Abstract
Objective: The aim of this study was to determine and analyze the survival rates of dental implants placed by undergraduate dental students under supervision at the University of Alberta’s School of Dentistry over a 10-year period.
Methods: Charts from patients who received either single or multiple dental implants between 1 January 2007 and 31 July 2017 were reviewed. Patients’ age, sex, American Society of Anesthesiologists (ASA) class and implant site data were extracted and compiled for statistical analysis.
Results: Of 299 implants placed in 189 patients, 1 failed and required removal.
Conclusion: In this study, the survival rate of implants placed over a 10-year period was 99.7%. Supervision by certified specialists, strict case selection criteria and maintenance and care protocols at the university’s dental clinic likely contribute to the high survival rate.
For more than 30 years, dental implants have been a safe, successful and commonly used means for replacing teeth of partly or completely edentulous patients.1-4 Implants provide benefits compared with tooth-supported fixed partial dentures or removable partial dentures in partly edentulous patients and implant-supported prostheses offer a significant quality of life improvement for fully edentulous patients.5
However, implants do not come without complications. One of the most significant is implant failure resulting in removal of the implant. A 2013 systematic review2 comparing long-term survival of teeth and implants over 15 or more years reported 0–33% failure for implants. Another systematic review6 had similar results, with an implant survival rate of 73.4–100% (mean 94.6%) after at least 10 years. A study7 of survival rates for single implants provided by postgraduate students and specialist practitioners at a dental school estimated a failure rate of 2.7%. In 2008, the survival rate of dental implants placed by oral and maxillofacial surgeons or periodontists and restored by dental students was found to be 93%.4
The aim of our study was to determine the survival rate of single-implant crowns, multi-unit implant restorations and implant-supported complete dentures placed and restored by undergraduate dental students between 2007 and 2017.
Materials and Methods
Charts from all patients who received dental implants between 1 January 2007 and 31 July 2017 at the University of Alberta School of Dentistry’s undergraduate clinic were reviewed, and patients’ age, sex, American Society of Anesthesiologists (ASA) status, implant site, implant brand, implant size and restoration type were extracted and compiled in a spreadsheet for analysis and comparison with other published studies.
Ethics approval was received from the University of Alberta Research Ethics Office, project no. Pro00080965.
Results
During the study period, 299 implants were placed in 189 patients — 77 males and 112 females — whose average age was 52.26 years (Table 1). Each implant was placed by a different supervised 4th-year dental student. Five specialist practitioners — oral and maxillofacial surgeons, periodontists or prosthodontists — oversaw the surgical placements and prosthodontists oversaw the restorative aspects of treatment. The average time of the most recent recall examination after the day of implant placement was 709.1 days (range: 7–2677 days). Yearly recalls are suggested to these patients; however, of the 189 patients in our study, 83 had a recall appointment in 2015, 2016 or 2017. Implant types included 288 Replace Select Tapered (Nobel Biocare, Richmond Hill, Ont.) and 11 soft tissue level SLA surface implants (Straumann Canada, Burlington, Ont.; Table 2). During the 10-year study period, only 1 implant failed; it required removal after 77 days because of bone loss and failure of osseointegration.
|
Note: ASA = American Society of Anesthesiologists. |
|
| Total implants placed | 299 |
| Total no. patients | 189 |
| Sex | |
| Male | 77 |
| Female | 112 |
| Average patient age, years | 52.26 |
| ASA status | |
| 1 | 77 |
| 2 | 104 |
| 3 | 8 |
| No. implant failures | 1 |
|
Characteristic |
Nobel Replace Select Tapered (n = 288) |
Straumann Standard Plus (soft tissue level) SLA (n = 11) |
|---|---|---|
| Width, mm (no.) | 3.5 (7) 4.3 (177) 5 (103) 6 (1) |
3.3 (2) 4.1 (5) 4.8 (4) |
| Length, mm (no.) | 8 (13) 10 (98) 11.5 (57) 13 (110) 16 (10) |
6 (1) 8 (2) 10 (4) 12 (4) |
In terms of site, 92 implants were placed in the maxilla with 2 in the anterior region, 68 in the bicuspid and 22 in the molar region (Table 3). Of the 207 mandibular implants, 55 were in the anterior region (54 implants were used to support 27 different complete lower dentures), 41 in the bicuspid and 111 in the molar region. There were 154 single implant crowns, 91 implants in multi-unit restorations and 54 in edentulous mandible overdentures (Table 4).
|
|
Anterior |
Premolar |
Molar |
Total |
|---|---|---|---|---|
|
Note: CMD = Complete Mandibular Denture |
||||
| Maxilla | 2 | 68 | 22 | 92 |
| Mandible | 55 (54 in 27 CMD) | 41 | 111 | 207 |
| Total | 57 | 109 | 133 | 299 |
|
Type |
No. implants |
|---|---|
| Single crown | 154 |
| Multi-unit fixed partial denture | 91 |
| Mandibular overdenture | 54 (in 27 patients) |
Discussion
We found an implant survival rate of 99.7%, with only 1 implant removed during the 10-year study period. Similar results were obtained by Pettersson and Sennerby,8 who reported 99.6% survival of Replace Select Tapered implants (Nobel Biocare), and by van Velzen et al.,3 with 99.7% 10-year survival of soft tissue level SLA surface implants (Straumann). However, a review6 reported a mean implant survival rate of 94.6% after at least 10 years. A possible reason for this difference may be the strict case selection criteria and protocol used for undergraduate students at the dental school. Since 2015, the protocol for acceptance of patients to the University of Alberta undergraduate implant program has been as follows.
- Review medical/dental history.
- Complete general consent and implant consent forms.
- Complete dental examination and have findings reviewed by the attending instructor.
- Obtain intra-oral and extra-oral photos.
- Take impressions for un-mounted diagnostic casts.
- Obtain cone beam computed tomography (CBCT) and oral radiologist’s interpretation.
- Perform wax-up on the diagnostic casts of the implant site. Digitally scan the cast and combine the STL (stereolithography) file with the DICOM (digital imaging and communications in medicine) CBCT file with implant-planning software.
- Plan treatment using information from the intra-oral examination, photographs, diagnostic casts, CBCT information and implant planning software.
- Develop a presentation, using a defined format, to present the diagnostic information and treatment plan.
- Present the treatment plan to the oral surgeon and prosthodontist involved in the program. The oral surgeon will review the CBCT again with the student.
- The oral surgeon and prosthodontist will review the treatment plan for acceptance or rejection, depending on factors, such as medical history, complexity of the implant treatment and complexity of adjunctive restorative needs of the patient.
Furthermore, certified specialists were present in the operating room in all cases, teaching the students and supervising all aspects of restorative treatment and maintenance. The protocol used between 2007 and 2015 was the same as the 2015 protocol; however, only plain films without CBCT imaging were used and PowerPoint (Microsoft, Redmond, Wash.) was not used to review cases. An example of a dental student case presentation is shown in Figures 1(a) to 1(g).
Another factor potentially influencing the high survival rate of implants placed at the University of Alberta is the maintenance and care that is a large part of the clinic. The dental school operates undergraduate clinics supervised by general dentists, prosthodontists, oral and maxillofacial surgeons and registered dental hygienists following guidelines similar to those reviewed by Todescan et al.9 to monitor the overall success of dental implants and prostheses. Recall assessments consist of updating medical and dental histories, examination of soft tissue including plaque index, probing depths, bleeding on probing, mobility, occlusion, interproximal contacts, as well as bone level based on periapical radiographs. The patient then undergoes full-mouth scaling and root planing conducted by dental hygiene students. Furthermore, home care is strongly emphasized. As the presence or absence of plaque is related to peri-implantitis,10 patients are educated in techniques and tools to remove plaque; electric tooth brushes, proper flossing techniques, mouthwash and water flossers are recommended home care aids.
Although not a main objective of our research project, we compared the dental implant education experience at the University of Alberta with that at other dental schools. A 2006 review of undergraduate dental implant education at universities in the United States5 reported that 97% included implant dentistry in the undergraduate curriculum. As at the University of Alberta’s Dental Implant Clinic, “teaching the implant curricula is a multidisciplinary effort” with the “prosthodontic faculty often cover[ing] case selection, treatment planning, and restoration of implants; the topics of surgical implant placement... are presented by the faculty of oral and maxillofacial surgery.”
The University of Alberta currently teaches implant dentistry in a classroom setting with 14 h of lectures in third-year and 2 h in fourth-year dental school, 7 h in a simulation lab on models used to train students by simulating conditions they will encounter in practice (dentoforms) and 12 h of clinic in both third and fourth years with patients, either restoring or placing dental implants. This compares with a 2017 survey11 of North American dental curricula where average didactic implant education included 17 h lecture, 3 h problem-based learning, 3 h self-study and 11 h of other activities. According to this survey, 89% of dental schools had students participate in implant surgery in some form, whereas only 3 out of the 47 responding schools reported that students actually perform implant surgery. At the University of Alberta, every fourth-year dental student is given the opportunity to place a dental implant. In general, exit surveys of graduating dental students at the University of Alberta have found that dental implants have been an area that students enjoy learning about, and they would like to pursue further training after graduation.
In conclusion, we found a 99.7% survival rate after an average of 709.1 days (7–2677 days) for dental implants placed by undergraduate dental students. The University of Alberta dental school implant clinic is supervised by certified specialists with strict case selection criteria and maintenance and care protocols that could contribute to the high survival rate. Therefore, we are not suggesting that new dentists trained in dental implants at a dental school would have a similar survival rate entering private practice. The University of Alberta offers a unique experience of both surgical and prosthodontic aspects of dental implants that students enjoy and find to be a valuable part of their dental education.
Conclusion
Geriatric oral health care is an important part of the curriculum of most dental and dental hygiene programs in our study. However, not all are providing students with clinical training opportunities with LTC residents. Meeting the oral health needs of this population requires urgent attention and care from dental and dental hygiene professionals. Barriers to providing didactic and clinical opportunities to students include a lack of teaching staff, lack of funding, time constraints and lack of access to geriatric populations. Oral health educational institutions must ensure that they are embedding evidence-based gerodontology in their curricula to reflect the oral and overall health needs of today’s aging population. Dental and dental hygiene schools should supplement their curricula to include geriatrics for all students.
Figure 1: Standard implant case work-up at the University of Alberta’s student dental clinic.
The patient was a healthy (American Society of Anesthesiologists status 1), 36-year-old female with a chief complaint of “missing teeth.” She had received routine dental care and had overall healthy dentition and periodontium. Tooth 14 was extracted 12 years earlier because of caries.
Cone beam computed tomography (CBCT) indicated 10–11 mm of bone height at the site of tooth 14 (a). A complete set of clinical photographs was taken (b); alginate impressions (c) and a diagnostic wax-up were followed by digital planning by the student. The case was presented by the student and reviewed by both a prosthodontist and an oral and maxillofacial surgeon. The patient was accepted.
The student’s plan (d) included a 5.0-mm implant, which was poorly aligned. The final implant position and size were determined during review with the oral surgeon, and a 4.3-mm implant was chosen, along with more palatal positioning allowing for adequate buccal bone.
In January 2015, stage 1 surgery was performed, using a 4.3 × 10 mm Nobel Replace Tapered Groovy implant; no complications were noted during or after the procedure. In September 2015, stage 2 surgery was performed without complications. In November 2015, the final prosthesis was inserted. During the first year post-implant, some early bone loss occurred, but radiography at the 2-year follow-up examination showed it had stabilized. This is an expected finding8 and is not considered pathologic, but rather normal bone remodeling.12

1(a) Pre-operative panorex image.

1(b) Pre-operative clinical photo, occlusal view.

1(c) Pre-operative diagnostic cast.
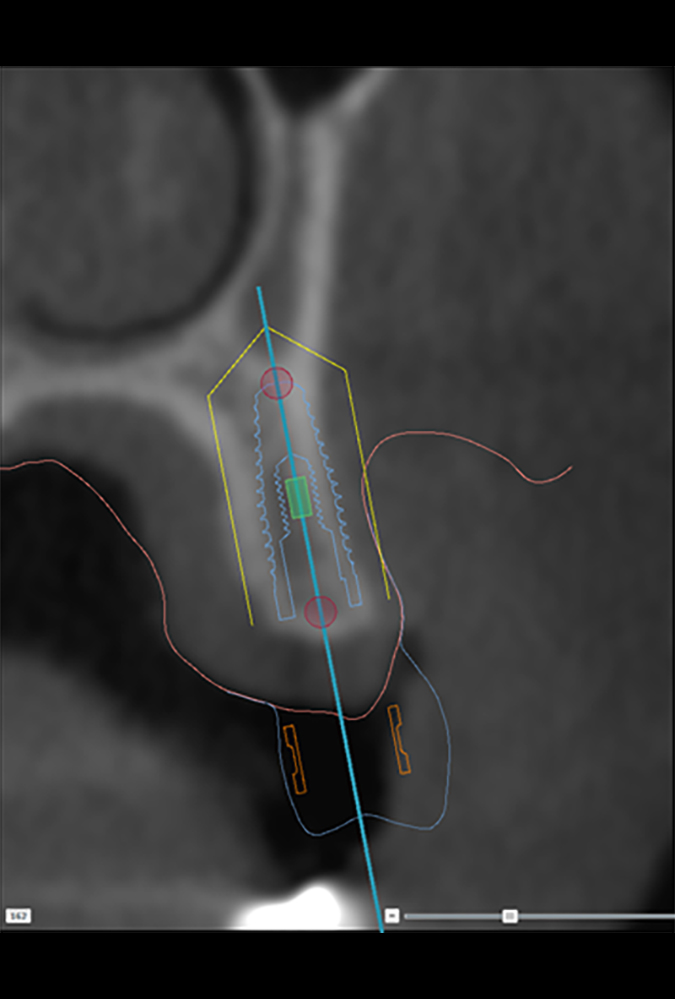
1(d) Implant planning by student using computer software.

1(e) Peri-apical radiograph after implant.

1(f) Post-implant photograph.
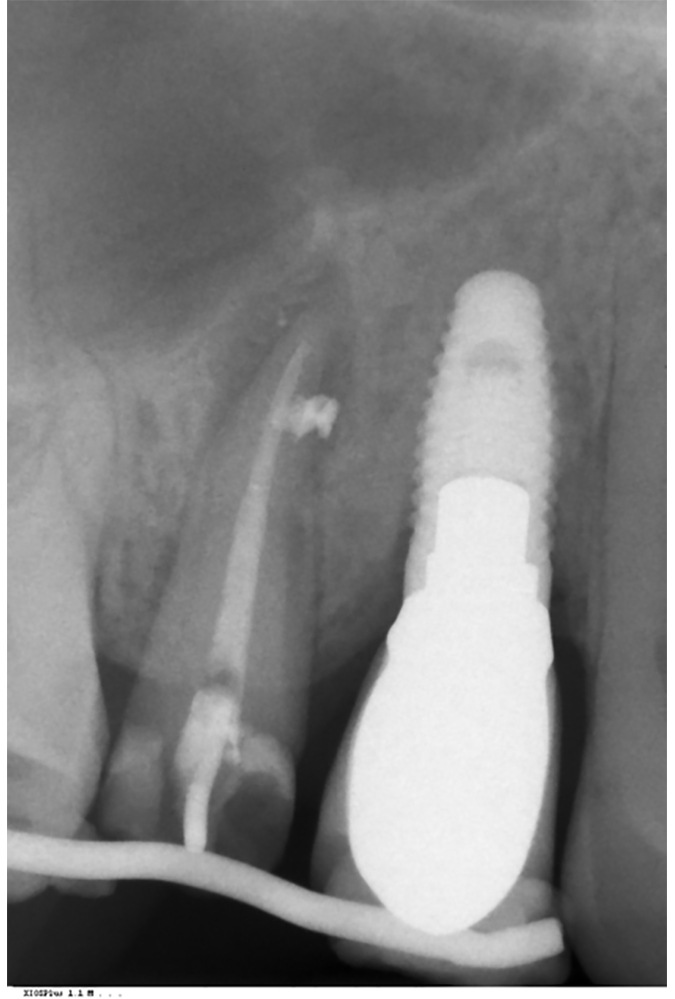
1(g) Follow-up radiograph taken 4 years post-implant.
THE AUTHORS
Correspondence to: Dr. Bernard Linke, 5509 Edmonton Clinic Health Academy, 11405 — 87 Avenue, Edmonton AB T6G 1C9. Email: blinke@ualberta.ca
This article has been peer reviewed.
The authors have no declared financial interests in any company manufacturing the types of products mentioned in this article.
References
- Donos N, Calciolari E. Dental implants in patients affected by systemic diseases. Br Dent J. 2014;217(8):425-30.
- Levin L, Halperin-Sternfeld M. Tooth preservation or implant placement: a systematic review of long-term tooth and implant survival rates. J Am Dent Assoc. 2013; 144(10):1119-33.
- van Velzen FJ, Ofec R, Schulten EA, Ten Bruggenkate CM. 10-year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res. 2015;26(10):1121-8.
- Kronstrom M, McGrath L, Chaytor D. Implant dentistry in the undergraduate dental education program at Dalhousie University. Part 1: Clinical outcomes. Int J Prosthodont. 2008; 21(2):124-8.
- Kroeplin BS, Strub JR. Implant dentistry curriculum in undergraduate education: part 1 — a literature review. Int J Prosthodont. 2011;24(3):221-34.
- Moraschini V, Poubel LA, Ferreira VF, Barboza E dos S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44(3):377-88.
- Guo Q, Lalji R, Le AV, Judge RB, Bailey D, Thomson W, Escobar K. Survival rates and complication types for single implants provided at the Melbourne Dental School. Aust Dent J. 2015;60(3):353-61.
- Pettersson P, Sennerby L. A 5‐year retrospective study on Replace Select Tapered dental implants. Clin Implant Dent Relat Res. 2015;17(2):286-95.
- Todescan S, Lavigne S, Kelekis-Cholakis A. Guidance for the maintenance care of dental implants: clinical review. J Can Dent Assoc. 2012; 78:c107.
- Serino G, Ström C. Peri-implantitis in partially edentulous patients: association with inadequate plaque control. Clin Oral Implants Res. 2009;20(2):169-74.
- Kihara H, Sun J, Sakai M, Nagai S, Da Silva J. A survey of dental implant instruction in predoctoral dental curricula in North America. J Dent Educ. 2017;81(9):1085-90.
- Albrektsson T, Chrcanovic B, Ostman PO, Sennerby L. Initial and long-term crestal bone responses to modern dental implants. Periodontol 2000. 2017;73(1):41-50.



