ABSTRACT
Objectives: To explore the demographic characteristics and clinical features among patients with osseous (cemento-osseous) dysplasia (OD/COD) of the jaws and to determine the frequency of particular radiographic characteristics.
Methods: The charts and radiographic reports of 118 patients with OD/COD, obtained from the archives of the University of Toronto discipline of oral and maxillofacial radiology, were reviewed. Demographic and clinical data, radiographic findings and final diagnoses were collected and analyzed to determine typical characteristics.
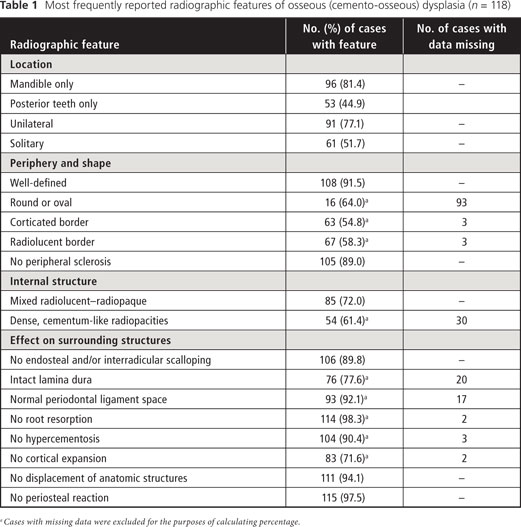
Results: Of the 117 patients for whom age and sex were known, the majority (97 [82.9%]) were female; these female patients had a mean age (± standard deviation) of 44.3 ± 13.4 years. Eighty-three (72.2%) of the 115 patients for whom symptoms were known were clinically asymptomatic. Ninety-three patients (78.8%) had OD/COD at single sites (i.e., periapical OD/COD), and 25 (21.2%) had OD/COD at multiple sites (i.e., florid OD/COD). In addition, 15 (12.7%) of the cases were associated with one or more simple bone cysts, and 13 (11.0%) were associated with osteomyelitis. In most cases, the OD/COD was unilateral, with the lesion being located in the mandible, usually associated only with the posterior teeth. The lesions exhibited well-defined, sclerotic or corticated margins (108 patients [91.5%]) and were surrounded by a radiolucent border. Minimal effects on surrounding structures were observed. As well, 85 (72.0%) of the lesions were in the mixed radiolucent–radiopaque stage, with dense, cementum-like radiopacities.
Conclusions: The majority of cases of OD/COD occurred in women in the fifth decade of life, and most cases were asymptomatic. OD/COD was more likely to present as solitary lesions but also occurred in association with simple bone cysts or osteomyelitis.
Introduction
The term “benign fibro-osseous lesion” refers to a group of non-neoplastic conditions in which normal bone is replaced with a fibrous connective tissue matrix containing abnormal bone or cementum.1 Histopathologically, these entities are composed of spindle-shaped, fibroblast-like cells and collagen, with only a few interspersed trabeculae of bone and cementum-like calcified material.2-4 One specific entity included in this group of conditions and occurring in the jaws is cemento-osseous dysplasia. The World Health Organization (WHO) has referred to this entity as “osseous dysplasia” (OD) and has acknowledged “cemento-osseous dysplasia” (COD) as a synonym.5 This terminology has resulted in some confusion in the literature.
In 1994, before the more recent publication of the WHO’s recommended terminology,5 the term “focal cemento-osseous dysplasia” was suggested by Summerlin and Tomich,2 primarily according to the location of dysplastic areas of bone (i.e., in the tooth-bearing areas of the posterior jaws and at extraction sites). The dysplastic lesions were identified as focal or periapical OD/COD on the basis of location only (i.e., posterior vs. anterior) because the 2 types of lesion share the same clinical, radiographic and histologic features.
Then, in its 2005 publication, the WHO described 3 clinical presentations of OD/COD5:
- periapical OD/COD: dysplastic lesions occurring in the anterior mandible and involving only a few adjacent teeth
- focal OD/COD: similar to periapical OD/COD, but with the limited number of lesions occurring in a posterior jaw quadrant (rather than in the anterior mandible)
- florid OD/COD and familial gigantiform cementoma: more extensive forms, occurring bilaterally in the mandible or in all jaw quadrants
OD/COD is usually confined to the tooth-bearing areas of the jaws or to edentulous alveolar processes.6 Immature lesions are characterized by a dearth of calcified material, whereas more mature lesions are characterized by the development and coalescence of dense, globular masses of calcified material.
The general dentist has an important role in the diagnosis of OD/COD, because the histopathologic presentation of this lesion is highly similar to that of other bone dysplasias. These similarities make it difficult to definitively diagnose the condition on the basis of microscopic features alone.2,7 The general dentist can determine the correct diagnosis in most cases of OD/COD, thus preventing unnecessary surgical intervention, by a thorough medical history, a complete intraoral examination, adequate radiographic investigation and application of knowledge. OD/COD represents a spectrum of conditions. However, for the purposes of the current study, OD/COD was considered to represent 2 main conditions: periapical OD/COD (synonymous with focal OD/COD), defined as a condition related to one or more anterior or posterior teeth, and florid OD/COD, defined as a condition with more extensive involvement (at least 2 quadrants).
The differential diagnosis of OD/COD may vary with the stage of development of the lesion. Radiographically evident changes to the internal radiolucency or radiopacity of these entities occur over time. In many of the numerous cases of OD/COD that have been misdiagnosed and/or mismanaged,8-11 the lesions were identified in their early stages, when their radiolucent appearance mimicked periapical rarefying osteitis (i.e., radicular abscess, granuloma or cyst), and unnecessary endodontic treatment was initiated. In the mixed radiolucent–radiopaque stage and the radiopaque stage, the differential diagnosis might include chronic sclerosing osteomyelitis, cemento-ossifying fibroma, odontoma and osteoblastoma.3,12-14 Distinguishing among these conditions may be made even more difficult by the confusing literature with regard to classification, diagnosis and management.13 The association of OD/COD with simple bone cysts and complications related to secondary infection or osteomyelitis further complicates the diagnosis.
Given the current understanding of OD/COD, new cases are often diagnosed solely on the basis of radiographic features.15 Therefore, familiarity with the various radiographic presentations of these lesions is imperative for correct diagnosis and may prevent unnecessary or inappropriate management. This study was undertaken with the aim of exploring the demographic and clinical features of OD/COD and determining the frequency of particular radiographic characteristics.
Methods
A retrospective analysis of the charts and radiographic reports of patients with OD/COD was undertaken. The cases had been catalogued between 1990 and 2007 in the files of the Special Procedures Clinic, operated through the discipline of oral and maxillofacial radiology at the University of Toronto, in Toronto, Ontario. The study was approved by the university’s Institutional Health Sciences Review Board.
Cases were selected on the basis of the definitive diagnosis, by 1 of 2 specialists in oral and maxillofacial radiology, at the time of original treatment (i.e., over the period 1990 to 2007). The specialists’ diagnoses were based on plain radiographs and advanced imaging (computed tomography [CT] or magnetic resonance imaging [MRI]), when available. For all patients, panoramic, occlusal and/or periapical plain radiographs were available. Advanced imaging (CT and/or MRI) was available for 23 cases.
Demographic and clinical data and the radiographic diagnoses were collected from the patients’ charts. The data were analyzed using SPSS software version 16.0 (SPSS Inc., Chicago, IL). Univariate analysis of the data involved descriptive statistics (i.e., frequencies and proportions) for qualitative variables and measures of central tendency and dispersion for quantitative variables.
Results
Demographic Characteristics and Clinical Features
The retrospective analysis of cases catalogued between 1990 and 2007 revealed 118 patients with a definitive diagnosis of OD/COD.
Of the 118 patients, age and sex were known for all but one person. Of these 117 patients, most (97 [82.9%]) were female, and the age range of these female patients was 13 to 73 years (mean ± standard deviation 44.3 ± 13.4 years). The 20 male patients (17.1%) ranged in age from 13 to 70 years (mean 40.1 ± 13.9 years). For all but 3 of the 118 patients, clinical features had been recorded. Of these 115 patients, 83 (72.2%) were clinically asymptomatic, whereas the remaining 32 patients (27.8%) reported one or more of the following symptoms: pain, swelling, tooth sensitivity or tooth mobility. The ethnic background of each patient was not recorded in the charts of the Special Procedures Clinic, nor was this detail recorded by any of the referring clinicians. As such, it was not feasible to analyze any potential patterns of occurrence in relation to ethnicity.
Types of OD/COD and Associated Pathoses
The majority of OD/COD lesions (93 [78.8%]) were categorized as periapical, and the remaining 25 (21.2%) were categorized as florid. In a minority of cases (15 [12.7%]), the lesion was associated with one or more simple bone cysts (5 cases [4.2% of total] involving florid OD/COD and 10 cases [8.5% of total] involving periapical OD/COD). Moreover, 13 (11.0%) of the cases were associated with osteomyelitis (6 cases [5.1% of total] involving florid OD/COD and 7 cases [5.9% of total] involving periapical OD/COD). A more detailed description of the association of OD/COD with simple bone cysts can be found elsewhere.16
Radiographic Features of OD/COD
The radiographic features of the 118 cases of OD/COD were retrieved from the archived radiographic reports. The most frequent features reported in these reports are summarized in Table 1. More than half of the OD/COD cases presented as solitary, unilateral lesions in the posterior mandible. Most of the lesions were well defined, with a radiolucent border surrounded by a radiopaque border, and most were mixed radiolucent and radiopaque internally, with no effects on surrounding structures.
Follow-up Data
For only 3 patients, all of whom had florid OD/COD, was follow-up information available (for periods ranging between 2 and 17 years). In 2 of the 3 cases, more internal radiopacities developed, which were associated with simple bone cysts that enlarged over time. In the third patient, secondary osteomyelitis developed.
Discussion
The term “benign fibro-osseous lesion” is well known and widely used. It encompasses a broad range of conditions, the diagnosis of which can be both challenging and confusing.13 OD/COD is a specific entity within this group of conditions. Its differential diagnosis should take into account the stage of development of the lesion and the possibility of associated entities, including osteomyelitis and simple bone cysts.17 In numerous cases, clinicians have failed to identify key clinical or radiographic features, which has resulted in misdiagnosis and/or mismanagement of the condition.8-11
It is well established that OD/COD may occur in people of all ages and all ethnic groups, but it is more common among middle-aged individuals of Asian, East Asian or African descent, followed by those of white background.15,18 Although information on patients’ ethnic background was not available in the charts reviewed for this study, the population of the Greater Toronto Area is highly diverse, and it might be safely assumed that the patients in this retrospective analysis represented a range of ethnicities. The majority of the patients in this study were female, and although they ranged in age from 13 to 73 years, the mean age for the female patients was 44.3 ± 13.4 years. These results are in general agreement with other studies showing that OD/COD occurs more commonly among women in the fourth and fifth decades of life.14,19,20 Su and colleagues14 also reported a wide age range (10 to 79 years) in their sample of 239 cases of OD/COD. The young age of some individuals in the current study may reflect the radiographic basis of the study. Younger patients with OD/COD may be asymptomatic, with the condition being identified incidentally on imaging studies performed for other purposes. The patient populations in studies involving histopathologic examination are often older, and individuals have typically presented with one or more clinically evident symptoms.19
In a recent systematic review, MacDonald-Jankowski20 reported that 64% of all cases of focal OD/COD were found incidentally. The majority of patients in the current study (72.2%) were clinically asymptomatic, a value slightly higher than that in other published reports.12,14,20 Again, this higher incidence may be attributable to the radiological nature of the study. The remaining patients (27.8%) presented with signs or symptoms of pain and swelling. Although the series of 54 patients with OD/COD described by Kawai and colleagues12 was based on radiologic findings, those authors reported that 32 patients (59%) presented with at least one of the following signs or symptoms: pain, gingival swelling, purulent discharge, tenderness on palpation or delayed wound healing after extraction. Indeed, most of these patients had secondary infection, and 15% had an initial diagnosis of mandibular osteomyelitis. Clinically apparent lesions presented with jaw swelling, dull pain or sensitivity, and drainage, which may have been due to secondary infection caused by direct exposure of the calcified masses to the oral cavity.15 Such symptoms might occur without an obvious dental cause.6,15 Exposure of the calcified masses might occur as a result of progressive atrophy of the alveolar process beneath a denture or after extraction of adjacent teeth.6,21
Although a majority of the cases of OD/COD in the current study were diagnosed on the basis of conventional dental radiographs, radiography was supplemented in 23 cases with advanced imaging (CT or MRI). Advanced imaging was performed in cases where conventional radiographs did not suggest the definitive diagnosis, in cases where a simple bone cyst was identified and those in which osteomyelitis was suspected. Advanced imaging provided additional information related to the extent of involvement, the presence of buccal or lingual expansion, the integrity of the periphery of the lesion, the internal density of the lesion and, for lesions that were particularly large, relationships with nearby anatomic structures.
The reported distribution of OD/COD varies according to subtype. Periapical or focal OD/COD lesions are solitary, whereas florid OD/COD lesions are distributed more or less symmetrically as multiple sclerotic masses, located in one or more quadrants, usually in the tooth-bearing regions of the jaws.4,15,18,21 In the study reported here, most of the OD/COD lesions were solitary (51.7%) and unilateral (77.1%). In addition, 78.8% of the lesions were periapical in nature, and the remaining 21.2% were florid. It was difficult to compare the relative proportions of periapical and florid lesions in this study with data in other published reports, since most of the previous literature consists of single case reports or small series of either periapical/focal OD/COD or florid OD/COD.
The majority of the OD/CODs in this study (81.4%) involved the mandible only, and about half (44.9%) involved the posterior teeth only. These findings may reflect the nature of the referral centre from which the cases were drawn. The lesions in such cases may have had an unusual appearance and may therefore have been more challenging for practitioners outside the field of oral and maxillofacial radiology.
Few studies have examined the periphery or border details of OD/COD lesions. Su and colleagues14 reported that in 53% of 142 cases of focal OD/COD, the lesions had well-defined borders. In contrast, Summerlin and Tomich2 reported that in most of their 221 cases of focal OD/COD, the periphery was poorly defined. However, in the discussion section of their paper, these authors described the majority of entities as being “fairly well-defined.” It is evident from these apparently contradictory statements that their definitions of “poorly defined” and “fairly well defined” were not clear; furthermore, the authors may not have calibrated their descriptions of radiographic features, which led to confusing statements. A complete or partial radiolucent rim was noted in a few reports12,13,22 and a sclerotic border has been less frequently reported2,14,22 (Fig. 1). Unfortunately, none of these authors2,12-14,22 reported the frequencies or proportions of individual radiographic features. The radiographic images of cases of OD/COD in the current study were analyzed and reported by 1 of 2 specialists in oral and maxillofacial radiology. Each of these radiologists had a different style of reporting, and some radiographic features of OD/COD were not mentioned in several of the archived reports. In this retrospective analysis, 91.5% of the OD/COD lesions were reported to have well-defined borders with a sclerotic or corticated periphery (54.8%) and a radiolucent internal rim (58.3%).

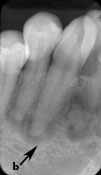


Figure 1: Periapical radiographs of osseous (cemento-osseous) dysplasia: (a to c) mandibular teeth with primarily radiolucent periapical areas and others with cementum-like internal radiopacities surrounded by a radiolucent band (arrows); (d) a well-defined corticated simple bone cyst with evidence of inter-radicular scalloping (arrow).
The wide spectrum of radiographic appearances of periapical OD/COD has been described in previous reports, which have included one or more presentations. Early-stage lesions have presented as periapical radiolucent defects that subsequently developed minute radiopacities. At a later stage, these minute radiopacities enlarged, coalesced and underwent further substantial radiopacification.2,12,14 These radiopacities could consist of dense, cementum-like structures and/or areas with a ground-glass appearance surrounded by a radiolucent periphery. The internal radiopacities were irregular or globular/ovoid in shape.15,19,21 Most cases of OD/COD reported here were in the mixed radiolucent–radiopaque stage (72.0%), and the internal radiopacities were described as being dense and cementum-like (61.4%). The radiographic findings in the current study are in agreement with the literature.19,20
A point of clinical controversy is whether OD/COD causes expansion of the affected jaw. A few published pathology-based reviews have described OD/COD lesions as nonexpansile.13,23 However, in other studies involving examination of occlusal radiographs,4,12,21 slight expansion of at least one of the mandibular cortical plates has been reported, with intact but thinned cortices. In the current study, occlusal radiographs were not available for all 118 cases, and bony expansion could not be comprehensively analyzed.
An association between OD/COD and simple bone cysts was first recognized by Melrose and colleagues4 in their 1976 study of 34 patients with florid OD/COD. Concomitant simple bone cysts are occasionally seen in association with OD/COD, but only a few case series have reported this association.4,6,24-26 In the current study, 12.7% of cases were associated with simple bone cysts (with two-thirds of these cases occurring in association with periapical OD/COD and one-third in association with florid OD/COD).
The progressive deposition of cementum-like calcifications, the hallmark of lesion maturation in OD/COD, increases the risk of secondary infection and osteomyelitis (Fig. 2). This deposition may occur because of poor vascularity of the altered dysplastic tissue when there is communication with the oral cavity.16 Only 13 (11.0%) of 118 patients with OD/COD in this study presented with concomitant osteomyelitis. Of these cases, 4 were related to an edentulous area. Kawai and colleagues12 reported that OD/COD was accompanied by osteomyelitis in 14.8% of their 54 cases, and Groot and colleagues16 reported that diffuse sclerosing osteomyelitis occurred in association with florid OD/COD in 31.3% of their 16 cases. Although they affect only a small number of patients, the potential for complications of this type to arise because of exposure through tooth extraction sites, bone loss from periodontal disease or implant placement should be recognized. Indeed, Waldron and colleagues27 recommended that every effort be made to avoid extraction of teeth in patients with florid OD/COD, because several patients had experienced poor socket healing and even formation of a sequestrum following extraction of teeth intimately associated with the cemental masses. Unless the OD/COD is symptomatic, treatment is usually not performed, because development and maturation of the lesion is self-limiting.15,20,21
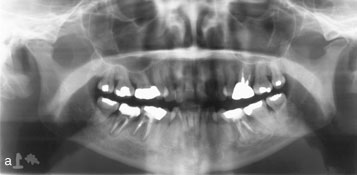



Figure 2: A 50-year-old woman with osseous (cemento-osseous) dysplasia (OD/COD) and osteomyelitis. Panoramic (a) and periapical (b) radiographs show a mostly radiopaque OD/COD lesion accompanied by lamellar periosteal formation of new bone along the buccal surface of the mandible. The lesion can be seen opposite the mandibular left first molar in a standard occlusal radiograph of the mandible (c) and a transverse computed tomography image (d).
The current study had several limitations. First, the sample of 118 cases was subject to referral bias. The cases referred to this institution may have been relatively difficult to diagnose, given the observed associations of OD/COD with simple bone cysts and osteomyelitis and the frequency of OD/COD as solitary posterior lesions rather than the classic mandibular anterior lesions. Presumably, less complex cases are easily managed by general practitioners, without the need to consult an oral and maxillofacial radiologist.
OD/COD represents a group of entities with radiographically variable appearance. Most of the patients with OD/COD in this study were women in their mid-40s, and most were asymptomatic. Cases of OD/COD were most likely to present as solitary, well-defined, corticated entities with globular cementum-like radiopacities, and only a small proportion presented in association with simple bone cyst. The favoured conservative approach to managing these conditions involves clinical and radiologic follow-up. Intervention may cause secondary infection of the cementum-like radiopacities, which may in turn induce osteomyelitis in a certain proportion of cases.
THE AUTHORS
References
- White S, Pharoah M. Oral radiology: principles and interpretation. 6th ed. St. Louis, MO: Mosby Inc.; 2009.
- Summerlin DJ, Tomich CE. Focal cemento-osseous dysplasia: a clinicopathologic study of 221 cases. Oral Surg Oral Med Oral Pathol. 1994;78(5):611-20.
- Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasias and cemento-ossifying fibromas: I. A pathologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(3):301-9.
- Melrose RJ, Abrams AM, Mills BG. Florid osseous dysplasia. A clinical-pathologic study of thirty-four cases. Oral Surg Oral Med Oral Pathol. 1976;41(1):62-82.
- Barnes L, Eveson JW, Reichart P, Sidransky D, editors. Pathology and genetics of head and neck tumours. World Health Organization Classification of Tumours. Lyon: IARC Press; 2005.
- Mahomed F, Altini M, Meer S, Coleman H. Cemento-osseous dysplasia with associated simple bone cysts. J Oral Maxillofac Surg. 2005;63(10):1549-54.
- Waldron CA. Fibro-osseous lesions of the jaws. J Oral Maxillofac Surg. 1993;51(8):828-35.
- Galgano C, Samson J, Kuffer R, Lombardi T. Focal cemento-osseous dysplasia involving a mandibular lateral incisor. Int Endod J. 2003;36(12):907-11.
- Smith S, Patel K, Hoskinson AE. Periapical cemental dysplasia: a case of misdiagnosis. Br Dent J. 1998;185(3):122-3.
- Islam MN, Cohen DM, Kanter KG, Stewart CM, Katz J, Bhattacharyya I. Florid cemento-osseous dysplasia mimicking multiple periapical pathology—an endodontic dilemma. Gen Dent. 2008;56(6):559-62.
- Resnick CM, Novelline RA. Cemento-osseous dysplasia, a radiological mimic of periapical dental abscess. Emerg Radiol. 2008;15(6):367-74. Epub 2008 Aug 23.
- Kawai T, Hiranuma H, Kishino M, Jikko A, Sakuda M. Cemento-osseous dysplasia of the jaws in 54 Japanese patients: a radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87(1):107-14.
- Brannon RB, Fowler CB. Benign fibro-osseous lesions: a review of current concepts. Adv Anat Pathol. 2001;8(3):126-43.
- Su L, Weathers DR, Waldron CA. Distinguishing features of focal cemento-osseous dysplasia and cemento-ossifying fibromas. II. A clinical and radiologic spectrum of 316 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(5):540-9.
- Ogunsalu C, Miles D. Cemento-osseous dysplasia in Jamaica: review of six cases. West Indian Med J. 2005;54(4):264-7.
- Groot RH, van Merkesteyn JP, Bras J. Diffuse sclerosing osteomyelitis and florid osseous dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81(3):333-42.
- Chadwick JW, Alsufyani NA, Lam EW. The clinical and radiographic features of solitary and cemento-osseous dysplasia-associated simple bone cysts. Dentomaxillofac Radiol. 2011;40(4):230-5.
- Cho BH, Jung YH, Nah KS. The prevalence, clinical and radiographic characteristics of cemento-osseous dysplasia in Korea. Korean J Oral Maxillofac Radiol. 2007;37:185-9.
- MacDonald-Jankowski DS. Florid cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2003;32(3)141-9.
- MacDonald-Jankowski DS. Focal cemento-osseous dysplasia: a systematic review. Dentomaxillofac Radiol. 2008;37(6):350-60.
- Goncalves M, Pispico R, Alves Fde A, Lugao CE, Goncalves A. Clinical, radiographic, biochemical and histological findings of florid cemento-osseous dysplasia and report of a case. Braz Dent J. 2005;16(3):247-50. Epub 2006 Jan 12.
- Beylouni I, Farge P, Mazoyer JF, Coudert JL. Florid cemento-osseous dysplasia: report of a case documented with computed tomography and 3D imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85(6):707-11.
- Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2(3):177-202. Epub 2008 May 13.
- Adachi K, Shigehara H, Ochi S, Nakatsu T, Akita K, Kishi K. Clinico-radiographic evaluation of simple bone cyst accompanied by radiopaque lesions. Oral Radiology. 1993;9(1):27-34.
- Saito Y, Hoshina Y, Nagamine T, Nakajima T, Suzuki M, Hayashi T. Simple bone cyst. A clinical and histopathologic study of fifteen cases. Oral Surg Oral Med Oral Pathol. 1992;74(4):487-91.
- Higuchi Y, Nakamura N, Tashiro H. Clinicopathologic study of cemento-osseous dysplasia producing cysts of the mandible. Report of four cases. Oral Surg Oral Med Oral Pathol. 1988;65(3):339-42.
- Waldron CA, Giansanti JS, Browand BC. Sclerotic cemental masses of the jaws (so-called chronic sclerosing osteomyelitis, sclerosing osteitis, multiple enostosis, and gigantiform cementoma). Oral Surg Oral Med Oral Pathol. 1975;39(4):590-604.
