ABSTRACT
Full-coverage bonded porcelain restorations offer predictable treatment options in dentistry, but a certain amount of tooth material must be removed to allow space for the required thickness of the restorative material. Laminate veneers and inlays are considered minimally invasive, but they also require removal of sound enamel. Sometimes, it may be preferable to extend the veneer preparations beyond the contact points toward the palatal surface, to hide the margins of the restoration, which necessitates removal of additional tissue. Improvements in adhesive technologies mean that small indirect restorations may be applied with removal of only a superficial layer of enamel. This clinical report describes a situation in which application of porcelain laminates and sectional veneers was chosen as the therapy of choice. A step-by-step protocol is proposed for cementation of these delicate restorations, and finishing procedures are described.
Introduction
A variety of treatment options are available to restore fractured, misaligned and malformed or hypoplastic anterior teeth. For many years, full-coverage crowns were indicated in this situation, but this treatment option is now considered invasive because of the need to remove tissue. Progress in adhesive technologies has made possible a variety of more conservative restoration techniques. For example, when the colour of the existing substrate (the patient’s teeth) is acceptable, thin porcelain laminate veneers (0.3–0.7 mm) may be suitable. The term “minimally invasive” is also used to describe full veneers that wrap around the teeth, although such restorations actually cover the buccal and palatal surfaces of the prepared teeth.1 When erosion has caused severe tooth loss, a wrap-around preparation cannot be considered minimally invasive, especially if there is a possibility of restoration with direct composites or ceramic sectional veneers, with no removal of sound enamel. Restoration of missing dental tissues with direct resin composites is quick and minimally invasive.2 This approach is inexpensive, the resulting restoration is easy to repair, and the esthetic results are acceptable.
The case report presented here describes minimally invasive treatment of anterior teeth with porcelain laminate and sectional veneers to restore esthetics and function.
Case Report
A 26-year-old female dental student was concerned about a fractured composite restoration on one of her anterior teeth, cervical marginal discoloration of the composite and the appearance of a black (i.e., open) triangle between the central incisors (Fig. 1). Another dentist had placed the restorations several years previously to restore her peg-shaped lateral teeth (Fig. 2), using a microhybrid resin composite. She reported that during the restoration process, her maxillary right canine had been damaged by the diamond bur used for finishing the restorations, but the damage had been left untreated (Fig. 3).
 Figure 1: Preoperative view of the patient’s face.
Figure 1: Preoperative view of the patient’s face.
 Figure 2: Intraoral view, showing the fracture on tooth 12, damage on the mesial side of tooth 13, the black (open) triangle and discoloration of the outlines of the direct composite resin veneer.
Figure 2: Intraoral view, showing the fracture on tooth 12, damage on the mesial side of tooth 13, the black (open) triangle and discoloration of the outlines of the direct composite resin veneer.
 Figure 3: Close-up microscopic photograph after removal of the direct resin veneer. Apparent damage on tooth 13 was reported to have occurred during finishing of the previous composite restoration.
Figure 3: Close-up microscopic photograph after removal of the direct resin veneer. Apparent damage on tooth 13 was reported to have occurred during finishing of the previous composite restoration.
During the first appointment, digital photographs and radiographs were obtained, and alginate impressions were made. No periodontal problems or carious lesions were found.
After relevant data were collected using a checklist of esthetic items and a schematic description of the clinical procedures had been presented, the treatment options were discussed with the patient.3,4 As a dental student, she was conscious of the benefits of preserving the dental tissues, and she did not want to sacrifice sound enamel. However, she had certain expectations about the final position, colour and surface texture of the teeth. The following comprehensive treatment plan was adopted: remove resin composite restorations, make impressions, roughen the teeth, control the fit of the restorations and adhesive cementation, and perform finishing and polishing of the bonded porcelain restorations.
Description of Minimally Invasive Restoration Procedure
Initial Considerations
In an esthetic rehabilitation in which the patient has high expectations, a mock-up or try-out with direct composite restorations can help in evaluating the patient’s esthetic demands.5 In this case, resin composite restorations were already present, and the planned alterations to the restoration were minor, so a mock-up was deemed unnecessary.
Restorations with inharmonious gingival display can have a detrimental effect on the appearance of the patient’s smile.6 In this case, however, the gingival scallop was optimal, oral hygiene was good, and no plaque or recessions were observed.
Preparation
Various preparation depths and 3 types of preparation forms have been described for porcelain laminate veneers, namely, window, overlapped and feathered preparations.7,8 To date, there is no consensus as to which preparation type is more resistant to fracture.7,8 Therefore, the least invasive preparation with maximal preservation of enamel is advisable.
In this case, an incisal overlap preparation was selected, to give the dental technician maximum control over esthetic characteristics and translucency. For the sectional veneers, no preparations were performed, except for removal of the resin composite restorations (Fig. 4). Although the veneer preparations extended into the enamel only (not into the dentin), an acrylic resin provisional restoration was positioned over all prepared teeth using the spot etch technique.
Fabrication of Laminate and Sectional Veneers
For fabrication of the laminates and sectional veneers (Vintage Al porcelain, Shofu, Kyoto, Japan), Nori-vest-alumina refractory dies (Noritake, Miyoshi, Japan) were used, in combination with alveolar models, to achieve better harmony with the gingival outline. Glass ceramic restorations were baked on the refractory dies. For the sectional veneers (0.01–0.5 mm thickness), small portions of dentin and various translucent ceramic powders were mixed according to the manufacturer’s instructions (Fig. 5). The porcelain laminates were 1 to 1.5 mm in thickness because of the coned tooth morphology. Restorations on these teeth required the use of a significant amount of dentin porcelain. The porcelain surfaces were stained for a natural-looking surface texture. The restorations were finished using stones (Dura-green stones, Shofu), diamond burs and abrasive papers (Meister Cones, Noritake), and a final fine polishing was performed with Pearl Surface F paste (Noritake).
 Figure 4: Intraoral view after removal of the direct resin composite restorations.
Figure 4: Intraoral view after removal of the direct resin composite restorations.
 Figure 5: Porcelain laminates and sectional veneers prepared on the refractory dies.
Figure 5: Porcelain laminates and sectional veneers prepared on the refractory dies.
Cementation
The sequence for surface conditioning of the inner surface of the porcelain laminates and sectional veneers is presented in Table 1, and the cementation sequence for these restorations appears in Table 2.
Table 1 Surface conditioning sequence for inner surface of porcelain laminates and sectional veneers
| Step | Action |
| 1 | Etching with hydrofluoric acid (1 min) |
| 2 | Rinsing with copious amounts of water (1 min) |
| 3 | Ultrasonic cleaning in distilled water (5 min) |
| 4 | Application of silane coupling agent, with allowance of time for evaporation (1 min) |
| 5 | Application of adhesive (no photopolymerization) |
| 6 | Application of cement on cementation surface of porcelain laminate and sectional veneers |
Table 2 Surface conditioning sequence for teeth and/or restoration complexes
| Step | Action |
| 1 | Application of rubber dam |
| 2 | Application of Mylar polyester strips around teeth to be conditioned |
| 3 | Roughening of enamel with diamond bur and air abrasion |
| 4 | Etching of enamel with 38% phosphoric acid (30 s) |
| 5 | Rinsing with water (1 min) |
| 6 | Application of adhesive (no photopolymerization) |
| 7 | Positioning of veneer with cement |
| 8 | Photopolymerization (10 s) |
| 9 | Removal of excess resin cement with probe |
| 10 | Application of glycerine gel |
| 11 | Photopolymerization from multiple directions (40 s each direction) |
| 12 | Removal of excess resin cement with diamond burs |
| 13 | Polishing of margins with polishing rubbers and polishing paste |
After placement of the rubber dam, adaptation at the marginal and proximal contacts was controlled under microscopic examination. With the translucent sectional veneers, it is important to control the colour of the restorations with a try-in paste (Variolink try-in paste, Ivoclar Vivadent, Schaan, Liechtenstein). At this stage, the restorations should present a chameleon (blending) effect. The colour of the laminate veneers was selected to match the restoration and the tooth, to ensure an invisible margin.
Surface Conditioning of Ceramic
The ceramic restorations were cleaned with copious amounts of water and then dried, after which the cementation surfaces were etched with 5% hydrofluoric acid (IPS Empress ceramic etching gel, Ivoclar Vivadent). Hydrofluoric acid selectively dissolves the glassy matrix or crystalline components of the ceramic to produce a porous, irregular surface.9-11 The microporosities on the ceramic increase the surface area and allow mechanical interlocking of the resin composite.
The laminates and sectional veneers were then cleaned ultrasonically to remove any remnants of particles of porcelain on the surface, which would diminish access of the adhesive to the undercuts.12
The next step was silanization with Monobond S silane coupling agent (Ivoclar Vivadent). Silane couples the inorganic particles present in the glass ceramics to the organic matrix of the resin cements. Use of hydrofluoric acid followed by silane facilitates the creation of high bond strengths, exceeding the cohesive strength of ceramic and the bonding strength of resin composite to enamel.12
Surface Conditioning of the Teeth
Before any adhesive procedures were applied to the teeth, the superficial outer layer of enamel was removed with diamond burs. After preparation, the enamel surfaces were conditioned with an etch-and-rinse adhesive bonding procedure, specifically, etching with 38% phosphoric acid (Ultradent, South Jordan, UT) for 30 seconds, followed by application of an adhesive (Excite, Ivoclar Vivadent) (Fig. 6).
Cementation of Laminate Veneers
For sectional veneers, which are very thin restorations, the thickness of the luting cement may affect the distribution of stress at the interface between the adhesive and the restoration.13 If the internal fit of an indirect restoration is poor, higher stresses may occur at this interface.13 In this case, the adaptation of the restoration was controlled under microscopic examination. In addition, during the laboratory procedures, no dye spacer was used, so as to achieve optimal adaptation of the restoration with minimal thickness of resin composite cement. Adhesive cement was applied on the inner surfaces of the restorations before insertion. After removal of excess cement, glycerine gel was applied at the margins to prevent an oxygen inhibition layer. The restorations were photopolymerized from the buccal and palatal directions. Excess resin composite was removed with an explorer, and the margins were finished and polished with diamond burs, rubber points (Fig. 7) and diamond polishing paste. The final result met the patient’s expectations (Figs. 8 and 9).
 Figure 6: Etching of a tooth with phosphoric acid.
Figure 6: Etching of a tooth with phosphoric acid.
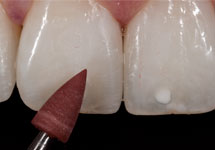 Figure 7: Finishing and polishing with a rubber point.
Figure 7: Finishing and polishing with a rubber point.
 Figure 8: Final intraoral view after placement of the porcelain laminates and sectional veneers.
Figure 8: Final intraoral view after placement of the porcelain laminates and sectional veneers.
 Figure 9: Photograph of the patient after treatment.
Figure 9: Photograph of the patient after treatment.
Discussion
Numerous previous studies provided information that helped to guide the treatment plan in this case. To begin, the selection of restoration type was an important consideration. In one clinical study, there was no significant difference in patient satisfaction with composite or ceramic laminate veneers immediately after placement, but after 2 years of clinical service, patients were significantly more satisfied with the ceramic restorations.14 In another study, survival rates for veneer restorations were 94% for porcelain restorations, 90% for indirect composite restorations and 74% for direct composite restorations.7 However, the material used for the restorations had no significant influence on absolute and relative failures. In yet another clinical study, direct resin composite veneers had a failure rate of 14% over 3 years of service, with a low incidence of marginal staining.15
Various clinical studies have shown that the survival rate for bonded porcelain laminate veneer restorations is more than 90% over 10 years of clinical service.16-19 In those studies, the failures reported were either cohesive ceramic fractures (the majority) or failures of the adhesive between the cement and the tooth surface.16-19 Adhesive-related failures could be attributed to the extent of tooth preparation. Particularly with deep preparations in dentin, less adhesion can be expected relative to enamel. In fact, the bond strength of composite cement to enamel is in the range of 40 MPa, sometimes exceeding the cohesive strength of enamel itself.20 Failure of the adhesive between cement and enamel was rarely observed.16-19 In addition to fractures, other types of failure, such as microleakage and debonding, have been reported.16-18
In this context, as an alternative to direct resin composite restorations, small pieces of thin ceramic veneers (“sectional veneers”) could be etched and adhered to enamel to restore the small defects, and this approach was applied in the current case. Preparation for sectional veneers requires removal of the superficial fluorosed 40-mm layer of enamel, to enhance adhesion to the enamel.21 Long-term clinical results for sectional veneers are not yet available. However, one of the most important aspects for long-term survival with these fragile restorations is the bonding procedure. Hence, the clinical success of the bonded porcelain restorations is largely determined by the quality of adhesion. For the ultimate esthetic outcome, a minimum thickness of resin cement at the interface is required, since resin composites are more prone to wear and discoloration than ceramic restorations. In particular, staining may be a problem if composite restorations are used for patients who smoke heavily; staining caused by smoking could be diminished with the use of ceramic restorations, because this material maintains its gloss and esthetic appearance for a long time.
As noted above, various preparation depths and types of preparation forms have been described for porcelain laminate veneers. Some manufacturers of dental ceramics recommend deep preparations to increase the strength of their ceramics, but these recommendations are based on studies performed with the materials alone, without consideration of the material–adhesive–tooth complex. The adhesion of thicker ceramic materials to teeth indicates tooth preparations that extend deep into the dentin. Conversely, the presence of thick ceramic veneers on minimally prepared teeth may lead to periodontal problems and bulky, less esthetic restorations because of overcontouring. It has been stated that laminates bonded to sound enamel have a good survival rate and that enamel adhesion should be considered the gold standard.18 Piemjai and colleagues22 concluded that minimal preparation, to achieve 0.5-mm porcelain thickness, resulted in better fracture strength than bonding to deeper preparations in dentin, to obtain 1.0-mm porcelain thickness. However, the differences were not statistically different.
In another study, preparations of 0.5 mm depth buccally, restored with bonded porcelain veneer (Empress), exceeded the strength of intact unprepared teeth.23 Comparable results were obtained when pressed ceramic veneers were cemented with Variolink II photo- and chemical-polymerized resin cement (Ivoclar Vivadent) to teeth with different preparation designs.1,15 The mean fracture strength of the unprepared teeth (713 N) was greater than but not significantly different from that of groups with other preparations. Therefore, minimal preparation seems advisable for adhesive bonding. However, it should be noted that shallow preparation often results in laminates with thin edges, with a high risk of fracture or chipping during the bonding procedures.6
In the case described here, the superficial outer layer of enamel was removed with diamond burs before adhesive procedures were undertaken. This procedure has been debated in the literature. For example, when 40 mm of fluorosed enamel was removed before restoration, the strength of the resin–enamel bond was improved.21,24 In the control group in the same study, with nonfluorosed enamel, some adhesives (e.g., Clearfil Protect Bond, Kuraray) performed better on prepared enamel, whereas other adhesives (e.g., Optibond FL, Kerr) had similar performance on enamel with and without preparation.
Bond strength is also affected by the type of adhesive. The total etch (3-step or etch-and-rinse procedure) and the self-etch (2-step) adhesives showed better bond strength in in vitro studies than the simplified all-in-one adhesives.20,25 On this basis, a simplified adhesive procedure cannot be recommended, as the adhesive strength is not comparable to that of the total etch procedure (the gold standard).
As noted above, the thickness of the luting cement may affect the distribution of stress at the interface between the adhesive and the restoration.13 In one in vitro study, thin laminates were cemented with a greater thickness of luting composite, but flaws were observed at the margins after cyclic loading.26 According to this study, the ratio of ceramic to luting composite should be above 3.0.26
In another in vitro study,27 increasing thickness of the cement led to a gradual decrease in fracture strength of the porcelain. Liu and colleagues28 obtained similar results in a finite element study in which cement thickness of less than 50 mm was proposed to reduce adhesive failures between cement and enamel.
Conclusion
This case report has described the restoration of the anterior dentition with porcelain laminates and sectional veneers. Adhesion, finishing and polishing procedures, which are considered key factors for clinical success, have been described in detail. The rationale for various choices in this treatment protocol has been detailed with reference to the pertinent literature. The use of porcelain laminates and sectional veneers could be a suitable alternative to conventional prosthetic approaches.
THE AUTHORS
References
- Stappert CF, Stathopoulou N, Gerds T, Strub JR. Survival rate and fracture strength of maxillary incisors, restored with different kinds of full veneers. J Oral Rehabil. 2005;32(4):266-72.
- Özcan M. Anterior restorations: Direct composites, veneers or crowns? In: Roulet JF, Kappert HF, editors. Statements: diagnostics and therapy in dental medicine today and in the future. New Malden: Quintessence; 2009. p. 45-67.
- Fradeani M. Esthetic rehabilitation in fixed prosthodontics. Volume 1. Esthetic analysis: a systematic approach to prosthetic treatment. Chicago (IL): Quintessence; 2004. p. 42-67.
- Devigius A. Treatment goal for the anterior segment – functional reconstruction or smile design. In: Roulet JF, Kappert HF, editors. Statements: diagnostics and therapy in dental medicine today and in the future. New Malden: Quintessence; 2009. p. 81-7.
- Reshad M, Cascione D, Magne P. Diagnostic mock-ups as an objective tool for predictable outcomes with porcelain laminate veneers in esthetically demanding patients: a clinical report. J Prosthet Dent. 2008;99(5):333-9.
- Bichacho N. Porcelain laminates: integrated concepts in treating diverse aesthetic defects. Pract Periodontics Aesthet Dent. 1995;7(3):13-23.
- Meijering AC, Creugers NH, Roeters FJ, Mulder J. Survival of three types of veneer restorations in a clinical trial: a 2.5-year interim evaluation. J Dent. 1998;26(7):563-8.
- Hui KK, Williams B, Davis EH, Holt RD. A comparative assessment of the strengths of porcelain veneers for incisor teeth dependent on their design characteristics. Br Dent J. 1991;171(2):51-2.
- Kramer N, Lohbauer U, Frankenberger R. Adhesive luting of indirect restorations. Am J Dent. 2000;13(Spec No):60D-76D.
- Özcan M, Vallittu PK. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater. 2003;19(8):725-31.
- Brentel AS, Özcan M, Valandro LF, Alarça LG, Amaral R, Bottino MA. Microtensile bond strength of a resin cement to feldspathic ceramic after different etching and silanization regimens in dry and aged conditions. Dent Mater. 2007;23(11):1323-31. Epub 2006 Dec 26.
- Blatz MB, Sadan A, Kern M. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 2003;89(3):268-74.
- Magne P, Versluis A, Douglas WH. Effect of luting composite shrinkage and thermal loads on the stress distribution in porcelain laminate veneers. J Prosthet Dent. 1999;81(3):335-44.
- Meijering AC, Roeters FJ, Mulder J, Creugers NH. Patients’ satisfaction with different types of veneer restorations. J Dent. 1997;25(6):493-7.
- Stappert CF, Ozden U, Gerds T, Strub JR. Longevity and failure load of ceramic veneers with different preparation designs after exposure to masticatory simulation. J Prosthet Dent. 2005;94(2):132-9.
- Friedman MJ. A 15-year review of porcelain veneer failure – a clinician’s observations. Compend Contin Educ Dent. 1998;19(6):625-8.
- Peumans M, van Meerbeek B, Lambrechts P, Vanherle G. Porcelain veneers: a review of the literature. J Dent. 2000;28:163-77.
- Peumans M, de Munck J, Fieuws S, Lambrechts P, Vanherle G, van Meerbeek B. A. prospective ten-year clinical trial of porcelain veneers. J Adhes Dent. 2004;6(1):65-76.
- Fradeani M, Redemagni M, Corrado M. Porcelain laminate veneers: 6- to 12-year clinical evaluation –a retrospective study. Int J Periodontics Restorative Dent. 2005;25(1):9-17.
- de Munck J, van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, et al. A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res. 2005;84(2):118-32.
- Ermis RB, De Munck J, Cardoso MV, Coutinho E, Van Landuyt KL, Poitevin A, et al. Bonding to ground versus unground enamel in fluorosed teeth. Dent Mater. 2007;23(10):1250-5. Epub 2007 Jan 9.
- Piemjai M, Arksornnukit M. Compressive fracture resistance of porcelain laminates bonded to enamel or dentin with four adhesive systems. J Prosthodont. 2007;16(6):457-64. Epub 2007 Aug 2.
- Hahn P, Gustav M, Hellwig E. An in vitro assessment of the strength of porcelain veneers dependent on tooth preparation. J Oral Rehabil. 2000;27(12):1024-9.
- Ibarra G, Vargas MA, Geurtsen W. Interfacial and surface characterization of two self-etching adhesive systems and a total-etch adhesive after bonding to ground and unground bovine enamel – a qualitative study. Clin Oral Investig. 2006;10(4):331-41. Epub 2006 Nov 21.
- Breschi L, Mazzoni A, Ruggeri A, Cadenaro M, Di Lenarda R, De Stefano Dorigo E. Dental adhesion review: aging and stability of the bonded interface. Dent Mater. 2008;24:90-101. Epub 2007 Apr 17.
- Magne P, Kwon KR, Belser UC, Hodges JS, Douglas WH. Crack propensity of porcelain laminate veneers: a simulated operatory evaluation. J Prosthet Dent. 1999;81(3):327-34.
- Scherrer SS, de Rijk WG, Belser UC, Meyer JM. Effect of cement film thickness on the fracture resistance of a machinable glass-ceramic. Dent Mater. 1994;10(3):172-7.
- Liu HL, Lin CL, Sun MT, Chang YH. Numerical investigation of macro- and micro-mechanics of a ceramic veneer bonded with various cement thicknesses using the typical and submodeling finite element approaches. J Dent. 2009;37(2):141-8. Epub 2008 Dec 11.
