. The workshop was advertised by Confederation College Thunder Bay, the Thunder Bay Dental Association and the Thunder Bay Dental Hygienists’ Society.
Questionnaire Design
The survey instrument was based on the aims of the study, previous literature on the topic (perceptions of SDF) and the investigators’ expertise (HPL: dental public health, KST: economic evaluations and FAP: pediatric dentistry). After a thorough literature review, expert consideration and taking into account research experience in the region, the authors concluded that existing surveys did not capture important topics related to the population and setting sampled, nor did they address some of the objectives in this study (e.g., decision-making in remote communities, cost perception and use of SDF in LTC).
Thus, a new instrument was constructed. The questionnaire included 42 items divided into 3 sections. The first part collected information regarding characteristics of the dental professionals and their patients. The second gauged participants’ general perceptions of SDF use, the perceived acceptability of SDF for their patients, perceptions of SDF’s effectiveness, costs and accessibility of SDF use in pediatric and older adult populations and the workshop’s influence on their SDF perceptions. Finally, 3 open-ended questions asked participants to report whether they perceived any additional problems (besides staining) in the acceptance of SDF for children and adults.
The instrument was developed in English and piloted with a similar cohort (dental professionals) before being administered to study participants. No content changes were made after piloting, only grammatical stylistic ones. The instrument can be made available on request to the corresponding author.
Data Analysis
Information collected in paper form was entered into the REDCap software (Vanderbilt University, 2004) to codify the data. Descriptive analysis was carried out to summarize the overall responses of participants. An exploratory subgroup analysis (Χ2 test) was then conducted to determine whether differences existed between dentists and non-dentist groups. In addition, an analysis of the effect of having received prior education on SDF regarding its uptake was also conducted (Χ2 test ). All data were analyzed using the SPSS statistical software package with significance set at p ≤ 0.05.
Ethics Approval
Prior ethics approval was received from the University of Toronto Research Ethics Board (RIS protocol no. 45469).
Results
Of 64 workshop attendees, 53 dental professionals aged 19–79 years (mean 45.9 years) completed the study questionnaire (Table 1). Most were dental hygienists (45.3%), followed by dentists (35.8%). The remainder of the participants included dental hygiene students, dental assistants and people who self-identified as “other,” which included health educator in combination with dental assistant or dental hygienist. Dental professionals who had been practising for ≥31 years were in the majority in this study (32.7%).
|
Characteristic |
No. (n = 53) |
% |
|---|---|---|
|
Note: CI = confidence interval. |
||
| Sex | ||
| Female | 38 | 71.7 |
| Male | 15 | 28.3 |
| Age, years | ||
| Mean (95% CI) | 45.9 (41.8–50.0) | |
| Median | 47 | |
| Standard deviation | 14.2 | |
| Range | 60 (19–79) | |
| Occupation | ||
| Student | 4 | 7.5 |
| Dental assistant | 2 | 3.8 |
| Dental hygienist | 24 | 45.3 |
| Dentist | 19 | 35.8 |
| Other | 4 | 7.5 |
| Specialization | ||
| Yes | 4 | 7.5 |
| No | 49 | 92.5 |
| Years in practice | ||
| 1–5 | 7 | 13.5 |
| 6–10 | 7 | 13.5 |
| 11–15 | 5 | 9.6 |
| 16–20 | 6 | 11.5 |
| 21–30 | 10 | 19.2 |
| ≥31 | 17 | 32.7 |
Participants reported serving different communities in and around Thunder Bay. Figure 1 depicts the regional distribution of the cities or First Nations reserves that the participants serve. Almost all dental professionals (98.1%) reported serving Indigenous patients, with 13.7% claiming an Indigenous patient population of 75% or more (Table 2). For 76.9% of the participants, 25–50% of their patient population was pediatric, and for 73.1%, 25–50% were older adults.
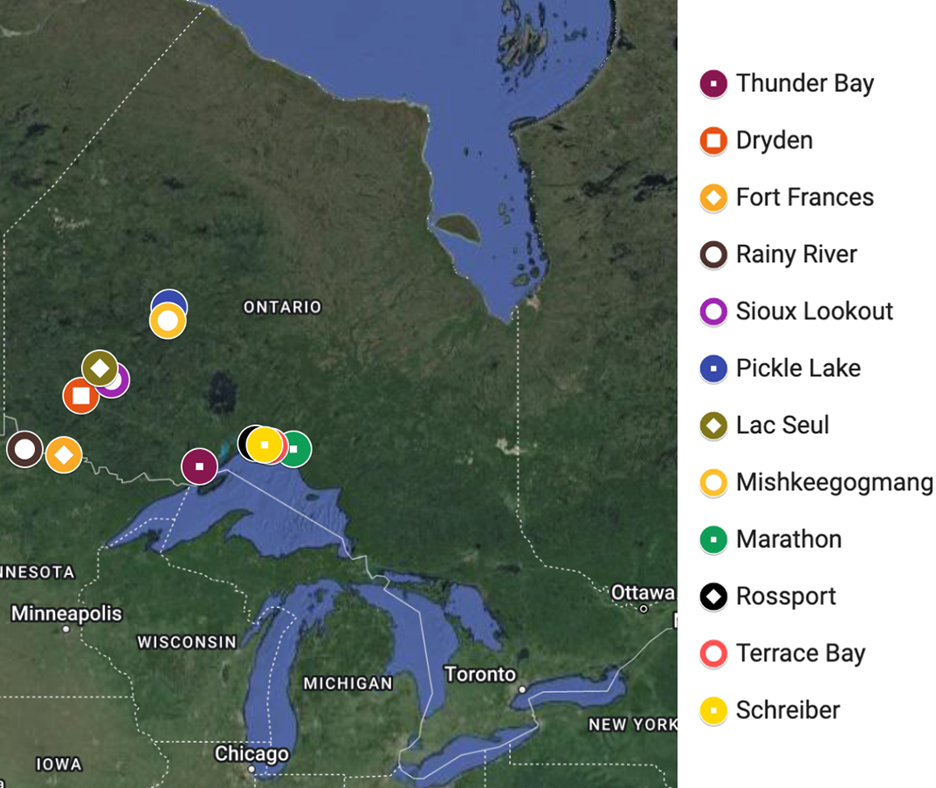
Figure 1: Cities served by workshop participants.
|
Characteristic |
% (n = 53) |
|---|---|
| Indigenous persons | |
| Yes | 98.1 |
| No | 1.9 |
| Proportion of Indigenous patients served | |
| 25% | 70.6 |
| 50% | 15.7 |
| 75% | 5.9 |
| 100% | 7.8 |
| Proportion of pediatric patients served (≤12 years old) | |
| 0% | 11.5 |
| 25% | 61.5 |
| 50% | 15.4 |
| 75% | 3.8 |
| 100% | 7.7 |
| Proportion of older adult patients served (≥65 years old) | |
| 0% | 9.6 |
| 25% | 40.4 |
| 50% | 32.7 |
| 75% | 15.4 |
| 100% | 1.9 |
All participants were aware of the use of SDF for pediatric patients before the workshop, but only 45.1% had received education on this topic as part of their professional training (Table 3). Most (88.7%) had heard of the use of SDF for older adults, and less than half (42.6%) received education on this use as part of their professional training.
Less than half of the study participants (43.4%) reported having previously used SDF in their clinical practice; 60.8% had never used it for pediatric patients and 57.7% had never used it with older adults (Table 3). Of those who reported having used SDF in older adults, nearly a third (32.1%) had used it for root caries, 30.2% for coronal caries and only 9.4% for dentin hypersensitivity.
|
Awareness of SDF |
% (n = 53) |
|---|---|
| Awareness of SDF use for pediatric patients before the workshop | |
| Aware | 100 |
| Not aware | 0 |
| Education on SDF use for pediatric patients as part of professional training | |
| Received | 45.1 |
| Not received | 54.9 |
| Awareness of SDF use for older adult patients before the workshop | |
| Aware | 88.7 |
| Not aware | 11.3 |
| Education on SDF use for older adult patients as part of professional training | |
| Received | 42.6 |
| Not received | 57.4 |
| Use of SDF | |
| Use of SDF in clinical practice | |
| Previously used | 43.4 |
| Never used | 56.6 |
| Frequency of SDF use in clinical practice | |
| Never | 55.8 |
| Rarely | 9.6 |
| Sometimes | 19.2 |
| Often | 11.5 |
| Very often | 3.8 |
| Frequency of SDF use for pediatric patients in clinical practice | |
| Never | 60.8 |
| Rarely | 9.8 |
| Sometimes | 19.6 |
| Often | 7.8 |
| Very often | 2.0 |
| Frequency of SDF use for older adult patients in clinical practice | |
| Never | 57.7 |
| Rarely | 11.5 |
| Sometimes | 19.2 |
| Often | 5.8 |
| Very often | 5.8 |
| Type of SDF use for older adult patients in clinical practice | |
| Root caries | |
| Checked | 32.1 |
| Unchecked | 67.9 |
| Coronal caries | |
| Checked | 30.2 |
| Unchecked | 69.8 |
| Dentin hypersensitivity | |
| Checked | 9.4 |
| Unchecked | 90.6 |
Most dental professionals had a positive view toward using SDF in children: they strongly agreed/agreed that they would use SDF to treat ECC in their community (84.9%) and that they would offer SDF treatments in cases where it could delay/prevent a child from having to be treated under general anesthesia (88.7%, Table 4).
|
Statement |
Response, % (n = 53) |
|---|---|
| Use | |
| I would use SDF to treat early childhood caries in my community | |
| Strongly disagree/disagree | 7.5 |
| Unsure | 7.5 |
| Strongly agree/agree | 84.9 |
| I would offer SDF treatments in cases where it could delay/prevent a child from having to be treated with general anesthesia | |
| Strongly disagree/disagree | 5.7 |
| Unsure | 5.7 |
| Strongly agree/agree | 88.7 |
| I have the option of using SDF for treatment in my practice | |
| Strongly disagree/disagree | 29.4 |
| Unsure | 15.7 |
| Strongly agree/agree | 54.9 |
| Acceptability | |
| Parents of my patient population would accept using SDF to treat early childhood caries. | |
| Strongly disagree/disagree | 1.9 |
| Unsure | 26.4 |
| Strongly agree/agree | 71.7 |
| Parents of my patient population would not accept SDF staining on posterior temporary teeth. | |
| Strongly disagree/disagree | 45.3 |
| Unsure | 30.2 |
| Strongly agree/agree | 24.5 |
| Parents of my patient population would not accept SDF staining on anterior temporary teeth. | |
| Strongly disagree/disagree | 15.1 |
| Unsure | 39.6 |
| Strongly agree/agree | 45.3 |
| Parents of my patient population would be more likely to accept SDF (in any sector) if their child had a previous early childhood caries treatment under general anesthesia. | |
| Strongly disagree/disagree | 7.5 |
| Unsure | 35.8 |
| Strongly agree/agree | 56.6 |
| Children of the population I serve would accept the SDF staining (in any sector). | |
| Strongly disagree/disagree | 15.1 |
| Unsure | 56.6 |
| Strongly agree/agree | 28.3 |
| EFFECTIVENESS AND ACCESSIBILITY | |
| SDF is more beneficial in remote communities. | |
| Strongly disagree/disagree | 34.0 |
| Unsure | 9.4 |
| Strongly agree/agree | 56.6 |
| SDF could potentially lower the number of pediatric patients requiring general anesthesia or sedation. | |
| Strongly disagree/disagree | 3.8 |
| Unsure | 13.2 |
| Strongly agree/agree | 83.0 |
| SDF is significantly difficult to obtain due to its availability. | |
| Strongly disagree/disagree | 41.5 |
| Unsure | 50.9 |
| Strongly agree/agree | 7.5 |
Most participants (71.7%) reported that parents of their pediatric patient population would accept using SDF to treat ECC (Table 4). Participants were more likely to think that parents would not accept SDF staining on their children’s anterior temporary teeth (45.3%), compared with staining on posterior temporary teeth (24.5%). Still, a sizable proportion of respondents were unsure whether their patients’ parents would accept SDF staining of posterior (30.2%) or anterior temporary teeth (39.6%) and 56.6% were unsure whether children would accept staining on any teeth. However, 56.6% strongly agreed/agreed that SDF is beneficial in remote communities. In addition, most participants agreed that use of SDF could decrease the number of pediatric patients requiring general anesthesia or sedation (83.0%). Lastly, just over half of dental professionals (50.9%) were unsure whether SDF was difficult to obtain because of lack of availability.
Regarding the use of SDF for older adults, most dental professionals strongly agreed/agreed that SDF would be ideal for treating coronal caries (90.6%) and root caries (98.1%) in patients in LTC facilities (Table 5). When it came to acceptance of SDF in this elderly patient population, 43.1% of dental professionals were unsure and 15.7% strongly agreed/agreed that the older adults in their practice would not accept SDF staining. Similar results were observed for substitute decision-makers/caregivers of older adults: 42.3% of dental professionals were unsure and 9.6% believed SDF staining would not be accepted by caregivers of seniors in their practice.
|
Statement |
Response, % (n = 53) |
|---|---|
| SDF is an ideal non-invasive treatment for coronal caries for older adults in long-term care facilities. | |
| Strongly disagree/disagree | 1.9 |
| Unsure | 7.5 |
| Strongly agree/agree | 90.6 |
| SDF is an ideal non-invasive treatment for root caries for older adults in long-term care facilities. | |
| Strongly disagree/disagree | 0 |
| Unsure | 1.9 |
| Strongly agree/agree | 98.1 |
| SDF staining would not be accepted by older adults in my practice. | |
| Strongly disagree/disagree | 41.2 |
| Unsure | 43.1 |
| Strongly agree/agree | 15.7 |
| SDF would not be accepted by the caregivers of the older population in my practice. | |
| Strongly disagree/disagree | 48.1 |
| Unsure | 42.3 |
| Strongly agree/agree | 9.6 |
Concerning the economics of SDF use for pediatric and older adult populations, participants had an overall view that SDF is more cost-effective than other ECC treatment options (75.5%), that its cost is more reasonable than alternative treatment options (77.4%) and that it would lower the cost of oral health care in LTC facilities (88.5%, Table 6).
|
Statement |
Response, % (n = 53) |
|---|---|
| SDF is more cost-effective than other early childhood caries treatment options currently available to me. | |
| Strongly disagree/disagree | 3.8 |
| Unsure | 20.8 |
| Strongly agree/agree | 75.5 |
| SDF cost is more reasonable compared with alternative treatment options in my community. | |
| Strongly disagree/disagree | 1.9 |
| Unsure | 20.8 |
| Strongly agree/agree | 77.4 |
| SDF is significantly difficult to obtain because of its cost. | |
| Strongly disagree/disagree | 54.7 |
| Unsure | 41.5 |
| Strongly agree/agree | 3.8 |
| SDF would lower the cost of oral health care in long-term care facilities. | |
| Strongly disagree/disagree | 0 |
| Unsure | 11.5 |
| Strongly agree/agree | 88.5 |
Participants were also positive about the workshop component of our study (Table 7). A majority strongly agreed/agreed that the workshop had changed their views on SDF use for ECC treatment (76.5%) and that it had made them more likely to choose SDF treatment for pediatric (82.4%) and older adult patients (87.8%).
|
Statement |
Response, % (n = 53) |
|---|---|
| The workshop and the information provided changed my views on the use of SDF for early childhood caries treatment. | |
| Strongly disagree/disagree | 15.7 |
| Unsure | 7.8 |
| Strongly agree/agree | 76.5 |
| The workshop made me more likely to choose SDF treatment for pediatric patients. | |
| Strongly disagree/disagree | 7.8 |
| Unsure | 9.8 |
| Strongly agree/agree | 82.4 |
| The workshop made me more likely to choose SDF treatment for older adult patients. | |
| Strongly disagree/disagree | 8.2 |
| Unsure | 4.1 |
| Strongly agree/agree | 87.8 |
Exploring differences between those who self-identified as dentists and non-dentists (dental hygienists, dental assistants, students and others) several surfaced. First, in terms of parental acceptance of SDF staining on their children’s anterior temporary teeth, there was a statistically significant difference of opinion (p = 0.030) between the 2 groups, with more dentists than non-dentists strongly agreeing/agreeing that this would not be accepted (Figure 2). When it came to SDF treatment for coronal caries in older adults in LTCs, all non-dentists agreed this would be an ideal non-invasive option; fewer dentists agreed with this perception (p = 0.007, Figure 3).
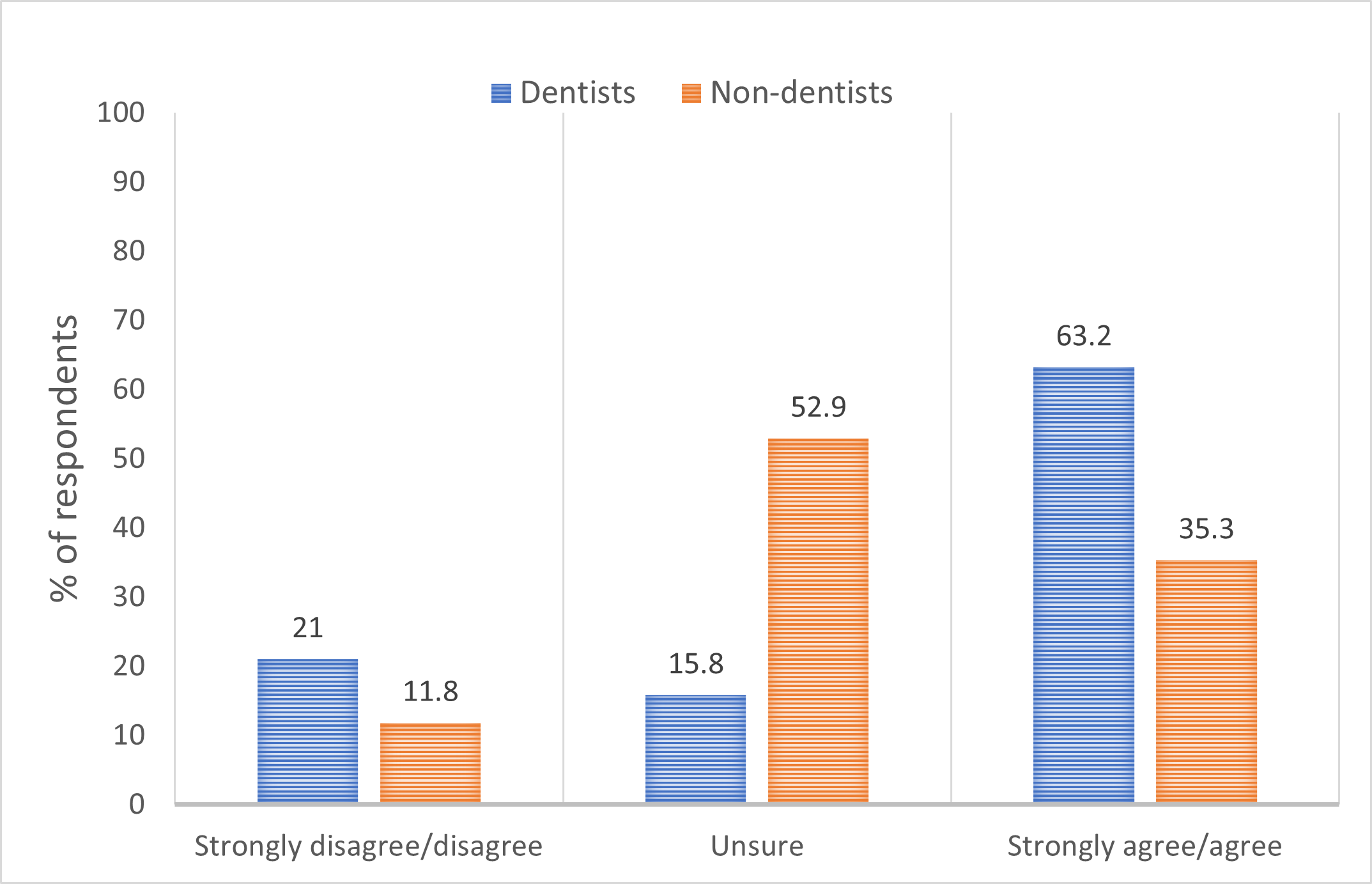
Figure 2: Difference in responses of dentists and non-dentists to the statement: parents of my patient population would not accept silver diamine fluoride staining on anterior temporary teeth (p = 0.030).
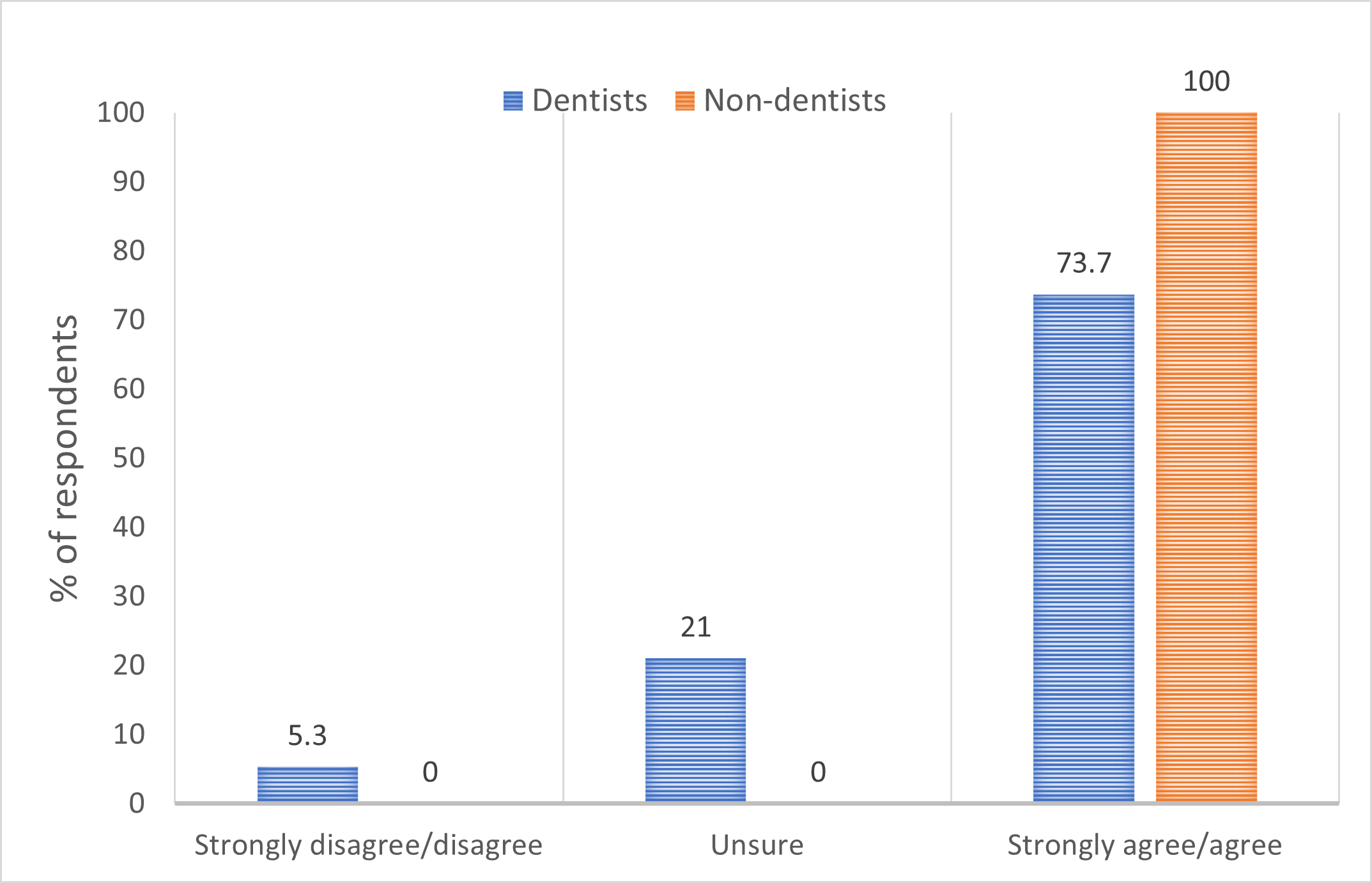
Figure 3: Difference in responses of dentists and non-dentists to the statement: silver diamine fluoride is an ideal non-invasive treatment for coronal caries for older adults in long-term care facilities (p = 0.007).
Lastly, the open-ended questions yielded interesting responses. For example, for both children and older adults, in addition to the staining issue, participants also had concerns about insurance coverage and fees, lack of patient knowledge of the material, non-compliance to recommended oral hygiene habits and frequency of visits (i.e., the need for reapplication).
Discussion
Acceptance and perceptions of the use of SDF as a caries management strategy for children and older adults were positive overall in this cohort of dental professionals working in northwestern Ontario. Although studied worldwide, this topic remains underreported in Canada, especially in areas with enormous responsibility for regional health care delivery, such as Thunder Bay. As we reflect on 7 years since Health Canada’s approval of SDF, it is important to identify opportunities for expanding its role. The continuing education workshop was beneficial to participants, as they considered diversifying their treatment options. In addition, survey responses regarding the cost and economic perceptions of SDF were also valuable in providing a full picture of these themes among the dental professionals surveyed.
The views of dental professionals related to the use and effectiveness of SDF in children agree with findings from similar studies. The main concern about SDF is staining, specifically of the front teeth,28–30 as we found in this study. Differences in dentists’ and non-dentists’ perceptions of parental acceptance of staining may indicate variation in the client populations of these professional groups. The fact that dental professionals see the value of SDF in potentially delaying the need for or avoiding sending children to the operating room for ECC treatment under general anesthesia is important where dental care in Northern Ontario is concerned. The literature suggests that general anesthesia is a reality for many children in Canada, especially those living in more remote areas.31,32 Our findings can be extrapolated to the broader Canadian and global context where similar geographic challenges exist and where admissions for treating ECC under general anesthesia could be reduced.
Our findings regarding the use of SDF for older adults also help paint a clearer picture, as this is a less-explored area, compared with SDF use in children. Although it has been suggested that SDF is accepted by older adults33,34 and caregivers34 in Singapore and Germany, many dental professionals in our study were “unsure” about the views of this cohort (43.1% for older adults and 42.3% for their caregivers). As the population of people ≥65 years in Canada increases (~17.5% in 2019 and 25% expected by 2040),35 use of SDF could be beneficial, as access to oral health services is a challenge for older adults.23 For instance, SDF can be easily applied in LTC homes or hospitals, and the treatment takes less time than more invasive dental procedures. Systematic reviews suggest that using SDF is beneficial in this age group,10,36,37 but further and more thorough clinical studies are warranted to understand effective use of this material in different scenarios (LTC facilities, functionally dependent patients, etc.).
Another underexplored topic is dental professionals’ perceptions of the economics and cost of using SDF. This is important as they are the ones who will recommend this treatment to their patients from an economic standpoint.38 Studies have shown that SDF is more cost-effective than treatment under general anesthesia in children in Australia8; in the USA, it aids in averting restorative costs.9 We found no studies analyzing cost factors for older adults. In addition, as suggested by study participants in the open-ended survey responses, information about insurance claim coverage should also be made more readily available to practitioners and their patients to allow informed decisions about whether to use SDF.
Understanding the educational impact that the workshop had on dental professionals was also of immense value to this study. A number of participants had not received education on SDF during their professional training. This may be reflective of the older age group that was sampled and the introduction of the material into the Canadian market less than 10 years ago. Fortunately, educational trends in teaching about SDF are changing in North America,39 although in Canada the curriculum may focus on the use of the material in children.18 Nevertheless, the fact that over 3 quarters of participants reported that the workshop had positively influenced their probable choice of SDF speaks to the power of having an accompanying educative component when rolling out SDF. This factor has been highlighted by Antonioni et al.40 who showed that education through publications (like this article) and continuing education courses (like the workshop) promoted the uptake of SDF. In a clinical setting, Weintraub et al.41 reported that, when studying SDF implementation facilitators, educative and feedback components (along with a detailed protocol presentation) were considered valuable by staff. Although the dental professionals in our study showed some skepticism pertaining to SDF’s clinical effectiveness and the staining, we believe there is an avenue for uptake if practitioners are better informed.
Regarding the limitations of this study, first, we used convenience sampling by inviting dental professionals in the Thunder Bay area to participate; omitting those who did not respond limits the generalizability of the results. Second, although piloted with practitioners in a similar context, no other validation on the instrument was carried out. Furthermore, although it was not the intention to evaluate SDF perceptions before and after the workshop, we acknowledge that the workshop could have influenced participants’ responses and, thus, we chose to include direct questions about the workshop’s influence. Finally, we also recognize that perceptions regarding harmful or adverse events associated with SDF, as well as acceptance of non-dental care professionals applying the material, could be useful, especially as a future area of inquiry. Nevertheless, the strengths of this study lie in the fact that it was carried out with a group of dental professionals — dentists and hygienists in Northern Ontario who mostly serve rural and Indigenous populations — that has been neglected in the literature. In addition, many of the topics that were addressed at the workshop and in the questionnaire are underexplored across different subgroups of the population, specifically regarding SDF use in the older adults and the inclusion of survey questions on dental professionals’ economic and cost perceptions of SDF.
This work comes at a propitious moment. Federal initiatives such as the Canadian Dental Care Plan, the Oral Health Access Fund and Indigenous-oriented Community Oral Health Services all seek to address barriers to oral health care access and delivery to various priority populations.42–44 It would be valuable to leverage these governmental initiatives and harness the public health benefits and patient/provider-friendly nature of SDF, especially in settings such as LTC facilities. Nevertheless, as highlighted in this study, the adoption of SDF in clinical settings must be pursued through adequate educative initiatives. Furthermore, as evidence regarding clinical and implementation effectiveness, as well as patient and provider perception accumulate in Canadian settings, public health agents must seize the momentum to push evidence-informed decisions when seeking funds and designing public health approaches.
Conclusion
Dental professionals in Northern Ontario showed a generally positive acceptance and perception of SDF as a caries management strategy for children and older adults. The accompanying educative component played a positive role in this regard. We believe that this approach should be adopted when SDF is introduced and used in populations living in geographic regions similar to Thunder Bay. Canadian dental professionals could greatly benefit from the use of SDF in circumstances and settings (e.g. rural/remote communities) like the ones explored in this study and more can be done to understand how this material’s benefits can be maximized.
THE AUTHORS
Corresponding author: Dr. Fabio Gregorio Arriola-Pacheco, Faculty of Dentistry, University of Toronto, 124 Edward St, Room 355, Toronto ON M5G 1G6, Canada. 416-864-8497; f.arriola@mail.utoronto.ca
Conflict of Interest: The authors have no conflicts of interest to disclose. The workshop speaker’s (Dr. Jeanette MacLean) honorarium was provided by Oral Science Canada and GC America. The authors have no commercial or professional relationship with either company and served only as organizers of the workshop.
Funding: Research was supported by the Canadian Institutes of Health Research, the Institute of Indigenous Peoples’ Health, the Nishtam Niwiipitan (My First Teeth) Study led by Dr. Herenia P. Lawrence (CIHR-IIPH grant no.: PI1-151324). Personal student funding was provided by the Mexican National Council of Humanities, Sciences and Technologies (CONAHCYT).
This article has been peer reviewed.
References
- Licensed natural health products database: Advantage Arrest. Ottawa: Health Canada; 2017. Accessed 2022 Nov. 16. https://health-products.canada.ca/lnhpd-bdpsnh/info?licence=80075746
- Premarket notification: diammine silver fluoride dental hypersensitivity varnish. Washington: United States Food and Drug Administration; 2014. Accessed 2022 Nov. 16. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm?ID=K102973
- Jiang CM, Duangthip D, Chan AKY, Tamrakar M, Lo ECM, Chu CH. Global research interest regarding silver diamine fluoride in dentistry: a bibliometric analysis. J Dent. 2021;113. doi: 10.1016/j.jdent.2021.103778
- Gao SS, Amarquaye G, Arrow P, Bansal K, Bedi R, Campus G, et al. Global oral health policies and guidelines: using silver diamine fluoride for caries control. Front Oral Health. 2021;2. doi: 10.3389/froh.2021.685557
- Crystal YO, Marghalani AA, Ureles SD, Wright JT, Sulyanto R, Divaris K, et al. Use of silver diamine fluoride for dental caries management in children and adolescents, including those with special health care needs. Pediatr Dent. 2017;39(5):135-45. PMID: 29070149
- Meyer BD, Hyer JM, Milgrom P, Downey T, Chi DL. Silver diamine fluoride-associated delays in procedural sedation in young children: a retrospective cohort study. J Am Dent Assoc. 2023;154(4):311-20. doi: 10.1016/j.adaj.2022.12.008
- Ending childhood dental caries: WHO implementation manual. Geneva: World Health Organization; 2019. https://apps.who.int/iris/handle/10665/330643?show=full
- Nguyen TM, Tonmukayakul U, Hall M, Calache H. Cost‐effectiveness analysis of silver diamine fluoride to divert dental general anaesthesia compared to standard care. Aust Dent J. 2022;67(4):352-61. doi: 10.1111/adj.12936
- Johhnson B, Serban N, Griffin PM, Tomar SL. Projecting the economic impact of silver diamine fluoride on caries treatment expenditures and outcomes in young U.S. children. J Public Health Dent. 2019;79(3):215-21. doi: 10.1111/jphd.12312
- Mungur A, Chen H, Shahid S, Baysan A. A systematic review on the effect of silver diamine fluoride for management of dental caries in permanent teeth. Clin Exp Dent Res. 2023;9(2):375-87. doi: 10.1002/cre2.716
- Chan AKY, Tsang YC, Jiang CM, Leung KCM, Lo ECM, Chu CH. Treating hypersensitivity in older adults with silver diamine fluoride: a randomised clinical trial. J Dent. 2023;136. doi: 10.1016/j.jdent.2023.104616
- Sabbagh H, Othman M, Khogeer L, Al-Harbi H, Al Harthi A, Abdulgader Yaseen Abdulgader A. Parental acceptance of silver diamine fluoride application on primary dentition: a systematic review and meta-analysis. BMC Oral Health. 2020;20(1):227. doi: 10.1186/s12903-020-01195-3
- Mohammed IE, Shariff N, Mohd Hanim MF, Mohd Yusof MYP, Md Sabri BA, Md Bohari NF, et al. Knowledge, attitudes and professional behavior of silver diamine fluoride among dental personnel: a systematic review. Children (Basel). 2022;9(12):1936. doi: 10.3390/children9121936
- Chai HH, Gao SS, Fung MHT, Duangthip D, Lo ECM, Chu CH. Principals’ perspectives on joining a kindergarten outreach dental service: a qualitative study. Int J Environ Res Public Health. 2022;19(19):12452. doi: 10.3390/ijerph191912452
- Chi DL, Milgrom P, Gillette J. Engaging stakeholders in patient-centered outcomes research regarding school-based sealant programs. J Dent Hyg. 2018;92(1):16-22. PMID: 29500281
- Kyoon-Achan G, Schroth RJ, Martin H, Bertone M, Mittermuller BA, Sihra R, et al. Parents’ views on silver diamine fluoride to manage early childhood caries. JDR Clin Trans Res. 2021;6(2):251-7. doi: 10.1177/2380084420930690
- Kyoon-Achan G, Schroth RJ, DeMaré D, Sturym M, Edwards J, Lavoie JG, et al. Indigenous community members’ views on silver diamine fluoride to manage early childhood caries. J Public Health Dent. 2020;80(3):208-16. doi: 10.1111/jphd.12370
- Brondani MA, Siarkowski M, Alibrahim I, Ribeiro CCC, Alves CMC, Donnelly LR, et al. An overview of pedagogical approaches to caries-control medications in Canadian dental and dental hygiene programs. J Can Dent Assoc. 2021;87:l1. PMID: 34343064
- Oral health Canada 2022 country profile. Geneva: World Health Organization; 2022. Available: https://www.who.int/publications/m/item/oral-health-can-2022-country-profile (accessed 2024 Jan. 18).
- Report on the findings of the First Nations Oral Health Survey (FNOHS) 2009-2010. Ottawa: First Nations Information Governance Centre; 2012. Available: https://fnigc.ca/wp-content/uploads/2020/09/fn_oral_health_survey_national_report_2010.pdf (accessed 2022 Jan. 13).
- The First Nations Regional Health Survey. Phase 3: volume one. Ottawa: First Nations Information Governance Centre; 2018. Available: https://fnigc.ca/wp-content/uploads/2020/09/713c8fd606a8eeb021debc927332938d_FNIGC-RHS-Phase-III-Report1-FINAL-VERSION-Dec.2018.pdf (accessed 2011 Jan. 13).
- Report on the findings of the oral health component of the Canadian Health Measures Survey 2007–2009. Ottawa: Health Canada; 2010. Available: https://publications.gc.ca/collections/collection_2010/sc-hc/H34-221-2010-eng.pdf (accessed 2024 Jan. 18).
- Levy BB, Goodman J, Eskander A. Oral healthcare disparities in Canada: filling in the gaps. Can J Public Health. 2023;114(1):139-45. doi: 10.17269/s41997-022-00692-y
- Sibley LM, Weiner JP. An evaluation of access to health care services along the rural-urban continuum in Canada. BMC Health Serv Res. 2011;11(1):20. doi: 10.1186/1472-6963-11-20
- Leimbigler B, Li EPH, Rush KL, Seaton CL. Social, political, commercial, and corporate determinants of rural health equity in Canada: an integrated framework. Can J Public Health. 2022;113(5):749-54. doi: 10.17269/s41997-022-00630-y
- McConkey S, Brar R, Blais G, Hardy M, Smylie J. Indigenous population estimates for the City of Thunder Bay. Toronto: Ministry of Health and Long-term Care; 2022. Available: http://www.welllivinghouse.com/wp-content/uploads/2022/06/ohc-thunder-bay_pop-estimates-factsheet_final_1June2022.pdf (accessed 2024 Feb. 2).
- Mashford‐Pringle A, Webb D. Appraising Canada’s 1979 Indian Health Policy: informing co‐development of distinctions‐based Indigenous health legislation. Can Public Admin. 2023;66(1):62-77. doi: 10.1111/capa.12512
- Seifo N, Cassie H, Radford J, Innes N. “It’s really no more difficult than putting on fluoride varnish”: a qualitative exploration of dental professionals’ views of silver diamine fluoride for the management of carious lesions in children. BMC Oral Health. 2020;20(1):257. doi: 10.1186/s12903-020-01243-y
- Chai HH, Kiuchi S, Osaka K, Aida J, Chu CH, Gao S. Knowledge, practices and attitudes towards silver diamine fluoride therapy among dentists in Japan: a mixed methods study. Int J Environ Res Public Health. 2022;19(14):8705. doi: 10.3390/ijerph19148705
- Crisp J, Mihas P, Sanders AE, Divaris K, Wright JT. Influences on dentists’ adoption of nonsurgical caries management techniques: a qualitative study. J Am Dent Assoc. 2021;152(6):463-70. doi: 10.1016/j.adaj.2020.10.001
- Da Silva K, Lionel A, O’Brien JM, Wright KD, Raazi M. The use of general anesthesia for pediatric dentistry in Saskatchewan: a retrospective study. J Can Dent Assoc. 2022;88(9):m9. PMID: 36322636
- Schroth RJ, Quiñonez C, Shwart L, Wagar B. Treating early childhood caries under general anesthesia: a national review of Canadian data. J Can Dent Assoc. 2016;82:g20. PMID: 27548666
- Sommerfeldt W, Gellert P, Müller A, Götze N, Göstemeyer G. Older patients’ perception of treating root caries with silver diamine fluoride — a qualitative study based on the Theoretical Domains Framework. J Dent. 2023;130:104408. doi: 10.1016/j.jdent.2022.104408
- Lee GKY, Tan MN, Gao X, Wee HL, Lai BWP, Hong CHL, et al. Acceptance of silver diamine fluoride use in community dwelling older adults, nursing home residents, and caregivers. J Dent. 2024;141:104819. doi:10.1016/j.jdent.2023.104819
- Aging and chronic disease: a profile of Canadian seniors. Ottawa: Public Health Agency of Canada; 2020. https://www.canada.ca/content/dam/hc-sc/documents/services/publications/diseases-and-conditions/aging-chronic-diseases/canadian-seniors-report_2021-eng.pdf (accessed 2024 Feb. 2).
- Chan AKY, Tamrakar M, Jiang CM, Tsang YC, Leung KCM, Chu CH. Clinical evidence for professionally applied fluoride therapy to prevent and arrest dental caries in older adults: a systematic review. J Dent. 2022;125:104273. doi:10.1016/j.jdent.2022.104273
- Farmer JW, Singhal S, Dempster L, Quiñonez C. Effectiveness, safety, and acceptance of silver diamine fluoride therapy and its implications for dental hygiene practice: position paper and statement from the Canadian Dental Hygienists Association. Can J Dent Hyg. 2018;52(3):192-207. https://files.cdha.ca/profession/SDF_Position_paper_cjdh_v52n3_FINAL.pdf (accessed 2024 Dec. 2).
- Sekhon M, Cartwright M, Francis JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. 2017;17(1):88. doi: 10.1186/s12913-017-2031-8
- Crystal YO, Janal MN, Yim S, Nelson T. Teaching and utilization of silver diamine fluoride and Hall-style crowns in US pediatric dentistry residency programs. J Am Dent Assoc. 2020;151(10):755-63. doi: 10.1016/j.adaj.2020.06.022
- Antonioni MB, Fontana M, Salzmann LB, Inglehart MR. Pediatric dentists’ silver diamine fluoride education, knowledge, attitudes, and professional behavior: a national survey. J Dent Educ. 2019;83(2):173-82. doi: 10.21815/JDE.019.020
- Weintraub JA, Birken SA, Burgette JM, Lewis TA, White BA. Use of the consolidated framework for implementation research to assess determinants of silver diamine fluoride implementation in safety net dental clinics. J Public Health Dent. 2019;79(4):298-306. doi: 10.1111/jphd.12324
- Farmer J, Singhal S, Gonheim A, Proaño D, Moharrami M, Kaura K, et al. Environmental scan of publicly financed dental care in Canada: 2022 update. Toronto: Dental Public Health, University of Toronto; 2022. https://caphd.ca/wp-content/uploads/2022/10/Canada-Dental-environmentscan-UofT-20221017.pdf (accessed 2024 Dec. 2)
- Canadian dental care plan. Ottawa: Government of Canada; 2024. https://www.canada.ca/en/services/benefits/dental/dental-care-plan.html (accessed 2024 Oct. 29).
- Oral health access fund. Ottawa: Government of Canada; 2024. https://www.canada.ca/en/services/health/healthy-living/dental-oral/oral-health-access-fund.html (accessed 2024 Oct. 29).






