Abstract
Purpose:
A specialized temporomandibular joint (TMJ) dental clinic was created at the Centre hospitalier universitaire (CHU) Sainte-Justine to optimize care of patients with juvenile idiopathic arthritis (JIA). In this article, we characteristics of patients with JIA and the resources available in Canadian pediatric hospitals for JIA patients with TMJ involvement.
Methods
To determine patient characteristics, we compiled retrospective data on patients seen at the TMJ clinic. Regarding resources available for patients with JIA, we sent questionnaires to the departments of rheumatology and dentistry of 13 Canadian pediatric hospitals.
Results:
Of the 86 JIA patients included in our study, 42% (95% confidence interval 32–52%) had TMJ involvement. Panoramic radiography was the imaging prescribed most often for patients with JIA (91%) and frequency of follow up was most often every 6 months. In the second part of the study, 7 hospitals were included; 2 had a specialized TMJ clinic. In many cases, reports of types of imaging and available dental specialists differed between the rheumatology and dentistry questionnaires for the same hospital.
Conclusions:
Few Canadian pediatric hospitals have a specialized TMJ clinic for JIA, and there seems to be a gap in the knowledge of primary care physicians regarding TMJ diagnosis and the management of patients with JIA.
Introduction
In the field of pediatric rheumatology, juvenile idiopathic arthritis (JIA) is the most common condition seen.1 In Canada, its prevalence is 3–100 per 100 000.2 JIA causes inflammation in 1 or more joints.3 Involvement of the temporomandibular joint (TMJ) occurs in about 40% of patients with JIA.4-7 Inflammation of the TMJ can affect the quality of life of a child, lead to facial asymmetry and malocclusion, limit mouth opening and impair mandibular growth.8-10 Chronic JIA affects psychosocial health throughout the patient's life and is responsible for early unemployment among young adults. Moreover, adults with JIA have a higher mortality rate than the general population.11 Without appropriate care, JIA can cause painful symptoms in affected children and irreversible sequelae in hard and soft tissues of the joints.8 Therefore, early detection and treatment by a multidisciplinary team are crucial to prevent and reduce the effects of this disease on the craniofacial complex.10,12
No professional body has defined the composition of a multidisciplinary team for management of diseases of the TMJ. However, the literature supports close collaboration among a pediatric rheumatologist, a radiologist, an oral and maxillofacial surgeon (OMFS), a pediatric dentist, an orthodontist and a physiotherapist.
In April 2019, the department of dentistry at the Centre hospitalier universitaire (CHU) Sainte-Justine established a specialized TMJ clinic to optimize care of patients with JIA. JIA patients are referred to this clinic for an initial screening. An OMFS assesses the patient, recommends diagnostic imaging if required and follows up or treats as needed.
Apart from an algorithm created to lead decision-making regarding JIA treatment, no accepted guidelines currently exist for the management of patients with JIA.12 Only 1 study describes which radiographs are most prescribed by OMFSs for JIA at the TMJ.13 More studies and consensus regarding follow-up intervals and imaging protocols are needed to develop recommendations and guidelines.
Although the importance of early diagnosis and treatment of TMJ involvement in JIA patients is known, access to care by a dental specialist is not always available. In Canada, there is currently no information on the resources available in pediatric hospitals for the care of patients with arthritis of the TMJ.
In light of these gaps in knowledge, our objectives were, first, to describe characteristics of patients seen in a novel TMJ clinic aimed at assessing and managing patients with JIA. Second, we aimed to determine resources available for JIA patents in pediatric hospitals across Canada.
Methods
Part 1: Characteristics of JIA Patients with TMJ Involvement
This descriptive retrospective study focused on patients seen at the CHU Sainte-Justine specialized TMJ clinic. The measures were characteristics of patients with JIA. Variables included patient's age and gender, the involvement of the TMJ, the specialty of the patient's dentist, the referent, the type of imaging used, the frequency of use of imaging, the types of JIA, medications, comorbidities, the frequency of follow up and treatments.
Eligibility Criteria
Included in the study were all patients with JIA seen between April 2019 and April 2021. Patients with incomplete information were excluded (Figure 1).
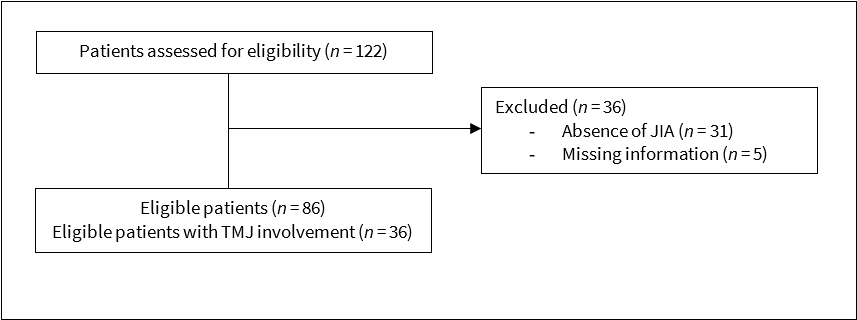
Figure 1: Flow chart showing selection of juvenile idiopathic arthritis (JIA) patients at the specialized temporomandibular joint (TMJ) clinic at Centre hospitalier universitaire Sainte-Justine.
Procedure
Patients at the CHU Sainte-Justine dental clinic are referred by a rheumatologist when they present signs or symptoms of TMJ involvement on examination. A diagnosis of JIA at the TMJ is made by the OMFS with the help of panoramic radiography, cephalometric radiography and a complete examination of the patient. When necessary and if possible, an MRI is used to confirm the diagnosis. Frequency of follow up is determined by the presence of JIA at the TMJ and the disease activity.
Treatment selection involves the OMFS, the pediatric rheumatologist, the patient and their family. Overall, decisions depend on progression of the disease, skeletal maturity and severity of the dentofacial deformity. For example, surgical treatment is performed at later stages, when arthritis is controlled. Arthroplasty is recommended in patients with significantly advanced JIA and whose mandibular growth is arrested by ankylosis at the TMJ. Intra-articular corticosteroid injection (IACI) is used with MRI-confirmed active JIA that does not respond well to medical treatments. Arthrocentesis is an alternative to IACIs. Orthodontics treatment is discussed and the OMFS may refer a growing patient for an orthopedic appliance to decrease dentofacial deformity. Patients are referred to an orthodontist for a distraction splint in case of pain and impaired TMJ function and to correct facial deformities. Pain and impaired TMJ function also result in a physiotherapy recommendation. Although much data on the description, effectiveness and indication for these treatments exist in the literature, almost no information exists on their clinical use.
At CHU Sainte-Justine’s dental clinic, we reviewed medical charts and collected demographic information; information regarding the disease: diagnosis and comorbidities; and management, including referring specialist, dental specialist managing the patient, the type of imaging used, the frequency of use of imaging, the frequency of follow ups and the treatments received.
Statistical Analysis
Descriptive statistics were used to describe the results. The mean ± standard deviation (SD), the proportion and 95% confidence interval (95% CI) for JIA patients with TMJ involvement were calculated.
Part 2: Resources Available for JIA Patients with TMJ Involvement in Canadian Pediatric Hospitals
In the second part of this study, 15 Canadian pediatric hospitals were potentially eligible to participate in this cross-sectional study through an online questionnaire.
Eligibility Criteria
All Canadian pediatric hospitals with a rheumatology department were eligible to participate. Hospitals whose department of pediatric rheumatology or dentistry completed at least 1 questionnaire were included. Hospitals where neither department responded to the invitation or submitted incomplete questionnaires were excluded from the analysis (Figure 2).
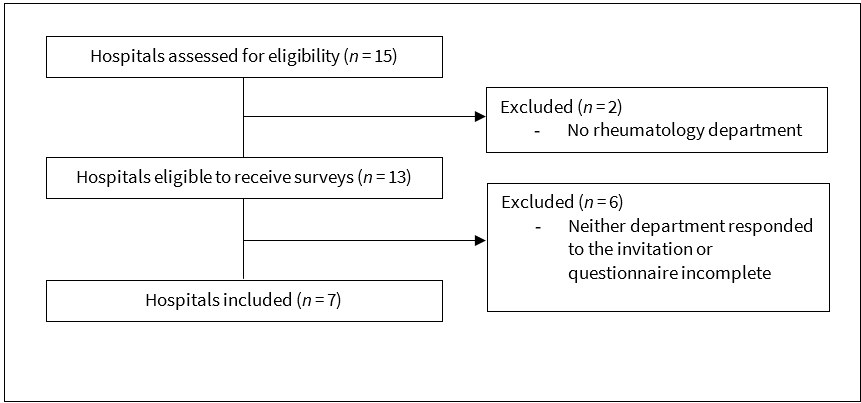
Figure 2: Flow chart showing selection of Canadian pediatric hospitals for participation in surveys.
Procedure
Because the study involved minimal risk, consent was recorded by survey response. An invitation email and a link to the questionnaire created using LimeSurvey were sent to the rheumatology and dentistry departments of each hospital. If there was no response after 1 month, a reminder email was sent.
Different questionnaires were sent to the departments of rheumatology and dentistry. They were aimed at determining the availability of specific resources for the care of JIA patients. The choices were based on suggested resources for the management of these patients in the literature.
The surveys consisted of multiple-choice questions and were divided into two sections. They focused on characteristics of the hospital environment as well as the resources available. The variables were the presence of a specialized TMJ clinic, the types of the professionals that refer a patient to the dental department, the disciplines involved in management teams within the hospital, the type(s) of imaging and the services offered in dentistry.
When the responses from rheumatology and dentistry at the same establishment were inconsistent in terms of the availability of a resource, the response from the professional whose department housed the resource was the one that was considered. The logic behind this decision was that the professional who has the resource in their department and uses it is inevitably more aware of its presence.
Statistical Analysis
Descriptive statistics were used to present the results. Means ± standard deviation (SD) and proportions (%) were calculated from the results obtained.
Ethics Approval
This study was approved by the research ethics board of CHU Sainte-Justine.
Results
Part 1: Characteristics of JIA Patients with TMJ Involvement
A total of 86 JIA patients at CHU Sainte-Justine’s TMJ clinic were included in the study and 36 of them (42%, 95% CI 32–52%) had involvement of the TMJ (Figure 1). Patients with JIA on the first visit were 3–18 years old (mean 10.95 ± 4.4 years); 90.7% were female and 9.3% were male. All patients were seen by an OMFS; 98% were referred to this clinic by pediatric rheumatologists while the remaining 2% were referred by an in-house dentist.
Descriptive Data
The use of imagery for JIA patients at the TMJ clinic is represented in Table 1. Frequency of imagery was based on panoramic radiography.
|
TMJ imagery |
No. patients (%) |
|---|---|
| Frequency | |
| Imagery has been taken 1 time or less, with no frequency repetition | 61 (71) |
| Every 6 months | 3 (3) |
| Every ≥ 12 months | 22 (26) |
| Types | |
| Panoramic radiograph | 78 (91) |
| Lateral cephalogram | 45 (52) |
| Antero-posterior cephalogram | 38 (44) |
| Magnetic resonance | 35 (41) |
| Magnetic resonance with contrast | 35 (41) |
| Cone-beam computed tomography | 0 (0) |
| Medical scan | 0 (0) |
| Ultrasound | 0 (0) |
| None | 6 (7) |
The most common follow-up frequency for these patients was every 6 months and the most common service provided was follow up of facial growth and TMJ symptoms, followed by orthodontic treatment (Table 2).
|
Characteristics |
No. patients (%) |
|---|---|
|
Note : RF = rheumatoid factor. |
|
| Types of JIA | |
| Oligoarthritis | 22 (61) |
| RF-positive polyarthritis | 1 (3) |
| RF-negative polyarthritis | 10 (28) |
| Psoriatic arthritis | 2 (6) |
| Arthritis with enthesitis | 0 (0) |
| Undifferentiated arthritis | 0 (0) |
| Systemic arthritis | 1 (3) |
| Medications | |
| None | 2 (6) |
| NSAIDs | 24 (67) |
| Adalimubab | 4 (11) |
| Etanercept | 6 (17) |
| Leflunomide | 0 (0) |
| Methotrexate | 20 (56) |
| Hydroxychloroquine | 0 (0) |
| Comorbidities | |
| Uveitis | 9 (25) |
| Gastrointestinal problems | 6 (17) |
| Chronic pain | 19 (53) |
| Follow-up frequency | |
| No follow up | 0 (0) |
| Every 3 months | 2 (6) |
| Every 6 months | 22 (61) |
| Every ≥ 12 months, as needed | 12 (33) |
| Treatments | |
| Facial growth and TMJ symptoms follow up | 34 (94) |
| Orthodontic treatment | 16 (44) |
| Bite plate/distraction splint | 7 (19) |
| Injections of intra-articular corticosteroids | 6 (17) |
| Physiotherapy | 2 (6) |
| Orthognathic surgery | 1 (3) |
| Arthrocentesis | 1 (3) |
| Joint reconstruction | 0 (0) |
Part 2: Resources Available for JIA Patients with TMJ Involvement in Canadian Pediatric Hospitals
A total of 7 hospitals participated in the survey for a response rate of 54% (7/13; Figure 2). Six questionnaires were completed by rheumatology departments and 6 by dentistry departments in these hospitals. All rheumatology respondents were pediatric rheumatologists. Dentistry survey respondents were pediatric dentists (67%) and OMFSs (33%).
Among the respondents, 2 pediatric hospitals have a specialized TMJ clinic and 1 of them pays particular attention to JIA. At the beginning of 2021, both clinics had been operating for 1–2 years. One offers screening and diagnosis for JIA patients, while the other also offers treatment.
According to responses from dental departments, all have an OMFS who takes care of JIA patients, and, in 50% of the hospitals’ dental clinics, pediatric dentists and orthodontists also play a role in follow ups. All surveys from dentistry departments indicated that pediatric rheumatologists refer JIA patients to their dental clinic. Some dentistry departments also indicated that patients are referred by health professionals, such as pediatricians (40%), otolaryngologists (20%) and external dentists (40%).
When asked about which professionals take charge of patients with TMJ arthritis in the hospital, rheumatology respondents provided a variety of responses depending on the hospital: plastic surgeon (33%), OMFS (83%), orthodontist (83%), pediatric dentist (67%), physiotherapist (67%), radiologist (50%), ophthalmologist (33%), orthopedist (17%) and dermatologist (17%).
When asked to dentistry respondents which departments in the hospital follow JIA patients with TMJ involvement, 83% of this group mentioned the rheumatology department and this same 83% group also mentioned the dentistry or oral and maxillofacial surgery department. The remaining 17% of dentistry respondents did not know.
When patients were referred to a dental professional for suspected arthritis of the TMJ, 4 hospitals out of 6 said they were referred in-house or to an affiliated hospital; the other 2 referred outside the hospital in the community.
We noted on multiple occasions that respondents from the department of rheumatology provided a different answer from their dental colleagues in the same hospital regarding which dental specialist manages JIA.
Use of Imagery
When asked what types of imaging are available for patients with JIA involving their TMJs, all dentists answered that they have access to MRI with and without contrast, anteroposterior and lateral cephalogram, panoramic radiography and medical scan. Some also have access to cone-beam computed tomography (CT; 67%) and ultrasound (83%). Rheumatologists also reported that they have access in the hospital to MRI with and without contrast and some have access to panoramic radiography (83%) and ultrasound (50%). Again, departments in the same hospital provided different answers regarding their access to imaging, specifically medical scans and panoramic radiography.
Treatments
Among the 6 participating hospitals, all offer imaging and monitoring of facial growth and symptoms; 5 offer arthrocentesis; 4 offer orthognathic surgery, joint reconstruction, intra-articular injection and distraction splint; and only 2 offer orthodontic treatment.
Discussion
In terms of improving management of JIA, this study highlights some findings regarding imaging and frequency of follow-up appointments.
First, our study confirms the clinical usefulness of panoramic radiography for JIA patients. According to a survey by Kinard and Abramowicz,13 panoramic radiography is the most frequently prescribed imaging for patients with JIA who are followed by OMFSs. In our study, JIA patients with TMJ involvement received panoramic radiography more often than other types of imaging (91%). This may be explained by its ease of use and low radiation emission compared with cone-beam CT.6,14 It can also be practical in certain situations when MRI is not recommended or is contraindicated; for example, when an uncooperative patient requires sedation before MRI and the child is not a candidate for sedation.15,16
Although MRI is the gold standard, its applicability in the clinical context is not always possible. Panoramic radiography is, therefore, not only an adjuvant to MRI, but a replacement tool along with clinical examination for detection and monitoring of JIA. Although it does not allow the detection of synovitis and the diagnosis of JIA in early stages, as MRI does, it should still have a place in future recommendations. In our opinion, this would also encourage rheumatologists to collaborate with a dental specialist who is equipped with panoramic radiography equipment and qualified for this type of follow up.
Second, the most popular follow-up frequency at the CHU Sainte-Justine clinic is every 6 months. Abramowicz et al.9 mention follow-ups every 3–6 months. To our knowledge, this is the only article that mentions follow-up time, and there is no current discussion in the literature about an appropriate interval for following patients with JIA of the TMJ. However, follow ups are important to monitor the progression of the disease and to prevent deterioration, as any change in disease activity may necessitate a change in treatment.
Hopefully, the practice at CHU Sainte-Justine’s clinic will provide useful data on follow-up frequency and imagery use to allow practitioners to reach a clear and scientific consensus. Further, we hope it will encourage other pediatric hospitals to create their own specialized clinic. With time and adequate numbers of patients, CHU Sainte-Justine’s clinic and others like it could combine in multi-centre trials to test treatment regimens for this challenging patient population.
In the second part of this study, we aimed to paint a current portrait of the resources available in Canadian pediatric hospitals for patients with arthritis at the TMJ. The results show that Canadian pediatric hospitals have a multitude of varied resources available for these patients. All hospitals surveyed have access to MRI with and without contrast which is the essential imagery for the diagnosis of JIA.8,14,17-20 However, only 2 of the 7 hospitals have a specialized TMJ clinic for JIA. OMFSs are the professionals with the largest role in Canadian pediatric hospitals in the management of JIA patients with TMJ involvement, but orthodontists and pediatric dentists also have an important role in some hospitals. This confirms that these 3 types of dental specialists are essential for diagnosis, follow up and complex treatment of these patients.10,21,22
We noted cases of different responses from 2 departments in the same hospital. This shows that some health professionals are not well informed about the imagery accessible for patients with JIA. It also reveals that rheumatologists are unfamiliar with the various dental specialists and their roles. This finding should encourage better communication between departments to improve understanding of the multidisciplinary care offered and promote consultation.
In comprehensive patient care, each member of the team plays an important role in the management of JIA.12,19,22-25 That of the pediatric rheumatologist is to perform a complete examination of joints, to define the activity of arthritis and to treat the disease by pharmacological therapy.22,24 The radiologist assists in the diagnosis and evaluates the disease through imaging. The OMFS is referred to for evaluation of TMJ involvement and restoration of the joint and the mandible.24 The pediatric dentist allows rapid detection and intervention through regular monitoring of the patient.11 Because JIA patients are known to have poor oral health, pediatric dentists play a role in monitoring dental hygiene and patient education.26 The orthodontist's responsibility is to periodically evaluate the patient’s dentofacial development through follow ups. If needed, they also take care of facial orthopedic treatment and evaluate morphological and occlusal alterations for surgical planning.6,11,22 The physiotherapist helps to reduce symptoms and establish normal function of the jaw.27 They help to maintain or improve range of motion of joints to increase joint endurance and strength and prevent injuries.28 Physiotherapy can also be used after prosthetic joint reconstruction surgery.29 The roles of all specialists should be known, as each specialist must be involved in patient care.
This study was limited in that the data from the TMJ specialized clinic cover only 2 years. This information is not sufficient to assess the adequacy of follow-up intervals, the frequency of imaging or the outcomes of treatments received. The survey sent to Canadian hospitals was not pilot tested. Moreover, the participation rate for the questionnaires was 54% (7 of 13 hospitals); thus, the responses may not reflect all Canadian pediatric hospitals. However, this participation rate is higher than in a similar study surveying treatment of JIA with TMJ involvement with OMFSs (33%).13
Conclusion
The clinic at CHU Sainte-Justine is one of the few in Canadian pediatric hospitals that pays particular attention to TMJ involvement in patients with JIA. It is useful for the management of these patients and offers a multitude of treatments. Data from this clinic may provide content for future recommendations regarding follow-up intervals and imaging protocols.
Most Canadian pediatric hospitals surveyed had access to care for patients with JIA affecting their TMJ. However, different departments in the same hospital had differing responses; thus, efforts should be made to promote interdisciplinary communication and collaboration in the interests of patient care.
THE AUTHORS
Corresponding author: Dr. Jasmine Thao Nguyen, Faculty of Dental Medicine, Université de Montréal, CP 6128, succ. Centre-Ville, Montréal QC H3C 3J7. jasmine.nguyen@umontreal.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References
- Barut K, Adrovic A, Şahin S, Kasapçopur O. Juvenile idiopathic arthritis. Balkan Med J. 2017;34(2):90-101.
- Oen K, Duffy CM, Tse SML, Ramsey S, Ellsworth J, Chédeville G, et al. Early outcomes and improvement of patients with juvenile idiopathic arthritis enrolled in a Canadian multicenter inception cohort. Arthritis Care Res (Hoboken). 2010;62(4):527-36.
- Oberle EJ, Harris JG, Verbsky JW. Polyarticular juvenile idiopathic arthritis — epidemiology and management approaches. Clin Epidemiol. 2014;6:379-93.
- Stoll ML, Sharpe T, Beukelman T, Good J, Young D, Cron RQ. Risk factors for temporomandibular joint arthritis in children with juvenile idiopathic arthritis. J Rheumatol. 2012;39(9):1880-7.
- Cannizzaro E, Schroeder S, Müller LM, Kellenberger CJ, Saurenmann RK. Temporomandibular joint involvement in children with juvenile idiopathic arthritis. J Rheumatol. 2011;38(3):510-5.
- Twilt M, Mobers SMLM, Arends LR, ten Cate R, van Suijlekom-Smit L. Temporomandibular involvement in juvenile idiopathic arthritis. J Rheumatol. 2004;31(7):1418-22.
- von Schuckmann L, Klotsche J, Suling A, Kahl-Nieke B, Foeldvari I. Temporomandibular joint involvement in patients with juvenile idiopathic arthritis: a retrospective chart review. Scand J Rheumatol. 2020;49(4):271-80.
- Abramowicz S, Kim S, Prahalad S, Chouinard AF, Kaban LB. Juvenile arthritis: current concepts in terminology, etiopathogenesis, diagnosis, and management. Int J Oral Maxillofac Surg. 2016;45(7):801-12.
- Abramowicz S, Levy JM, Prahalad S, Travers CD, Angeles-Han ST. Temporomandibular joint involvement in children with juvenile idiopathic arthritis: a preliminary report. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127(1):19-23.
- Frid P, Resnick C, Abramowicz S, Stoustrup P, Nørholt SE, Temporomandibular Joint Juvenile Arthritis Work Group TMJaw. Surgical correction of dentofacial deformities in juvenile idiopathic arthritis: a systematic literature review. Int J Oral Maxillofac Surg. 2019;48(8):1032-42.
- Hochberg MC, Gravallese EM, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH. Rheumatology. 7th ed. Amsterdam: Elsevier; 2019. 2048 p.
- Resnick CM, Frid P, Nørholt SE, Stoustrup P, Peacock ZS, Kaban LB, et al. An algorithm for management of dentofacial deformity resulting from juvenile idiopathic arthritis: results of a multinational consensus conference. J Oral Maxillofac Surg. 2019;77(6):1152.e1-33.
- Kinard BE, Abramowicz S. Juvenile idiopathic arthritis practice patterns among oral and maxillofacial surgeons. J Oral Maxillofac Surg. 2017;75(11):2333.e1-8.
- Pawlaczyk-Kamienska T, Pawlaczyk-Wróblewska E, Borysewicz-Lewicka M. Early diagnosis of temporomandibular joint arthritis in children with juvenile idiopathic arthritis. A systematic review. Eur J Paediatr Dent. 2020;21(3):219-26.
- Abramowicz S, Simon LE, Susarla HK, Lee EY, Cheon JE, Kim S, et al. Are panoramic radiographs predictive of temporomandibular joint synovitis in children with juvenile idiopathic arthritis? J Oral Maxillofac Surg. 2014;72(6):1063-9.
- Walker B, Conklin HM, Anghelescu DL, Hall LP, Reddick WE, Ogg R, et al. Parent perspectives and preferences for strategies regarding nonsedated MRI scans in a pediatric oncology population. Support Care Cancer. 2018;26(6):1815-24.
- Covert L, Van Mater H, Hechler BL. Comprehensive management of rheumatic diseases affecting the temporomandibular joint. Diagnostics (Basel). 2021;11(3):409.
- Müller L, Kellenberger CJ, Cannizzaro E, Ettlin D, Schraner T, Bolt IB, et al. Early diagnosis of temporomandibular joint involvement in juvenile idiopathic arthritis: a pilot study comparing clinical examination and ultrasound to magnetic resonance imaging. Rheumatology (Oxford). 2009;48(6):680-5.
- Stoustrup P, Twilt M. Improving treatment of the temporomandibular joint in juvenile idiopathic arthritis: let's face it. Expert Rev Clin Immunol. 2019;15(11):1119-21.
- Abramowicz S, Cheon JE, Kim S, Bacic J, Lee EY. Magnetic resonance imaging of temporomandibular joints in children with arthritis. J Oral Maxillofac Surg. 2011;69(9):2321-8.
- Stoustrup P, Resnick CM, Pedersen TK, Abramowicz S, Michelotti A, Küseler A, et al. Standardizing terminology and assessment for orofacial conditions in juvenile idiopathic arthritis: international, multidisciplinary consensus-based recommendations. J Rheumatol. 2019;46(5):518-22.
- Stoustrup P, Pedersen TK, Nørholt SE, Resnick CM, Abramowicz S. Interdisciplinary management of dentofacial deformity in juvenile idiopathic arthritis. Oral Maxillofac Surg Clin North Am. 2020;32(1):117-34.
- Frid P, Nordal E, Bovis F, Giancane G, Larheim TA, Rygg M, et al. Temporomandibular joint involvement in association with quality of life, disability, and high disease activity in juvenile idiopathic arthritis. Arthritis Care Res (Hoboken). 2017;69(5):677-86.
- Stoustrup P, Twilt M, Resnick CM. Management of temporomandibular joint arthritis in JIA: tradition-based or evidence-based? J Rheumatol. 2018;45(9):1205-7.
- Stoustrup P, Twilt M, Herlin T. Systemic treatment for temporomandibular joint arthritis in juvenile idiopathic arthritis. J Rheumatol. 2020;47(6):793-5.
- Walton AG, Welbury RR, Thomason JM, Foster HE. Oral health and juvenile idiopathic arthritis: a review. Rheumatology (Oxford). 2000;39(5):550-5.
- Kau CH, Allareddy V, Stoustrup P, Pedersen T, Kinard B, Cron RQ, et al. Management of juvenile idiopathic arthritis: preliminary qualitative findings from the National Dental Practice-Based Research Network. J World Fed Orthod. 2021;10(2):70-3.
- Onel KB, Horton DB, Lovell DJ, Shenoi S, Cuello CA, Angeles-Han ST, et al. 2021 American College of Rheumatology guideline for the treatment of juvenile idiopathic arthritis: therapeutic approaches for oligoarthritis, temporomandibular joint arthritis, and systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 2022;74(4):553-69.
- Svensson B, Feldmann G, Rindler A. Early surgical-orthodontic treatment of mandibular hypoplasia in juvenile chronic arthritis. J Craniomaxillofac Surg. 1993;21(2):67-75.




