Case Presentation
In September 2008, a 5-year-old child was referred to our department for evaluation of a lesion on the mandibular mucosa that had been increasing in size over 3 months. Intraoral examination showed a firm, well-demarcated, painless, blue-grey macula involving the alveolar mucosa in the area vestibular to the primary mandibular left canine (Fig. 1). The lesion failed to respond to the blanching test. There was no other unusual pigmentation on the oral mucosa or the lips, and no pathologic changes were visible on periapical radiographs of the involved mandibular region. An excisional biopsy was performed to remove the lesion completely and analyze it. A full mucoperiosteal flap was raised, revealing an abundance of granulation tissue and residues of solid black granules. Histologically, the specimen revealed interstitial edema of the corium accompanied by accumulation of solid brownish granules resembling pencil graphite (Fig. 2). There were no cellular atypia to suggest melanoma.
 Figure 1: Intraoral view showing a blue-grey tattoo in the area vestibular to the primary mandibular left canine.
Figure 1: Intraoral view showing a blue-grey tattoo in the area vestibular to the primary mandibular left canine.
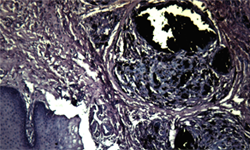 Figure 2: Histologically, the specimen showed interstitial edema of the corium and accumulation of brownish granules resembling pencil graphite (hematoxylin and eosin, original magnification ×100).
Figure 2: Histologically, the specimen showed interstitial edema of the corium and accumulation of brownish granules resembling pencil graphite (hematoxylin and eosin, original magnification ×100).
What is the Diagnosis?
Differential Diagnosis
Pigmented lesions, which are common in the mouth, may be of endogenous or exogenous origin. Oral pigmentation can be related to a wide range of factors, such as physiologic changes, foreign-body implantation, manifestations of systemic diseases and malignant neoplasms.1,2 In the differential diagnosis, it is important to distinguish between benign and malignant lesions and to include a thorough medical history, extraoral and intraoral examinations and laboratory studies. The clinician should also determine the onset and duration of the lesion, the presence of systemic signs and symptoms, drug use and smoking habits as well as the number, distribution, size, shape and colour of the pigmentation. Blue, brown, grey and black discolourations, along with vascular lesions, are all found in the oral mucosa.3,4
Red, Blue and Purple Vascular Pigmentation
In childhood, focused red or blue-purple pigmentation of the oral tissues can often be a congenital vascular lesion, such as hemangioma, presenting as benign proliferation of vascular channels and spontaneously regressing after puberty. The most common oral site for these lesions is the mouth, where the reddish-blue lesion generally appears as an asymptomatic flat or raised spot that blanches on pressure.
In adults, vascular malformations tend to persist and, especially in the elderly, lingual varicosities may occur as soft blue, red or purple elevations on the ventral surface of the tongue. This pathologic venous dilation is often located on the lower lip as a blue nodule that may appear after lip or cheek biting. These nodules blanche on pressure, except when the varix contains a thrombus.2
Non-blanching vascular pigmented lesions include hematomas, petechiae, purpurae and ecchymoses. These usually occur after a trauma as a consequence of blood extravasation into the soft tissues or spontaneously because of some defect in the hemostatic mechanism, such as idiopathic thrombocytopenic purpura. The colour of such lesions varies from red-blue to blue-black and is closely related to the degradation of hemoglobin in the extravascular spaces. Generally, the appearance of the oral tissues gradually returns to normal in about 2 weeks.2,5
Brown Melanotic Pigmentation
An endogenous pigment, melanin is synthesized by melanocytes and transferred to keratinocytes to protect the skin against exposure to the sun. Melanocytes are neural-crest-derived cells that reside in the basal epithelial layer of the skin and oral mucosa. Brown or blue pigmented lesions may be caused by overproduction of melanin in basilar melanosis or in benign nevi and malignant melanomas, which are associated with melanocyte overpopulation.1,4 Many pigmented lesions of the oral cavity are caused by melanin pigment.
Oral melanotic macules are brown-to-black benign lesions related to increased production of melanin in the basal cell layer of the epithelium; they are usually localized on the lip, gingiva, palate or buccal mucosa. If such pigmentation persists after 2 weeks, ecchymosis can be excluded and the differential diagnosis should include nevus and melanoma. Oral melanotic macules do not cause an increase in the number of melanocytes and are not associated with a predisposition to melanoma.6 Biopsy for routine histopathologic examination is recommended to rule out oral melanoma in patients with melanotic macule on the palate, where malignant melanoma is most prevalent.7,8
Other rare causes of focused oral pigmentation are the nevocellular nevus and blue nevus. Unlike melanotic macule, pigmented nevi are characterized by benign proliferation of basal-layer (nevocellular nevus) or dermal (blue nevus) melanocytes. Because the dermal melanocytes proliferate within the deep connective tissue, overlying blood vessels cover the brown melanin resulting in the typical blue tint on the skin. In the oral mucosa, both blue and nevocellular nevi appear as a brown nodule, and it may be difficult to differentiate clinically among a pigmented nevus, a melanotic macule, an exogenous tattoo and melanoma.4
Oral melanoacanthoma is another melanotic lesion that should be differentiated from other intraoral pigmented lesions. This uncommon, benign pigmentation of the oral mucosa is characterized by proliferation of dendritic melanocytes throughout the epithelium. The clinical presentation is a flat or slightly raised brown-to-black macular lesion, generally solitary, which occurs predominantly in the buccal mucosa of young black females.2 Oral melanoacanthoma is usually an asymptomatic lesion without malignant potential; it may represent a physiologic or reactive process. A biopsy is necessary to distinguish this lesion from other oral melanocytic pigmentation.4,7
The malignant proliferation of atypical melanocytes at the epithelial–connective tissue interface is the distinctive feature of oral melanoma. This rare lesion accounts for less than 1% of all oral malignancies, and it is generally encountered in the 5th decade, with greater incidence in men than women. The most common site in the oral cavity is the anterior aspect of the hard palate, followed by the anterior labial gingiva.8 Clinically, oral melanoma is an asymptomatic, slow-growing, brown-to-black macule with irregular, asymmetric borders. Eventually, a melanoma may present as a rapidly enlarging mass with bleeding, ulceration, bone destruction and pain or as a non-pigmented (amelanotic) lesion. Malignant melanoma is a fatal disease, and a biopsy should be performed of any pigmented oral lesion with irregular or asymmetric margins.7,8
Grey or Black Exogenous Pigmentation
The most frequent type of exogenous localized oral pigmentation is the amalgam tattoo. The usual clinical aspect is a grey, bluish-grey or black macular stain, which is usually seen on the gingival or alveolar mucosa. This lesion is the consequence of iatrogenic introduction of amalgam into the submucosa during removal of an old filling or extraction of restored teeth. In exceptional cases, this pigmentation may be due to galvanism between metal alloys in the mouth, during which mercury diffuses through soft tissue developing the tattoo.9 Tissue response to amalgam depends on the particle size and composition, and a foreign-body reaction with a mononuclear inflammatory cell infiltrate is often noted. Amalgam tattoo is an innocuous pigmentation, and intraoral radiographs can be used to identify the metallic particles when they are large enough.9,10
Rationale for Diagnosis
In exploring the differential diagnosis of a rare case of intraoral graphite pigmentation in a young patient, we have described the most important localized pigmentations of the oral cavity that the clinician may encounter in daily practice. An adequate differential diagnosis is essential to exclude the possibility of malignancy. In general, benign pigmented lesions have regular borders, small dimensions, symmetry and colour uniformity; in contrast, the typical malignant clinical aspect includes surface ulceration, colour variation and irregular borders. For focal pigmented lesions, a biopsy is necessary to arrive at a definitive diagnosis.
During early childhood, intraoral graphite implantation may cause focal pigmentation through accidental injury with a graphite pencil. The traumatic event usually takes place in the classroom during grade school, and it tends to involve the palate or the vestibular aspect of the gingiva. The lesion appears as a focal, grey-to-black macule, and a history of injury can confirm the initial diagnosis. Neither graphite nor amalgam tattoos require removal, but a biopsy is recommended to exclude melanoma when a grey-to-black pigmented lesion appears in areas distant from any restored teeth or in the absence of previous injury with a graphite pencil. Microscopically, solid granules in a chronic inflammatory cell infiltrate present the same histopathologic aspect in both graphite and amalgam tattoos.10
THE AUTHORS
References
- Eisen D. Disorders of pigmentation in the oral cavity. Clin Dermatol. 2000;18(5):579-87.
- Neville BW, Damm DD, Allen CM, Bouquot JE. Dermatologic diseases. In Oral & maxillofacial pathology. 2nd ed. Philadelphia: W.B. Saunders; 2002. p. 643-704.
- Wood NK, Goaz PW, Sawyer RP. Intraoral brownish, bluish, or black conditions. In Wood NK, Goaz PW, editors. Differential diagnosis of oral and maxillofacial lesions. 5th ed. St. Louis: Mosby; 1997. p. 182-208.
- Müller S. Melanin-associated pigmented lesions of the oral mucosa: presentation, differential diagnosis, and treatment. Dermatol Ther. 2010;23(3):220-9.
- Carpenter WM, Rudd M. Focal, flat pigmentations of the oral mucosa: a clinical approach to the differential diagnosis. J Calif Dent Assoc. 2000;28(12):949-54.
- Kaugars GE, Heise AP, Riley WT, Abbey LM, Svirsky JA. Oral melanotic macules. A review of 353 cases. Oral Surg Oral Med Oral Pathol. 1993;76(1):59-61.
- Femiano F, Lanza A, Buonaiuto C, Gombos F, Di Spirito F, Cirillo N. Oral malignant melanoma: a review of the literature. J Oral Pathol Med. 2008;37(7):383-8. Epub 2008 Feb 17.
- Hicks MJ, Flaitz CM. Oral mucosal melanoma: epidemiology and pathobiology. Oral Oncol. 2000;36(2):152-69.
- McCullough MJ, Tyas MJ. Local adverse effects of amalgam restorations. Int Dent J. 2008;58(1):3-9.
- Witman PM, Rogers RS 3rd. Pediatric oral medicine. Dermatol Clin. 2003;21(1):157-70.



